1. Background
Candida albicans is considered as part of the normal flora of the mouth, which doesn’t cause disease but under unfavorable local conditions, such as poor oral hygiene (1), wearing of denture (2) and general predisposing factors such as high carbohydrate diet, smoking (3), diabetes (4) malnutrition, leukemia, chemotherapy, genetic disorders (5), long term antibiotic therapy (6), corticosteroid therapy (7), senility (8), radiotherapy (9) and cancer (10)can cause candidiasis. Using mouthwashes is a common way to controlling the C. albicans population in the mouth, which are used widely in dentistry (11, 12). Mouthwashes have been recommended for the prevention and control of oral diseases, especially for the control of oral microorganisms (13). They usually contain water and some active components such as antibiotics, antifungal and anti-inflammatory substances. Some mouthwashes have been found to enhance the removal process and elimination of microorganisms (14).
Nowadays, different types of medicine have been used for the treatment of oral problems. Most of them are chemical and have many side effects; consequently researchers are interested in herbal remedies for medication and aim to substitute herbal material instead of chemical formula with limited side effects for human beings (15). Different mouthwashes are available in the Iranian market but there is no information about their efficiency differences. Among different herbal and chemical mouthwashes, which are available in the Iranian market (Table 1), chlorhexidine and persicac have been more considered. Chlorhexidine was introduced as an antiseptic agent with activity against different organisms such as bacteria, viruses and different types of fungi including C. albicans, which causes oral candidiasis (16). Different studies on chlorhexidine have demonstrated its potential to prevent oral complications, such as the occurrence of chronic or opportunistic infections (17).
In order to overcome the effects of chemical drugs, the World Health Organization (WHO) has advised researchers to investigate the possible use of natural products such as herb and plant extracts (18). One of the agents considered as an alternative to chlorhexidine is a plant called Salvadora persica or “Miswak”. S. persica herbal mouthwash contains three medicinal plants, S. persica, Yarrow and Mint. Furthermore, WHO encourages the use of chewing S. persica sticks (Miswak) as an effective oral hygiene procedure (19, 20). S. persica, a very popular plant in the Middle East, contains a number of identified antimicrobial and other prophylactic components including volatile oils, flavonoids, alkaloids, steroids, terpenoids, saponins and carbohydrates (18, 21).
Currently, a herbal drug is defined as a remedy derived from plants (roots, leaves, flowers, fruits, seeds) and other natural sources which can be used for therapeutic purposes and its active chemical constituents provide the basis for pharmaceutical synthesis (21). Different studies have indicated that, using a mouthwash in patients with systemic infection could decrease fungal and bacterial colonization in the mouth cavity. McCourtie et al. (22) investigated the effect of chlorohexidinegluconate on Candida adhesion to acrylic denture and concluded that fungal colonization decreases by using chlorohexidine. A study by Pizzo et al. (23) indicated a considerable decrease in the colonization of adhesive Candida to epithelial cells in individuals using chlorohexidine. Nayak et al. (24) investigated the effect of chlorohexidine on dental plaque and concluded that chlorohexidine is an effective agent in decreasing dental plaque and colonization of microorganisms in plaque.
Among mouthwashes, most researches have focused on chlorhexidine against C. albicans and there is a lack of complete information about other mouthwashes especially herbal ones. The current study tried to evaluate the effect of the anticandidial activity of different mouthwashes, which are used in the Iranian market and attempted to find the most effective mouthwash for patients who are susceptible for candidiasis.
2. Objectives
The purpose of the current research was to compare the effect of chemical and herbal mouthwashes on C. albicans.
3. Materials and Methods
3.1. Strain of C. albicans
In this study, a standard strain of C. albicans was used, NO. PTCC 5027.The standard strain was cultivated in Sabouraud dextrose agar, SDA (Merck, Germany) and placed at 30 ºC for 24 hours until activated.
3.2. Mouthwashes
Different types of mouthwashes were used for this study. Chemical mouthwashes such as Vi-one (Rojn Cosmetic Lab Co, Tabriz, Iran), Fluorine (World Health Laboratories Co, Tehran, Iran), Hexodine (World Health Laboratories Co, Tehran, Iran), Oral B (Grossgerau Co, Hessen, German), Sensodyne (GSK Co, London, UK), Foramen (Guarnizo Co, Cantabria, Spain), Epimax (Emad Pharmaceutical Co, Esfahan, Iran), Chlorohexidine (Shahre Daru Laboratories Co, Tehran, Iran), Fluoride (Shahre Daru Laboratories Co, Tehran, Iran), anti-septic Irsha (Shafa Cosmetic Laboratories Co, Tehran, Iran), anti-plaque Irsha (Shafa Cosmetic Laboratories Co, Tehran, Iran ), Benzydamine (Behvazan Co, Rasht, Iran), Colgate (Kucukyali Co, Estanbol, Turkey), and herbal mouthwashes such as Matrica (Barij Essence Pharmaceutical Co, Kashan, Iran), S. persica (Porsina Pharmaceutical Co, Tehran, Iran), and Corpore Sano (Disna. SA Co, Barcelona, Spain) were used. The compositions of all of the mouthwashes are provided in Table 1.
| Name | Batch No. | Manufacture Date | Expiry Date | Ingredients as Listed on Packages |
|---|---|---|---|---|
| Oral B | KT 13 | October 2010 | August 2013 | Aqua, glycerin, polysorbate 20, aroma, methylparaben, cetylpyridinium, chloride, sodium fluoride, sodium benzoate, propylparaben, CI42051, CI 47005. |
| Sensodyne | 1241033 | August 2011 | August 2013 | Sodium flouride. |
| Vi-one | 2231 | July 2012 | July 2014 | Deionized water, sorbitol,glycerine, ploxamer 407, polyethylene glycol, perment ethanol, menthol, sodium methyl paraben, aspartame, sodium propyl paraben, citric acid, sodium fluoride 0.05%, cetylpyridinium chloride 0.05%, CIN 42090. |
| Fluorine | 90-F1-O1 | April 2011 | April 2013 | Sodium flouride, cetylpyridinium chloride, zinc ions, glycerin, sorbitol, sodium fluoride. |
| Hexodine | C1-03 | July 2012 | July 2014 | Aqua, glycerin, CI 42090. |
| Epimax | 2011 EPM-11 | December 2011 | December 2013 | Sorbitol, propylene glycol, tetra sodium pyrophosphate, citric acid, polysorbate 20, polysorbate60, chlorhexidinedigluconate, sorbic acid, menthol, sodium fluoride, sodium saccharine, dye. |
| Chlorhexidine | CL-06 | March 2012 | March 2014 | Sorbitol. flavour, PEG 40 hydrogenated castor oil, alcohol, CI 16035. |
| Anti-Plaque Irsha | 9058 | December 2011 | December 2014 | Alcohol, glycerin, synperonic, TSPP, SLS, benzoic acid, allantoin, PVM/MA, benzoate, fluoride 0.05%, saccharin, CI 42090, CI 19140. |
| Anti-Septic Irsha | 9022 | February 2012 | February 2015 | Alcohol, synperonic, benzoic acid, benzoate, okaliptol, tymol, methy salicylate, mentol, aqua. |
| Benzydamine | BH. 89.16 | December 2010 | December 2013 | Hydrochloride 0.15%. |
| Colgate | 2069 CHG11B | August 2010 | August 2013 | Aqua, glycerin, alcohol, sorbitol, propylene glycol, polysorbate20, sodium benzoate, aroma, PVM/MA copolymer, zinc citrate, CI 42090, sodium fluoride, tetrasodium pyrophosphate, tetrapotassium pyrophosphate, sodium saccharin. |
| Fluoride | 14 | December 2011 | December 2014 | Sodium fluoride 0.2%. |
| Foramen | Ref.015 | February 2012 | February 2016 | Sodium fluoride 0.05%, triclosan, aqua, sorbitol, glycerin, PEG-40, castoroil, aroma, cinnamal, sodium propyl paraben,sodium benzoate, sodium saccharin, CI 42090. |
| M.chamomilla | 310038 | December 2011 | December 2013 | Matricaria chamomilla |
| S. persica | 09 | September 2011 | September 2013 | Salvadora persica, Mentha spicata, Achilleamille folium. |
| Corpore Sano | G0019 | March 2012 | March 2014 | Aqua, alcohol, PEG-40, hydrogenated castor oil, aroma, geraniol, sodium benzoate, sodium saccharin, Propolis extract, ethylparaben, propylparaben, methanol, citric acids, CI 19140, CI 42090. |
3.3. Agar Diffusion
A suspension was made by physiological saline (Samen, Iran) and fresh culture of C. albicans (24 hours) and the OD (with turbidity equating to a McFarland standard of 0.5) was read at 530 nm wave length by a spectrophotometer (Pars Teb Novin, Iran), in which there were 2.5×106 CFU/mL colonies in each milliliter (optical density at 530 nm, 0.12). Next, 10 µL of the suspension was transferred to SDA medium and two wells were made with suitable distance in culture medium, filling with mouthwashes. To decrease error, the test was repeated 4 times. Plates were placed in the incubator (Behdad Medical Production, Iran) at 30 ºC for 24 hours (25). Inhibition zone was measured and recorded using a Collis (Kiya Sanat Khavaran, Iran) (26). For each mouthwash, one control plate containing mouthwash and sterilized distilled water was prepared.
3.4. MIC Measurement
To determine the minimum inhibitory concentration for each mouthwash, a serial dilution was prepared according to the CLSI protocol (27). The lowest concentration of mouthwash that prevented turbidity (growth) of C. albicans was considered as the minimum inhibitory concentration. This method was conducted based on turbidity clearance.
3.5. Minimum Fungicidal Concentration (MFC) Measurement
To determine the minimum fungicidal concentration of fungus, 10 µL of specimens were taken from the MIC (last clear tube) and two last tubes were poured in SDA, incubating at 30 ºC for 24 hours. The lowest concentration of mouthwash that prevented the growth of C. albicans determined by sub-culturing of the last clear MIC tube on SDA and refers to fungicidal activity. This procedure was conducted to allow more accuracy and control error. Colony counts of less than four, indicated no growth while more than four indicated growth (27).
3.6. Statistical Analysis
The data were analyzed with the SPSS software (18th edition), using independent T-test and one-sided variance analysis (one way ANOVA) with P < 0.05.
4. Results
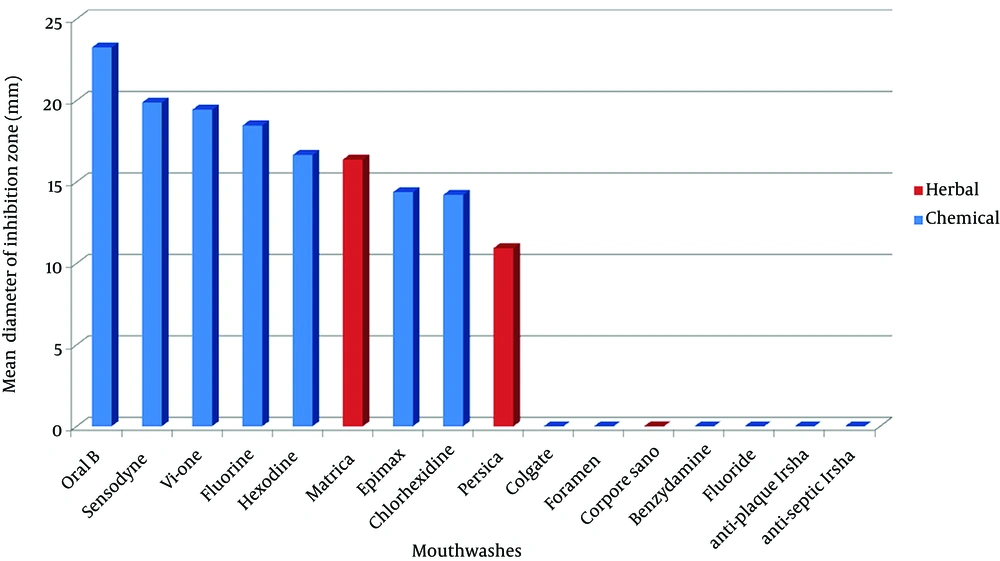
The mean diameter of inhibition zone by herbal and chemical mouthwashes has been indicated in Tables 2 and 3. The comparison of inhibition zone diameter by using chemical and herbal mouthwashes has been indicated in Figure 1. Oral B and S. persica, mouthwashes showed the highest and lowest anti-candidial activity against C. albicans in SDA, according to the inhibition zone diameter.
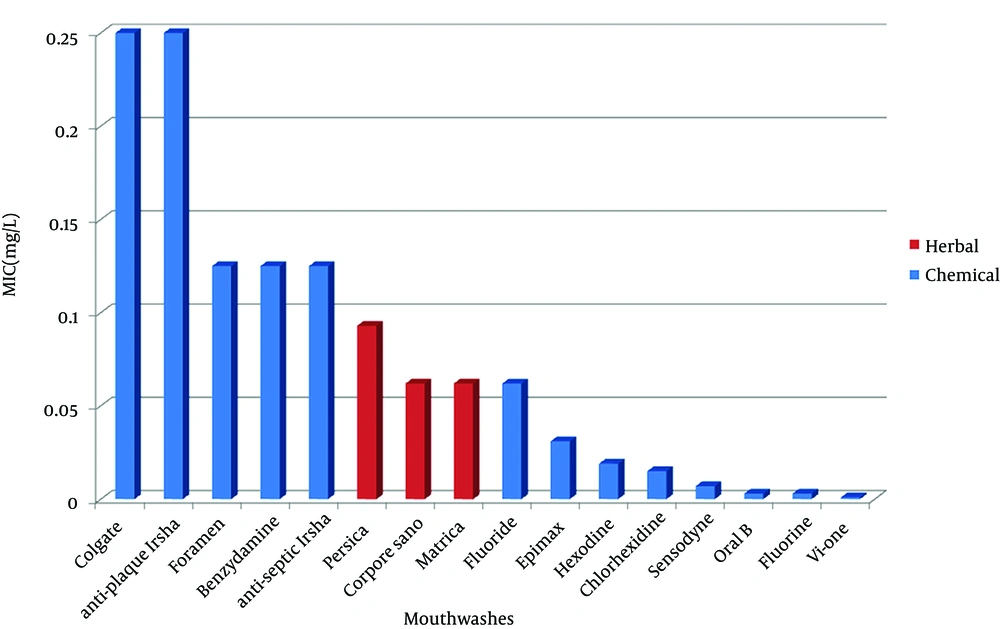
Amount of MIC was determined by the tube dilution test, with 10 dilution tubes. The point at which growth of C. albicans was inhibited was recognized as the minimum inhibitory concentration. Statistical analysis of the MIC and MFC amounts of chemical and herbal mouthwashes are shown in Tables 4 and 5. Comparison of the amounts of MIC and MFC by using chemical and herbal mouthwashes are indicated in Figure 2. Colgate and anti-plaque Irsha mouthwashes showed the highest amount of MIC and MFC against C. albicans (Figure 3) and Vi-one mouthwash showed the lowest amount of MIC and MFC (Figure 4). The results of the MFC were similar to MIC (Tables 4 and 5).
| Types of Mouthwashes | Mean (mm) | SD (mm) | P value From One Way ANONA Test | Control P value |
|---|---|---|---|---|
| Oral B | 23.25 | 0.65 | ||
| Sensodyne | 19.87 | 1.32 | ||
| Vi-one | 19.43 | 0.81 | ||
| Fluorine | 18.46 | 1.84 | ||
| Hexodine | 16.65 | 0.85 | ||
| Epimax | 14.37 | 0.79 | P<0.001 | P<0.05 |
| Chlorhexidine | 14.21 | 0.45 | ||
| Anti-Plaque Irsha | R | R | ||
| Anti-Septic Irsha | R | R | ||
| Benzydamine | R | R | ||
| Colgate | R | R | ||
| Fluoride | R | R | ||
| Foramen | R | R |
a R. means C. albicans resistance to these mouthwashes.
b The units of mean and standard deviation of inhibition zone are in millimeter (mm).
| Types of Mouthwashes | Mean (mm) | SD (mm) | P value From One Way ANONA Test | Control P value |
|---|---|---|---|---|
| M.chamomilla | 16.37 | 0.74 | ||
| S. persica | 10.93 | 0.77 | P < 0.001 | P < 0.05 |
| Corporesano | R | R |
a R. means C. albicans resistance to these mouthwashes.
b The units of mean and standard deviation of inhibition zone are in millimeters (mm).
| Types of Mouthwashes | MIC and MFC (mg/L) | P value From One Way ANONA Test | Control P value |
|---|---|---|---|
| Anti-Plaque Irsha | 0.250 | ||
| Colgate | 0.250 | ||
| Anti-Septic Irsha | 0.125 | ||
| Benzydamine | 0.125 | ||
| Foramen | 0.062 | ||
| Fluoride | 0.062 | P < 0.001 | P < 0.05 |
| Epimax | 0.031 | ||
| Hexodine | 0.019 | ||
| Chlorhexidine | 0.015 | ||
| Fluorine | 0.007 | ||
| Sensodyne | 0.007 | ||
| Oral B | 0.003 | ||
| Vi-one | 0.001 |
aThe unit of MIC is in mg/L.
| Types of Mouthwashes | MIC and MFC (mg/L) | P value From One Way ANONA Test | Control P value |
|---|---|---|---|
| S. persica | 0.093 | ||
| M. chamomillaMatrica | 0.062 | P = 0.465 | P < 0.05 |
| Corporesano | 0.062 |
aThe unit of MIC is in mg/L.
5. Discussion
The use of antiseptic mouthwashes as a component of a complete oral hygiene regimen. Mouthwashes are a convenient and accepted method of oral hygiene (28). In the current study, C. albicans indicated the most and the least sensitivity to Oral B and S. persica, respectively. Among different mouthwashes, C. albicans was resistant against fluoride, benzydamine, Colgate, Foramen, anti-septic Irsha and anti-plaque Irsha.
Giuliana et al. (29) investigated the in vitro antifungal effect of mouthwashes containing antimicrobial factor against Candida species and indicated that, chlorohexidine has antifungal properties and is effective against C. albicans. Also, in the current study, chlorohexidine was indicated to be effective against C. albicans, but in comparison with other mouthwashes, it showed a lower effect. Bajaj and Tandon (30) evaluated the effect of chlorohexidine on dental plaque, gum inflammation and microbial growth and indicated that microbial growth was decreased after the application of this substance. The current study investigated the effect of chlorohexidine against C. albicans and indicated that it has a lower effect in comparison with other mouthwashes, especially Oral B.
Meiller et al. (31) investigated the antifungal effect of 0.2% chlorohexidine against C. albicans. There is less information about chlorohexidine and its effect on C. albicans in comparison with the other mouthwashes. Chlorhexidine (CHX) is the most active agent, due to its wide spectrum of antimicrobial activity against a wide variety of organisms, including C. albicans (17). The mode of action of this substance is not entirely understood, but it is known that it acts as a fungicide and has a fungistatic function, leading to the coagulation of nucleoproteins and changes in cell walls allowing the possible escape of cytoplasmic components through the plasmalemma (17, 32). However, for oral use as a mouthwash, chlorhexidine has been reported to have a number of side effects, such as unpleasant taste, staining of teeth and tongue, gingival desquamation, taste disturbance and painful mucosa (18, 33). Chlorhexidine is not the first choice of drug for the treatment of Candida infections. However, the increase in the number of opportunistic infections caused by fungi, mainly in HIV infected individuals, and the great number of strains that have become resistant to the common antifungals has encouraged new research in relation to alternative treatments of such infections, among which is the use of chlorhexidine (32).
Among herbal mouthwashes examined by the agar diffusion method, Matrica and S. persica had the most and the least effect on C. albicans, respectively and Corpore Sano didn’t have any effect on C. albicans. Almas (34) investigated the antibacterial effect of S. persica extract (50%) in Persica mouthwash and chlorohexidine against oral microbes and C. albicans and concluded that, chlorohexidine mouthwash has more antimicrobial effect in comparison with extract of toothbrush plant and Persica has less antibacterial activity in comparison with chlorohexidine. It is important to note that Persica couldn’t change the oral microbial and C. albicans level. In the current study, the results were similar to previous studies and Persica indicated less activity than chlorohexidine and Matrica against C. albicans with an average inhibition zone diameter of 10.93 mm and there was a significant difference between Persica and chlorohexidine anticandidial activity as indicated by the Tukey-HSD test (P < 0.001).
Alali and Al-Lafi (35) reported that there is considerable amounts of antibacterial agent in Persica leaves, which has activity against all types of oral bacteria and is comparable with different types of antiseptics. In the current study, Persica indicated mild anticandidial activity. Several studies have been conducted on Persica compounds and there isn’t enough information about other mouthwashes. Based on our findings, there was no significant difference between herbal and chemical mouthwashes using independent T-test (P = 0.764). Using the agar diffusion method and according to the one-way ANOVA test, there was a significant difference within the group of chemical and herbal mouthwashes (P < 0.001). In the group of chemical mouthwashes, Oral B indicated a significant difference with other mouthwashes and in the group of herbal mouthwashes Matrica indicated a significant difference with other mouthwashes as indicated by the Tukey-HSD test (P < 0.001).
Investigation of minimum inhibitory concentration and minimum fungicidal concentration in the group of chemical mouthwashes, revealed that Colgate and anti-plaque Irsha had the least and Vi-one had the most activity with an average concentration of 0.250 mg/L and 0.001 mg/L, respectively. In the group of herbal mouthwashes, also S. persica had the least activity (0.093 mg/L) and Matrica and Corpore Sano had the most activity (0.006 mg/L). The MIC and MFC results were the same and all mouthwashes had a minimum fungicidal concentration at the same level as the minimum inhibitory concentration. There was no significant difference between chemical and herbal mouthwashes using independent T-test (P = 0.879). al-Bagieh et al. (36) evaluated the antifungal activity of Persica extract and concluded that Persica concentrations more than 15% has a fungistatic effect on C. albicans.
In the current study, Persica a concentration of 0.093 mg/L indicated fungistatic activity against C. albicans. Guggenheim and Meier (37) indicated that, chlorohexidine could significantly decrease the number of microorganisms in biofilm. In the current study chlorohexidine effectively decreased candidial growth (MIC 0.015 mg/L). Using the MIC and MFC methods and according to the one-way ANOVA test, there was a significant difference within the group of chemical mouthwashes (P < 0.001) and there was no significant difference within the group of herbal mouthwashes (P = 0.465).
In conclusion, as our study showed, among chemical and herbal mouthwashes, Oral B is a better chemical mouthwash. These mouthwashes can be used for infection treatment, rather than antibiotics, to decrease antibiotic resistance. Furthermore, clinical studies are needed to confirm the efficiency of in vivo application.