1. Background
Stenotrophomonas maltophilia is a readily available commensal of importance (1), found in water, soil, sewage and frequently on plant or within plant rhizosphere (2). They are commensals known for multitudinous applications in biotechnology (3). The bacteria explore the depression of immune systems to cause infection (4-6), though they have also been implicated in infection of immunocompetent subjects (7-9). They are therefore important considering their infectivity and the morbidity they initiate (10, 11), which range from nosocomial to community acquired infections. They cause a wide range of human systemic infections (12, 13) after entering through the respiratory pathway (4, 14).
Falagas et al. (15) reported a high mortality rate of 37.5% from S. maltophilia infections. Multidrug resistance by S. maltophilia has been well documented (16-19), raising the mortality rate in some areas to as high as 44.4% (20). Although the drug of choice for S. maltophilia infections is the sulfonamides (21), especially the synergistic form (cotrimoxazole or trimethoprim-sulfamethoxazole), resistance to these antibiotics is rampant around the world among human and nonhuman animals (22-24) and is mediated by the sulphonamide resistance (sul) gene. Sul3, being the newest sulphonamide gene, has been fingered as the possible reason for new rise in sulphonamide resistance world-wide (25). Sul2 has also been the most widely reported gene in animals (26-30) and can be used to trace the sulphonamide resistance genes in other sources originated from animal farms.
2. Objectives
Grasses and butternuts are eaten raw by animals and human, respectively. The latter is eaten as squash salad by human (31). Therefore, the safety of consumers is hinged on the type of bacterial flora associated with the plants and their susceptibility to antibiotics when they infect consumers. This in turn depends on the pool of genes in the rhizosphere of plants, as resistance gene(s) may become disseminated to the indigenous bacterial community form one organism, and ultimately contribute to the clinical problems of antibiotic resistant pathogens. Therefore, the aim of this study was to assess the S. maltophilia isolates from plants rhizosphere in the Nkonkobe Municipality, Eastern Cape Province, South Africa, for their antibiogram characteristics and the presence of antibiotic resistance genes, sul2 and sul3, in their genomes.
3. Materials and Methods
3.1. Study Location and Samples Collection
This study was conducted within the Nkonkobe Municipality of the Eastern Cape Province, South Africa. The Municipality is situated in the Amathole District Municipality, bordering the Nxuba Municipality to the west and the Amahlathi Municipality to the east. The municipality has a predominantly rural population and has a total of 21 wards. About 80% of the population of Nkonkobe resides in rural settlements. Soil butternut and grass roots in Alice Town environment were carefully uprooted and aseptically cut with sterile scissors into sterile containers and transported in ice to the laboratory for bacteria isolation.
3.2. Isolation of Test Bacteria
Isolation of the bacteria from root rhizospheres was performed following the methods of Bollet et al. (32) with slight modifications. About 1 g of the plant root sections were collected and inoculated into 10 mL of nutrient broth (bio-Merieux, Marcy-l’Etoile, France), supplemented with 0.5 mg of DL-methionine (Sigma Chemicals, South Africa) per mL. After 24 hours of incubation at 37°C, 0.1 mL was inoculated unto Mueller Hinton agar, spread to dry using a glass spreader, and allowed to stand for 15 minutes. Thereafter, four discs of 10 µg imipenem (MAST Diagnostics, Merseyside, UK) were aseptically placed on the surface of the inoculated agar. After 18 hours of incubations at 37°C, colonies that grew around the disc were subcultured for purity and subjected to preliminary identification.
3.3. Preliminary Identification of the Presumptive Stenotrophomonas Isolates
The purified isolates were Gram stained and observed under a light microscope. The Gram negative isolates were subjected to oxidase test and the oxidase negative isolates were subjected to preliminary speciation using analytic profile index 20E (API 20 E, BioMerieux, South Africa). In addition, carbon assimilation tests and other biochemical tests were carried out in the identification process. Stenotrophomonas genus positive isolates were then selected for specie confirmation.
3.4. Polymerase Chain Reaction confirmation of Stenotrophomonas maltophilia Isolates
Differentiation of S. maltophilia isolates amongst the genus isolates identified above was carried out using specie-specific polymerase chain reaction (PCR), using the primer sets SM1 (5'-CAGCCTGCGAAAAGTA-3') and SM2 (5'-TTAAGCTTGCCACGAACAG-3') (Inqaba Biotech., South Africa) (32). The PCR condition was as follows: an initial denaturation of 95°C for 5 minutes, a subsequent 30-cycle amplification including annealing at 58°C for 10 seconds, extension at 72°C for 60 seconds, and denaturation at 95°C for 10 seconds. For the last cycle, the extension step was two minutes (33). S. maltophilia DSM 50170 (ATCC 13637, type strain t20, Berlin, Germany) was used as the control.
3.5. Phenotypic Antibiotic Susceptibility Test
The disc diffusion technique was employed to determine the antibiotic susceptibility pattern of the isolates. The test antibiotics included meropenem, cefuroxime, ampicillin, ceftazidime, cefepime, minocycline, kanamycin, ofloxacin, levofloxacin, moxifloxacin, ciprofloxacin, gatifloxacin, polymyxin B, cotrimoxazole, trimethoprim, aztreonam and polymyxin B. S. maltophilia 50170 was used as the positive control, and the antibiogram was performed in accordance with standards described by the National Committee for Clinical Laboratory Standards (34) and Cheesebrough (35).
3.6. Multiple Antibiotic Resistance Index
The multiple antibiotic resistance index (MARI) was calculated as the ratio of the number of antibiotics to which resistance occurred by the isolates (a) to the total number of antibiotics to which the isolates were exposed (b), ie, MARI = a/b (36).
3.7. Assessment of Trimethoprim-Sulfamethoxazole Resistance Genes
Trimethoprim-sulfamethoxazole is the drug of choice in the treatment of infections caused by S. maltophilia. This, along with our initial observation of resistance to this antibiotic, informed the need for assessment of the presence of sul2 and sul3 genes in the resistant isolates, which were performed in accordance with the descriptions of Blahna et al. (26) using the primers (Inqaba Biotech., South Africa) listed in Table 1. The PCR condition for sul2 detection began with an enzyme activation (denaturation) stage at 94°C for five minutes, followed by 30 cycles of denaturation at 94°C for 40 seconds, annealing at 55°C for 40 seconds and extension at 72°C for 1 minute. A final extension at 72°C was run for seven minutes. For sul3 detection, the PCR condition was as follows: heating at 94°C for five minutes, 30 cycles at 94°C for 60 seconds, 55°C for 60 seconds and 72°C for 60 seconds, followed by one cycle at 72°C for seven minutes (26).
| Primers | Primer Sequence | Size |
|---|---|---|
| Sul2 F | 5′-GCGCTCAAGGCAGATGGCATT-3′ | 285 |
| Sul2 R | 5′-GCGTTTGATACCGGCACCCGT-3′ | 285 |
| Sul3 F | 5′- GAGCAAGATTTTTGGAATCG -3′ | 799 |
| Sul3 R | 5′- CATCTGCAGCTAACCTAGGGCTTTGGA -3′ | 799 |
4. Results
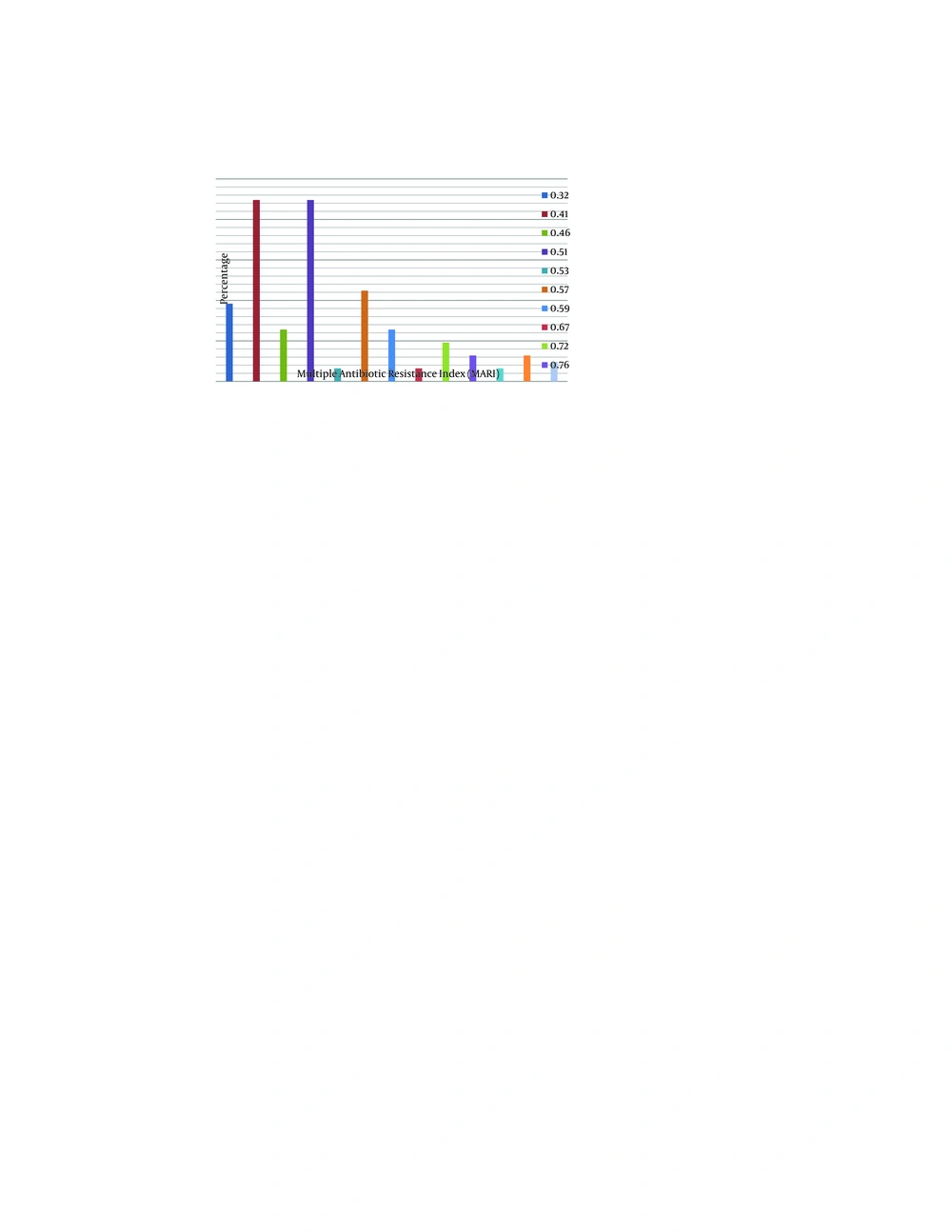
One hundred and twenty (96%) S. maltophilia isolates were recovered from grass root rhizosphere, while 5 (4%) were recovered from soil butternut rhizosphere (Table 2). About 8.9% of the isolates were resistant to meropenem, while resistance to the other antibiotics was as follows: cefuroxime 95.6%, ampicillin-sulbactam 53.9%, ceftazidime 10.7%, cefepime 29.3 %, minocycline 2.2%, kanamycin 56.9%, ofloxacin 2.9%, levofloxacin 3%, moxifloxacin (2.8%), ciprofloxacin 24.3%, gatifloxacin 1.3%, polymyxin B 2.9% and aztreonam 58% (Table 3). Variable susceptibilities to the cephalosporins (with carbapenem) were observed. About 88% of the isolates were susceptible to meropenem and ceftazidime, while 58.7% were susceptible to cefepime. In addition, 97.8% and 97.1% of the isolates were susceptible to minocycline and polymycin B, respectively. With regards to the fluoroquinolones, about 94.7% of the isolates were susceptible to both gatifloxacin and levofloxacin, while 90% and 87.1% were susceptible to moxifloxacin and ofloxacin, respectively (Table 3). A lower resistance (26.1%) to cotrimoxazole was observed in comparison with 98.6% resistance to trimethoprim (Table 3), and the MARI ranged 0.32-0.9 (Figure 1). Furthermore, four isolates were positive for sul3 genes while none were for sul2 gene (Table 4).
| Source | Recovered |
|---|---|
| Grass Root Rhizosphere | 120 (96.0) |
| Soil Butternut Rhizosphere | 5 (4.0) |
| Total | 125 (100) |
aData are presented as No. (%).
| Antibiotics | Responses, % | ||
|---|---|---|---|
| Susceptible | Intermediate | Resistant | |
| Meropenem | 88.1 | 3.0 | 8.9 |
| Cefuroxime | 1.5 | 2.9 | 95.6 |
| Ampicillin-sulbactam | 44.6 | 1.5 | 53.9 |
| Ceftazidime | 88.0 | 1.3 | 10.7 |
| Cefepime | 58.7 | 12.0 | 29.3 |
| Minocycline | 97.8 | 0.0 | 2.2 |
| Kanamycin | 38.5 | 4.6 | 56.9 |
| Ofloxacin | 87.1 | 10.0 | 2.9 |
| Levofloxacin | 94.7 | 4.0 | 1.3 |
| Moxifloxacin | 90.0 | 7.2 | 2.8 |
| Ciprofloxacin | 74.3 | 1.4 | 24.3 |
| Gatifloxacin | 94.7 | 8.0 | 1.3 |
| Polymyxin B | 97.1 | 0.0 | 2.9 |
| Aztreonam | 14.5 | 27.5 | 58.0 |
| Cotrimoxazole | 63.8 | 10.1 | 26.1 |
| Trimethoprim | 0 | 11.4 | 98.6 |
| Resistance Genes | Percentage Detected/phenotypic resistance, % |
|---|---|
| Sul3 | 12.1 |
| Sul2 | 0 |
5. Discussion
Commensal S. maltophilia may end up as an opportunistic pathogen (37). As revealed in this study, these bacteria are easily culturable, and appear ubiquitous, probably due to their resilience in the face of environmental stress (38). Our experience in this study suggests that the recovery of the organisms varies from place to place. As some studies have reported the isolation of this bacteria from soil butternut and walnut rhizosphere (39, 40), only 5 (4%) were isolated from the soil butternut rhizosphere compared to 120 (96%) from grass rhizosphere. The intrinsic resistance of this organism to imipenem was exploited for their isolation and API, supported by molecular identification, allowed convenient discrimination between the Stenotrophomonas species and other imipenem-resistant bacteria only (32).
The recovery rate of this bacterium appears to be increasing with time compared to when the bacteria was initially discovered. This scenario is buttressed by our findings as well as those of Gulmez et al. (41) which showed a higher frequency of occurrence of this specie than previously observed. S. maltophilia has been reported to be resistant to myriads of antibiotics (42, 43). This high resistance characteristic which was peculiar to clinical isolates has now been observed among environmental strains (44, 45). The resistance observed to kanamycin and trimethoprim in this study was in agreement with the report of Musa et al. (46) on commensal S. maltophilia from Osphronemus goramy. Similarly, S. maltophilia resistance to cephalosporin was higher in this study compared to that reported previously (47).
Berg et al. (48) and Crossman et al. (49) also noted that resistance to conventional antibiotics would have helped S. maltophilia to compete with other rhizospheric bacteria and made them survive in their habitat. This assertion is pertinent as all the isolates here showed MARI > 0.2, which implies that they have arisen from high-risk sources where antibiotics is in constant arbitrary use resulting in high selective pressure, as reported by Suresh et al. (50). Fluoroquinolone and polymycin B, both of which showed good activities against the S. maltophilia isolates, are usually the antibiotics of choice in the treatment of infections by the bacteria. The activities of these antibiotics against the bacteria have been similarly reported by Gales et al. (10) and Tripodi et al. (51). Valdezate et al. (52) observed that > 95% (94.7% in this study) of the bacterial isolates in their study were susceptible to a fluoroquinolone. However, it is known that trimethoprim-sulfamethoxazole is the drug of therapeutic choice against S. maltophilia infections (10, 53-55); but several reports have shown that the prevalence of S. maltophilia strains that are resistant to trimethoprim-sulfamethoxazole are increasing (56-58).
In this study, about 26% of the S. maltophilia isolates were resistant to this antibiotic compared with 2% reported elsewhere (10). The trend continues to threaten the public health of individuals, especially in an HIV/AIDS infested populations where the immune system is weakened. Resistance to trimethoprim-sulfamethoxazole is mediated by the sulphonamide resistance sul genes among other determinants (59). A study in Portugal by Antunes et al. (60) detected sul1, sul2, or sul3 genes in some Gram-negative isolates. The sul3 gene was observed to meditate trimethoprim-sulfamethoxazole resistance (61). This gene was earlier detected in some Gram-negative isolates recovered from animals and foods in Switzerland and Germany (22-24), suggesting commensal S. maltophilia to be as important as its clinical counterpart.
The presence of sul3 genes in this study may imply that the endophytic and clinical strains possess a similar level of antibiotic resistance, which may be more extensive among some endophytic strains of S. maltophilia (2). This probably explains the resistance against cotrimoxazole observed in this study. The rise in this sulphonamide resistance worldwide has been attributed to the newest sulphonamide resistance gene, sul3, especially in nonclinical (human) specimens like fresh water and soil (used in this study), sewage loving animals and animal farm (25, 62); but the isolates harboring these genes can still infect human. The potential threat that such resistant isolates could be to public health, informed the call for a surveillance study of the sul gene and phenotypic sulfamethoxazole by Toleman et al. (59).
Commensal S. maltophilia appears to be an important commensal with comparable antibiogram characteristics to its clinical strains. It also appears to be abundant in grass and soil butternut rhizosphere in the Eastern Cape Province of South Africa. The MARIs of the bacterial isolates suggest that their sources have been under antibiotics selective pressure, which could be related to abuse of antibiotics. Their antibiogram characteristics also suggest that the bacterium is an important reservoir of antibiotic resistant determinants (especially sulphonamide resistance (sul3) genes) in the environment.