1. Background
Chronic obstructive pulmonary disease (COPD) is one of the most important causes of disability and mortality in the world. It causes physical disability, affects quality of life and causes death. Chronic obstructive pulmonary disease is the fourth cause of death in the United States of America (1). According to the global initiative for chronic obstructive lung disease (GOLD), COPD is defined as a preventable and treatable disease that leads to the narrowing of the airways and is not fully reversible (2). In industrial countries, cigarette smoking and in developing countries, cigarette smoking and environmental pollutants such as floating particles due to cooking in nonstandard environments are the most common causes of COPD (3). In addition to the role of cigarette, environmental pollutants and genetic factors, the role of infections have also been mentioned in the pathogenesis and progression of this disease (4).
Helicobacter pylori is a Gram-negative, microaerophilic bacterium with a slow growing nature. The most important biochemical index of H. pylori is the production of large quantities of urease. This bacterium colonizes the gastric mucosa and causes a long-term immune response and local and systemic inflammation in the host. They affect the gastric mucosa of almost 50% of the world’s population (5-7). Previous studies have provided extensive evidence on the role of H. pylori in chronic gastritis, peptic ulcer, B-cell lymphoma of gastric mucosa associated-lymphoid tissue (MALT) lymphoma and gastric cancer (diffuse, intestinal) (8-10).
Recent studies have shown that there is a relationship between H. pylori infection and extra gastric diseases such as cardiovascular, skin, liver and rheumatic diseases (11, 12). This bacterium is associated with several respiratory diseases such as COPD, bronchiectasis, asthma, lung cancer and lung tuberculosis (13-15). Indeed, before identifying H. pylori, higher incidence of COPD and tuberculosis had been observed in patients with peptic ulcers compared to the normal population (16-20). Release of similar inflammatory cytokines in H. pylori infection and acute COPD attacks has been proved by some studies (16, 17, 21). The probable mechanism for the relationship between H. pylori and lung diseases might be the systemic effect of gastrointestinal peptides (gastrin, somatostatin) and cytokine release or direct injury and chronic inflammation of airways due to aspiration and inhalation. Since the release of inflammatory cytokines including IL1β, IL8 and TNFα is observed in chronic lung diseases and H. pylori eradication causes returning of these cytokines to the normal levels (22), it seems that activation of inflammatory mediators by H. pylori is the pathogenic mechanism of extragastric manifestations of H. pylori infection (22-25).
2. Objectives
The present study was designed to investigate the relationship between H. pylori and COPD via anti H. pylori IgG serology, real-time PCR of bronchoalveolar lavage and transbronchial biopsy urease tests.
3. Patients and Methods
This descriptive cross-sectional study was performed on 60 adults with COPD, who had been referred to our lung diseases diagnosis department in 2012. After obtaining history, physical examination, spirometry and confirmation of COPD diagnosis by the pulmonologist, subjects were selected through convenience sampling. The rate of airway obstruction in COPD patients was determined based on the GOLD criteria (Global Initiative for Obstructive Lung Diseases):
Grade 0: Patients at risk with normal spirometry
Grade 1: Mild obstruction, FEV1/FVC < 70%, FEV1 ≥ 80%
Grade 2: Moderate obstruction, FEV1/FVC < 70, 50% ≥ FEV1<80%
Grade 3: Severe obstruction, FEV1/FVC < 70%, 30% ≥ FEV1 < 50%
Grade 4: Very severe obstruction, FEV1/FVC < 70%, FEV1 < 30% or FEV1 < 50%, associated with respiratory failure and symptoms of right-sided heart failure (2).
After explaining the research goals and details to the subjects and obtaining their informed written consent, they were enrolled in the study. The study was approved by Kerman University of Medical Sciences (code: 91/218). All patients underwent spirometry. In order to determine the severity of lung chronic obstruction, the GOLD criteria, and for determining the severity and prognosis of disease, the BODE-index, were used. Four factors were used for the evaluation of the severity of obstruction based on the BODE-Index including, weight (BMI), airflow obstruction (FEV1), dyspnea and exercise capacity (six-minute walking distance), that in comparison to FEV1 provide more accurate information about the rate of obstruction and the disease prognosis (26, 27).
Demographic data including age, sex, cigarette smoking, opium consumption and educational level were recorded and symptoms of reflux including regurgitation, heartburn, epigastric pain, dysphonia and dysphagia were recorded based on the gastroesophageal reflux disease (GERD) questionnaire (28). Those who were in an exacerbation condition of COPD and had a history of H. pylori eradication and also had severe hypoxia and cardiac arrhythmia were excluded from the study. All subjects underwent bronchoscopy and bronchoalveolar lavage (BAL) and biopsy sampling of the airways. Biopsy samples were studied using the urease test, the BAL sample was studied by Real time PCR and serum was serologically examined for detection of anti H. pylori IgG.
3.1. Serological Test
The serum samples were kept at -20°C and used for measuring anti H. pylori IgG by the enzyme linked immunosorbent assay (ELISA) method (Trinity kit, Germany). Samples with IgG ≥ 1.2 immune status ratio (ISR) were considered positive according to the manufacturer's instructions.
3.2. DNA Extraction
After collecting BAL samples, they were kept at -80°C until use in the experiments. Then, H. pylori DNA was extracted using the QIAamp DNA Mini kit (Qiagen, Germany), according to the manufacturer’s instructions. Extracted DNA pellets were re-suspended in 100 μL of pre-warmed elution buffer and stored at -20°C until use.
3.3. Molecular Test
A SYBR Green Real Time PCR assay was developed to screen DNA for H. pylori. The primers amplify a 102 bp region for detection of UreA (Urease Gene) in H. pylori and a 145 bp region for detection of pathogenic H. pylori. The urease gene of H. Pylori was used in order to detect the presence of this bacterium and CagA was used for identification of the pathogenic strains of the bacterium. We used the β-Actin housekeeping gene for the internal control gene and for normalizing the test. PCR reactions contained 5 µL of DNA, 100 ng of each primer, and 14 µL of Maxima SYBR Green PCR Master Mix (Thermo Scientific) in a 20 µL total volume. Thermo cycling conditions were as follows: 95°C for 10 minutes, 40 cycles at 95°C for 15 seconds, and 60°C for 40 seconds; quantitative determination of the amplified products was done with the Rotor Gene 6000 (Corbett Research, Australia). The PCR results were considered positive when copy/mL ≥ 10 (29-31). Sequence of primers has been shown in Table 1.
| Name of Gene | Forward Primer | Reverse Primer |
|---|---|---|
| UreA | GAGAATGAGATGAAACTCACCC | TTGTCTGCTTGTCTATCAACC3 |
| CagA | CTCATTGCGAAGGCGACCT | TCTAATCCTGTTTGCTCCCCA |
| β-actin | TGCCTATCAGAAAGTGGTGGCT | GCTCAAGGCCCTTCATAATATCC |
3.4. Urease Test
Rapid Urease Test was performed on bronchial samples by the Man Company Kit (Iran) and based on the producer manual; accordingly, 1 mL of the prepared solution was poured into a cup and the biopsy sample was placed in this solution for 60 minutes. Color change from yellow to pink-purple was considered as H. pylori positive; this occurs due to ammonium production by the bacterium.
4. Results
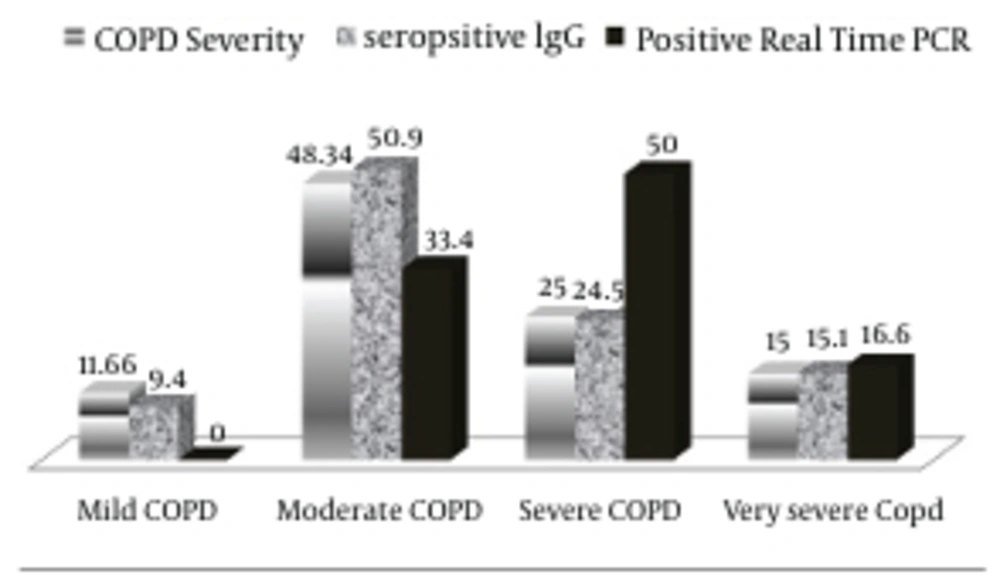
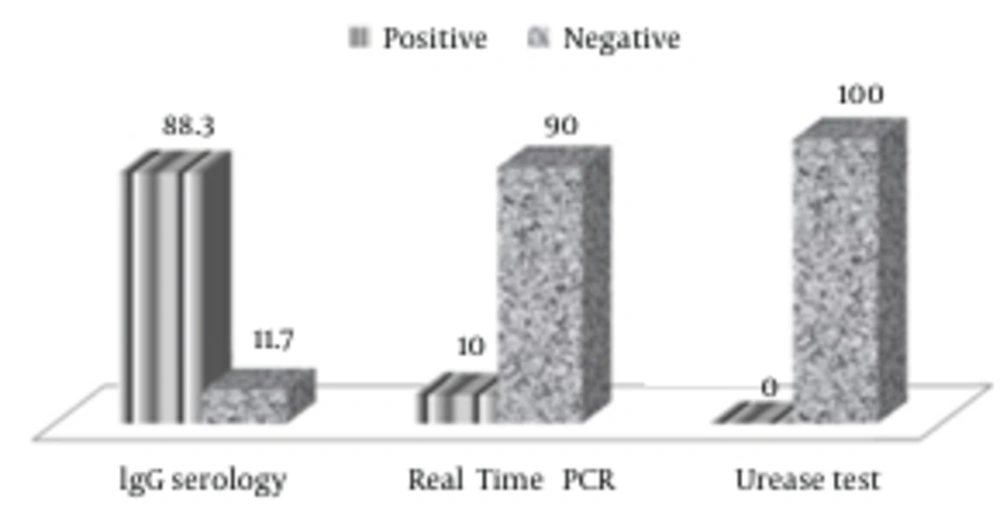
The mean age of participants was 60.65 ± 9.15 years (age range: 40-86). In total, 15 individuals (25%) were female and 45 (75%) were male. From all participants, 36 (60%) were cigarette smokers and 41 (68.3%) were opium addicts. In regards to the severity of disease based on FEV1, seven patients (11.66%) had mild obstruction, 29 (48.34%) had moderate obstruction, 15 (25%) had severe obstruction and 9 (15%) had very severe obstruction. The prevalence of H. pylori in COPD patients was 10% (6 of 60 patients) based on real-time PCR, 88.3% (53 of 60 patients) based on serology and 0% based on the urease test (Figure 2).
For determining the relationship between H. Pylori (based on urease test) and disease severity, urease tests were obtained from all patients, and the results were negative for all subjects. The relationship between H. pylori (based on serology) and disease severity was also determined based on the GOLD criteria; in the group that were seropositive based on the enzyme linked immunosorbent (ELISA) method, five (9.4%) had mild obstruction, 27 (50.9%) had moderate obstruction, 13 (24.5%) had severe obstruction and eight (15.1%) suffered from very severe obstruction. No significant relationship was found between the presence of H. pylori (based on serology) and disease severity (P = 0.907). The results are shown in Table 2 and Figure 1.
According to the results of real-time PCR and considering the severity of disease based on the GOLD criteria, amongst those with positive PCR results, one patient (16.6%) had very severe obstruction, three (50%) had severe obstruction and two (33.3%) had moderate obstruction. In other patients real-time PCR results were negative. The relationship between presence of H. pylori (based on real-time PCR) and disease severity was not statistically significant (P = 0.808). The results are demonstrated in Table 3 and Figure 1.
In order to increase the accuracy of determining prognosis of the disease, the BODE index was also used. Accordingly, based on PCR, BODE Index of four patients (66.7%) was between three and four, one patient (14.3%) had a score of six and one patient (16.7%) scored eight. Based on seropositivity, BODE score of 38 patients (71.7%) was between three and four, 10 (18.9%) scored from five to six and five (9.4%) scored from seven to nine; a higher BODE Index correlates with an increasing risk of death. No significant relationship was found between H. pylori infection (based on real-time PCR and serology) and BODE index (P = 0.475 and P = 0.695, respectively). The results are shown in Tables 2 and 3.
Based on the urease, serology and real-time PCR tests and logistic regression, no significant relationship was found between H. pylori in COPD patients and variables of age, educational level, cigarette smoking and reflux symptoms. Based on the serology test, logistic regression showed a significant relationship only with dysphagia (P = 0. 035) (Table 1). Moreover, based on real-time PCR of opium addicts, both raw test and logistic regression showed a significant relationship (P = 0.041) (Table 3) (Figure 2).
| Serology | Crude | Adjusted | ||||||
|---|---|---|---|---|---|---|---|---|
| B | S.E | P Value a | OR | B | S.E | P Value | OR b | |
| BODE index | -0.129 | 0.584 | 0.826 | 0.879 | 0.412 | 1.051 | 0.695 | 1.511 |
| FEV1 | 0.495 | 0.359 | 0.167 | 1.64 | -0.07 | 0.609 | 0.907 | 0.931 |
| Age | -0.020 | 0.044 | 0.644 | 0.980 | -0.04 | 0.062 | 0.497 | 0.957 |
| Cigarette smoking | 0.001 | 0.003 | 0.820 | 1.001 | 0.00 | 0.003 | 0.915 | 1.00 |
| Opium consumption | 0.127 | 0.894 | 0.887 | 1.13 | 0.139 | 0.886 | 0.876 | 1.149 |
| Hoarseness | 0.327 | 0.961 | 0.733 | 1.38 | 1.06 | 0.818 | 1.93 | 2.90 |
| Heartburn | 1.36 | 1.11 | 0.232 | 3.90 | 1.69 | 0.886 | 0.056 | 5.44 |
| Regurgitation | -0.657 | 1.08 | 0.545 | 0.518 | 0.087 | 0.812 | 0.915 | 1.09 |
| Dysphasia | 0.943 | 0.985 | 0.338 | 2.56 | 1.76 | 0.840 | 0.035 | 5.86 |
| Epigastria pain | 0.950 | 0.983 | 0.333 | 2.58 | 1.43 | 0.827 | 0.083 | 4.20 |
a Based on logistic regression.
bB(Estimated parameter coefficient), SE (Standard Error),OR(Odds Ratio) , FEV1( Forced Expiratory Volume in one second).
| PCR | Crude | Adjusted | ||||||
|---|---|---|---|---|---|---|---|---|
| B | S.E | P Value a | OR | B | S.E | P Value | OR | |
| BODE index | -0.129 | 0.584 | 0.082 | 0.879 | -0.064 | 0.907 | 0.475 | 0.052 |
| FEV1 | -0.208 | 0.418 | 0.619 | 0.812 | -0.173 | 0.714 | 0.808 | 0.084 |
| Age | -0.009 | -0.044 | 0.844 | 0.991 | -0.015 | 0.068 | 0.820 | 0.985 |
| Cigarette smoking | 0.000 | 0.003 | 0.900 | 1.00 | -0.001 | 0.003 | 0.788 | 0.999 |
| Opium consumption | -2.420 | 1.170 | 0.038 | 0.088 | -2.36 | 1.15 | 0.041 | 0.094 |
| Hoarseness | -0.351 | 1.030 | 0.733 | 1.42 | 0.315 | 0.957 | 0.742 | 1.37 |
| Heartburn | 0.402 | 1.166 | 0.730 | 0.669 | 0.154 | 0.955 | 0.872 | 1.16 |
| Regurgitation | -0.859 | 1.070 | 0.425 | 2.36 | -0.811 | 0.953 | 0.395 | 2.25 |
| Dysphasia | 0.389 | 1.260 | 0.758 | 0.67 | 0.214 | 1.162 | 0.854 | 1.77 |
| Epigastria pain | 0.542 | 1.110 | 0.628 | 1.71 | 0.575 | 0.962 | 0.550 | 1.37 |
a Based on logistic regression.
5. Discussion
In the present study, bronchoalveolar fluid of 10% of COPD patients was positive for H. pylori according to real time PCR and 88.3% of patients had positive results according to their serology test. Urease test results were negative for all patients. However, there was no significant relationship between the obtained results and the severity and prognosis of COPD based on the GOLD and BODE index criteria. The relationship between chronic bronchitis and peptic ulcer was determined several years prior to the identification of H. pylori, and the prevalence of chronic bronchitis in patients with peptic ulcer was shown to be two to three times more than the control group (18, 32). In a study performed during 1998, the prevalence of H. pylori seropositivity in patients with chronic bronchitis was more than that of the control group (81.6% vs. 57.9%) (33). A study in Denmark demonstrated an association between H. pylori IgG seropositivity and chronic bronchitis (34). According to this study, the prevalence of H. pylori IgG and CagA protein seropositivity in COPD patients was significantly higher than the control group and there was no significant correlation between seropositivity and pulmonary function test (35). It has also been reported that cases with positive IgG H. pylori antibody are more likely to be among chronic bronchitis patients (36). The findings of these studies are similar to our results.
In another previous study, Anti-Cag A level was significantly higher in the COPD group compared to the control group and, similar to our study, no significant relationship was found between H. pylori infection and COPD severity (37). In a study on the relationship between H. pylori infection and pulmonary function based on FEV1 and FVC, lower pulmonary function was reported in seropositive patients, yet after statistical adjustment for socioeconomic status, this relationship disappeared (38). In our study, also, no significant relationship was found between H. pylori seropositivity and pulmonary function tests. Furthermore, in one study that compared non-smoking male patients with non-smoking males without chronic respiratory disease, a strong relationship was found between COPD and H. pylori serology, yet, like our study, no significant relationship was found between H. pylori seropositivity and pulmonary function tests (39). According to a study on the serum of 49 patients with chronic obstructive pulmonary disease, H. pylori IgG level in COPD patients was significantly higher than the control group and there was a significant correlation between the severity of the disease and H. pylori seropositivity (13). The rate of H. pylori seropositivity in our patients was 88.3% and there was no significant correlation between the severity of the disease and seropositivity; the difference between our and the previous study might be due to different sample sizes. A recent study showed that both peptic ulcer and positive H. pylori serology in COPD patients are more than the control group (40).
There are very limited studies that have performed a direct isolation of this bacterium from lung tissue. In one of the previous studies, 34 patients with various types of lung diseases underwent bronchoscopy and biopsy of lung tissue. Histopathology and urease test showed no positive evidence of H. pylori presence in biopsy samples (41). Similarly, in the present study, none of the urease tests were found positive in regards to H. pylori. In some previous studies on patients with bronchiectasis, BAL and lung tissue were investigated by PCR for the presence of H. pylori and, DNA of this bacterium was not found in any of the samples (42, 43). However, in the present study, the real-time PCR detected DNA of H. pylori bacterium in BAL of 10% of COPD patients.
All previous studies have been based on serological tests, however there are several intervening factors that affect the performance of these tests. Moreover, Iran is among regions with high prevalence of H. pylori and approximately 90% of adults in Iran are infected with this bacterium (44). In addition, factors such as age, sex and socioeconomic conditions are involved in COPD and H. pylori infection. Therefore, socioeconomic status should surely be considered in this regard. Indeed, cigarette smoking is also an intervening factor and is one of the major causes of COPD. In regards to the relationship between H. pylori infection and cigarette smoking, there are controversies amongst previous findings (15, 37). In the present study, there was no significant relationship between cigarette smoking and H. pylori in COPD patients.
5.1. Study Limitations
Chronic obstructive pulmonary disease patients, due to sputum production and many gastrointestinal problems frequently use antibiotics and anti-acids and since consumption of these medicines can affect the study results, they should be considered as part of patient’s history. Further studies with a greater sample size and more severe cases of COPD are recommended, because in studies with more severe COPD patients, the number of positive cases in PCR might be higher, as the present study, revealed that positive cases in real time PCR were those with more severe COPD. Another limitation of the present study was the lack of a control group, yet since bronchoscopy is an invasive method, including a control group was ethically impossible.
In the present study, DNA of H. pylori was detected in about 10% of COPD patients by BAL real time PCR and 88.3% of patients were IgG seropositive. As previously mentioned, most previous studies had been based on serology. However, in the present study, in addition to serological tests, real time PCR was applied. The findings can explain the hypothesis of direct injury and chronic inflammation through inhalation and aspiration in addition to systemic immune response resulted from H. pylori colonization.
In fact, it is thought that H. pylori along with the host genetic susceptibility and other environmental risk factors can make the person susceptible to COPD occurrence or lead to COPD worsening. Although we found H. pylori infection in some patients with chronic obstructive pulmonary disease, the results of this study, could not explain the pathogenic mechanisms in chronic obstructive pulmonary disease. It is recommended for other researches to measure inflammatory factors such as IL-1, INFγ and IL8 in BAL of COPD patients who are H. pylori positive based on real time PCR of BAL, in order to identify pathogenic mechanisms of the relationship of this bacterium with COPD. Indeed, studies on genetic loci, through identifying human leukocyte antigens (HLAs), which can make the individual vulnerable to both H. pylori infection and COPD, are recommended.