1. Background
Among the etiologic agents of infectious disease, Staphylococcus aureus, especially Methicillin-Resistant Staphylococcus aureus (MRSA) strains are the main agents of human infections (1). This pathogen can cause nosocomial infection in such a manner that it is the most common pathogen isolated from patients in hospitals that can cause wide range of infections from skin and soft tissue infections till toxic shock syndrome and life threatening syndromes. During the end of 1990s, increasing of S. aureus infections was led to isolation of MRSA (2-5). Nearly, all S. aureus isolates produce various toxins and enzymes that are important in the pathogenicity of this bacterium (6, 7). With the emergence of resistant strains at 1961 that had multidrug resistance, the treatment of S. aureus infections had been paid more attention. The MRSA stains are widely distributed around the world that shows their resistance to both penicillins and cephalosporins (8, 9).
The MRSA produces a unique type of Penicillin Binding Protein 2a (PBP2a) that has low affinity for β-lactam antibiotics (10, 11). Most of MRSA strains can also produce a leukotoxin as Panton-Valentine Leukocidin (PVL) that increases their virulence and can cause severe necrotic pneumonia (8, 12). Pathogenicity of S. aureus results from the surface cell wall structures and different exoproteins that PVL is one of the most important of them for overcoming host immunity and disease progress (13). Pore forming toxins perforate membranes of host cells, mainly the plasma membrane and also intracellular organelle membranes. They directly kill target cells, in order to intracellular delivery of other bacterial or external factors, releasing nutrients or escaping from phagosomal space. Panton-valentine leukocidin is a member of pore forming toxins that targets host leukocytes. The PVL- producing strains are commonly involved in the skin and soft tissue infections as well as able to cause life threatening infections like pneumonia (7, 8, 12). Two open reading frames are responsible for coding PVL, i.e. lukS-pv and lukF-pv. The presence of pvl gene is a genetic marker for the MRSA populations (14). Recently, reports about infections caused by pvl-positive strains have been increased that necessitate investigations about the prevalence of this virulent marker among MRSA strains in hospital and also community acquired infections.
2. Objectives
The aim of the present study was to discover the association of pvl and mecA in MRSA strains isolated from hospitalized patients in three educational hospitals of Ahvaz City, Iran.
3. Materials and Methods
3.1. Sampling
Fifty S. aureus isolates were collected from patients in three educational hospitals of Ahvaz, including Imam Khomeini, Golestan and Taleghni hospitals. These samples were obtained from 200 samples collected from different sections of the above-mentioned hospitals including Outpatient Department (OPD), skin, men surgery, ophthalmology, nephrology, pediatric, women, orthopedic, ear, nose and throat (ENT), neonates and internal medicine. Samples were collected from skin lesions, blood cultures, burns, intravenous catheters, wound drainages, abscesses, tracheal secretions, synovial fluids, ocular secretions and urines. These isolates were identified based on standard morphological and biochemical tests including catalse, oxidase, tube coagulase, mannitol fermentation, sensitivity to furazolidon, resistance to bacitracine, PYR test and Voges-Proskauer (15).
3.2. Determining Antibiotic Susceptibility
In order to determine methicillin resistance of isolates Muller-Hinton Agar (MHA, Merck, Germany) screening test was used according to CLSI (clinical and laboratory standards institute) (16). Briefly, a 0.5 McFarland suspension was prepared from pure culture of isolates and then cultured on MHA containing oxacillin (6 μg/mL). For this purpose using a sterile swab the bacterium was inoculated as a dot with a 10 - 15 mm diameter and a strike culture was prepared on the other part of plate and incubated at 35°C. The results were studied after 24 and 48 hours of incubation. Growth of only one colony on this culture medium revealed methicillin resistance of that isolate. Staphylococcus aureus ATCC 29213 as the negative control and sensitive to methicillin and S. aureus ATCC 33591 as the positive control and resistant to methicillin were used in all experiments. Furthermore, the susceptibility of isolates to oxacillin was surveyed using the standard Kirby-Bauer disc diffusion method (17).
3.3. DNA Extraction
The isolates were cultured in Trypticase Soy Broth (TSB, Merck, Germany) for 18 h at 37°C. Then, 1.5 mL of culture was centrifuged (12000 rpm, 10 minutes) and the precipitate was dissolved in one mL deionized water and boiled for 20 minutes. After centrifugation (5000 rpm, 5 minutes) the supernatant was slowly mixed with phenol-chloroform-isoamyl alcohol (1: 24: 25) at 1: 1 ratio and the aqueous phase was harvested by centrifugation at 13000 rpm, 30 seconds. Cold isopropanol was added to aqueous phase (60.100, v/v) and stored overnight at -22°C. The DNA was then precipitated and washed subsequently with absolute and 70% ethanol. Finally, DNA was air-dried at 37°C and dissolved in 200 μL sterile deionized water and stored at -22°C till experiments (18).
3.4. Polymerase Chain Reaction
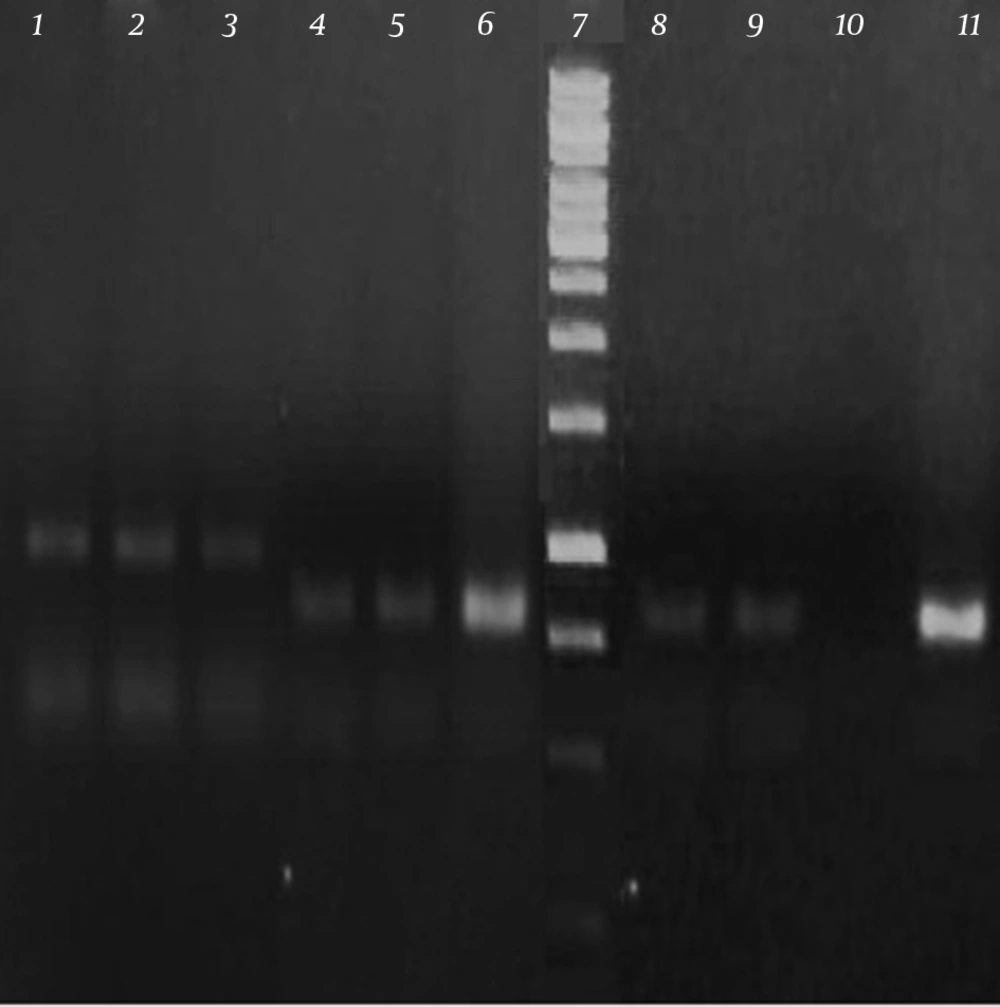
Polymerase Chain Reaction (PCR) was performed in a final 25 μL volume reaction containing PCR buffer (10x), Magnesium Chloride (MgCl2) (2 mM), Deoxynucleotide Triphosphates (dNTPs) (0.2 mM), forward and reverse primers (10 ρmol/μL), template DNA (1 μL), Taq DNA polymerase ( 1.5 u) and deionized water. The PCR method was performed in thermal cycler (Bio-Rad, USA) according to the following program: initial denaturation (94°C, 2 minutes), 35 cycles each composed of initial denaturation (94°C, 30 seconds), primer annealing (55°C, 45 seconds) and extension (72°C, 75 seconds) and a final extension (72°C, 4 minutes) (19). Positive control for mecA and pvl genes and negative control (distilled water) were also regarded in each series of PCR reaction. The PCR product was subjected to electrophoresis in 1% agarose gel containing DNA safe stain and documented using gel documentation (UVI TEC, Cambridge, UK).
4. Results
From a total of 50 samples, 27 samples (54%) were belonged to Imam Khomeini Hospital, 16 samples (32%) from Golestan Hospital and 7 samples (14%) from Taleghani Hospital. According to the patient gender, 26 samples (52%) were isolated from men while 24 samples (48%) were from women. The number of samples from different clinical specimens and hospital sections are presented in Tables 2 and 3, respectively.
| Clinical Sample | Number of Isolates |
|---|---|
| Skin lesions | 11 |
| Blood cultures | 9 |
| Burns | 6 |
| Urines | 3 |
| Abscesses | 3 |
| Tracheal Secretions | 3 |
| Synovial Fluids | 2 |
| Ocular Secretions | 3 |
| Intravenous Catheters | 6 |
| Wound Drainages | 4 |
| Ward | Number of Isolates |
|---|---|
| OPD | 13 |
| Skin | 13 |
| Men surgery | 1 |
| Ophthalmology | 3 |
| Nephrology | 8 |
| Pediatric | 3 |
| Women | 3 |
| Orthopedic | 2 |
| ENT | 2 |
| Neonates | 1 |
| Internal Medicine | 1 |
a Abbreviations: OPD, Outpatient Department; ENT, Ear, Nose and Throat.
The results of antibiotic susceptibility tests revealed that all isolates were resistant to methicillin. Following PCR reaction with mecA and pvl specific primers, 314 bp and 433 bp PCR products were produced for mecA and pvl genes, respectively (Figure 1).
Table 4 shows the total number of MRSA isolates and their mecA and pvl markers. Based on the obtained results, 30% (15 samples) of MRSA strains were positive for mecA gene while 6% (3 samples) had pvl gene. None of the samples had simultaneously both virulence markers.
| Isolate | mecA | pvl |
|---|---|---|
| 1 | - | - |
| 2 | - | - |
| 3 | - | - |
| 4 | - | - |
| 5 | - | - |
| 6 | - | - |
| 7 | - | - |
| 8 | + | - |
| 9 | + | - |
| 10 | - | - |
| 11 | - | - |
| 12 | - | + |
| 13 | + | - |
| 14 | - | - |
| 15 | - | - |
| 16 | - | - |
| 17 | - | - |
| 18 | + | - |
| 19 | - | - |
| 20 | - | - |
| 21 | + | - |
| 22 | - | - |
| 23 | - | - |
| 24 | + | - |
| 25 | - | - |
| 26 | - | + |
| 27 | - | - |
| 28 | + | - |
| 29 | - | - |
| 30 | + | - |
| 31 | - | - |
| 32 | - | - |
| 33 | + | - |
| 34 | - | - |
| 35 | - | - |
| 36 | - | - |
| 37 | - | - |
| 38 | - | - |
| 39 | - | - |
| 40 | - | - |
| 41 | - | - |
| 42 | - | + |
| 43 | - | - |
| 44 | - | - |
| 45 | + | - |
| 46 | + | - |
| 47 | + | - |
| 48 | + | - |
| 49 | + | - |
| 50 | + | - |
5. Discussion
Staphylococcus aureus is one of the most common pathogens that have been isolated from patients in hospitals, especially MRSA strains are among important nosocomial infections for humans (1). Having knowledge about the prevalence of MRSA and their virulence factors is useful for treatment and control of community and hospital acquired S. aureus infections. Following the emergence of MRSA strains, molecular studies showed that some of these isolates carry pvl gene (20). The pvl positive strains lead to infections with different clinical appearance even in immunocompromised patients lead to necrotic pneumonia, which its mortality can be as much as 75% (8). Therefore, frequent monitoring of this pathogen, its antibiotic susceptibility and determining their virulence factors is of great importance in control and treatment of infections.
According to the results of this study, only 30% of isolates identified as MRSA were positive for mecA gene. This explains that it maybe mecA positive MRSA isolates have different mechanism for methicillin resistance than mecA. These results are in agreements with other reports such as reported by Bagdonas et al. in Lithuania (23.4%) (21), Turnidge et al. in Australia (24%) (22), Li et al. in China (12%) (23) and also in different parts of Iran, e.g. Fatholahzadeh et al. in Tehran (36%) (24) and by Japoni et al. in Shiraz (43%) (25). However, the frequency of mecA positive isolates in this study is more than the results of Bagdonas et al. Turnidge et al. and Li et al. while is less than the results obtained by Fatholahzadeh et al. (2009) and Japoni et al. This finding is a hopeful result that the frequency of mecA in Ahvaz is yet less than other studied areas of Iran. The occurrence of pvl gene in previous studies has been reported from 2% - 35% (26, 27). In comparison the obtained results for pvl gene in the present study is near to the lower limit obtained from similar studies. No association between mecA and pvl genes was found in our study. It is possible that mecA and pvl genes but not both of them be present on the chromosome of clinical isolates of S. aureus.
The obtained results in the present study are in agreement with the finding of Okon et al. (27) and Terry Alli et al. (9) that reported no pvl positive strain is there among tested MRSA strains. Okon et al. (27) have suggested it is maybe that resistance determinants be carried on other mobile elements, such as plasmids, transposons, and phages; so, their elimination from bacterial cell would result in the absence of mecA gene and consequently no association with pvl gene. Affolabi et al. (28) also reported no significant association between pvl and mecA in S. aureus isolates from Cotonou. However, the pvl gene has been reported in some MRSA in other studies (29, 30).
According to the results of this study, PCR assay for MRSA gene can be useful for definite diagnosis of MRSA strains. Identification of mecA positive strains can be used as a guide for separating infected patients from others in hospital environment in order to prevent gene transfer among clinical strains and also distribution of virulent factors.