1. Background
Cholera is a major public health concern, in countries where access to safe water and adequate sanitation cannot be guaranteed, for all residents. Vibrio cholerae serogroups O1 and O139 are the causative agents of cholera (1). Reports from the epidemic forms of cholera diarrhea, particularly in developing countries, show that toxigenic V. cholerae with O1 or O139 serogroup is the main causative microorganism. Cholera toxin, encoded by ctx gene, is a potent factor, which induces intense dehydration and pathogenesis (2). There are two biotypes of V. cholerae O1, classical and El Tor, which are believed to have evolved from separate lineages among the two biotypes, strains belonging to the El Tor biotype have better adaptability to survive in the environment and in the human host (3). Diagnosis of V. cholerae, based on multiplex polymerase chain reaction (PCR) can be useful.
Multiplex PCR provides the possibility of evaluating several genes, through one PCR reaction, in a short time interval, by designing different target-specific primers. This method is simple, fast and cost-saving and has the ability to test a large number of samples, at the same time. Moreover, technicians can interpret the results easily (2). In 2012, the world health organization estimated that every year, there are 3 - 5 million cholera cases and more than 100,000 people die of the disease, with the majority (99%) of the cases and deaths occurring in Sub-Saharan Africa and Southern Asia (4). However, V. cholerae serogroup O1 still is the most common cause of cholera epidemics. Cholera is an endemic disease in Iran and is common in summer and early month of autumn. The causative serogroup, in our country, is O1 and we did not have any report for isolation of O139 serogroup in recent outbreaks (5).
Alborz is one of Iran’s provinces, which has a population of 2,412,513 people, based on 2011 census. During the last recent decades, several cases of cholera epidemics have occurred in Karaj, in 3 - 5-year intervals (6). In each outbreak, it has always been a big concern to choose the type of antibiotic. Although the national guidelines recommend special antibiotics, based on the antibiogram of national reference laboratory (7), it seems that, because of uncontrolled usage of antibiotics in the society and due to the changes in the serotypes causing the disease, it is essential to monitor the status of drug resistance permanently and to revise the current prescriptions guidelines (8).
2. Objectives
In this study, we aimed to determine the antibiotic susceptibility pattern of V. cholerae. Therefore, we reviewed the epidemiologic characteristics of the disease and conducted the antibiotic susceptibility test for the V. cholerae samples, collected from El Tor infected patients, in 2011.
3. Materials and Methods
This was a cross-sectional study, which reviewed a cholera epidemic that occurred in Alborz province, in 2011. From the beginning of the cholera epidemic (June 14, 2011) until the end of the disease (October 22, 2011), a total of 9844 specimens were taken from suspected cases, among diarrheal patients, via rectal swabs. The specimens were placed in Cary-Blair transport medium and sent to laboratory. Samples were enriched in alkaline peptone water and isolated on thiosulphate-citrate-bile salt-sucrose agar. Strains were serotyped using polyvalent O1 and monospecific Inaba and Ogawa antisera (9). All antiserums type determination serotyping test were performed with 1TOR 1R polyvalent antiserum 1T and monovalent Ogawa and Inaba (Baharafshan institute of research and development, Tehran, Iran) were purchased, which was approved by the national reference laboratory. From the 244 confirmed cases, 239 cases underwent antibiogram test, via disk diffusion method (Kirby-Bauer) and based on National committee for clinical laboratory standards (NCCLS) instructions. The standard Escherichia coli ATCC 25922 was used for antibiogram quality control and, eventually, all results were interpreted and reported, using NCCLS standard table (10).
Using the chi-square and Fisher exact test, the relationship between antibiotic resistance and other variable was tested.
4. Results
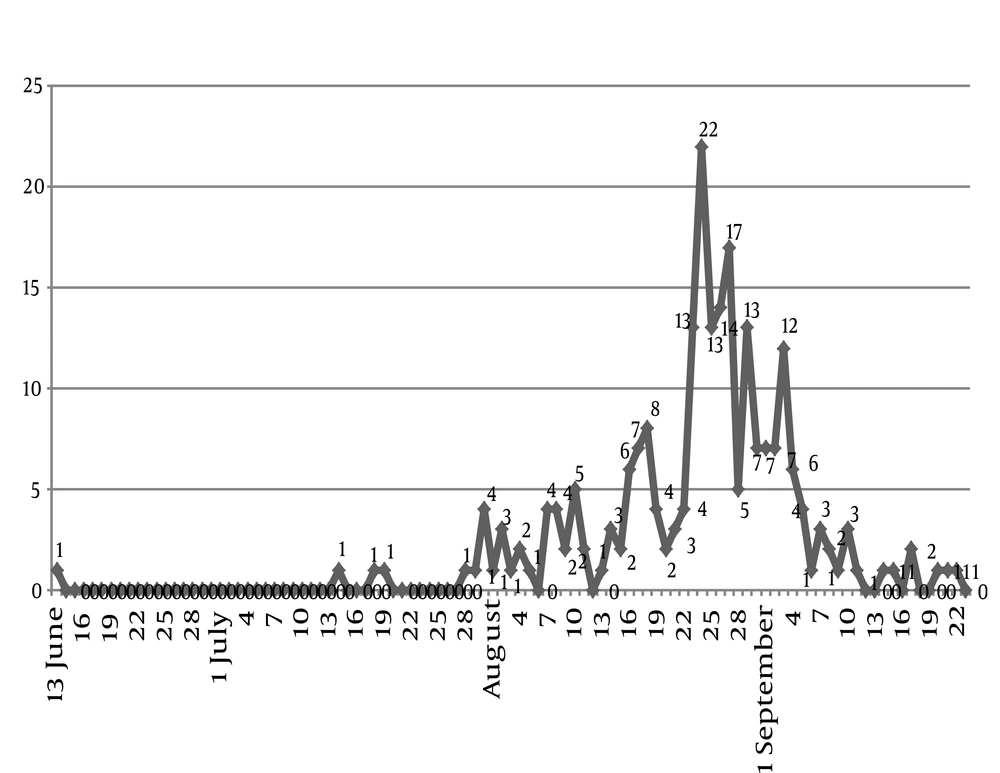
The first case of cholera occurred in a 58-year-old man, in June 14, 2011. In total, until October 22, 2011, which was announced as the end of outbreak, 9844 samples were taken from diarrheal patients. Regarding the type of V. cholerae, 244 El Tor biotype positive cases were reported. All cases were serotype Ogawa. Figure 1 shows the trend of the incidence of El Tor, in the province, in terms of days. From all patients in Alborz province, three patients died. Therefore, the case fatality rate reached 1.3%. The mean age of patients was 37.8 years and the highest incidence rate occurred in the age group 21 - 30 years. Based on antibiogram tests, ciprofloxacin had the highest level of antibiotic susceptibility (99.6%) and co-trimoxazole showed the highest level of antibiotic resistance (95.4%).
Drugs like doxycycline and tetracycline, which are among the drugs recommended in treatment guidelines, had antibiotic sensitivities of 84.7% and 81.2%, respectively. More details on drug resistance of different antibiotics are shown in Table 1. Using Chi-square and Fisher exact tests, the relationship between antibiotic resistance to doxycycline and sex was tested. This was not significant (P = 0.622). Using the Chi-square test, the relationship between antibiotic resistance to tetracycline and sex was tested. This was also not significant (P = 0.073). Using Fisher exact test, the relationship between antibiotic resistance to tetracycline and doxycycline was tested. This was significant (P = 0.000).
| Result of Antibiotic Susceptibility | Ciprofloxacin | Azithromycin | Tetracycline | Doxycycline | Erythromycin | Furazolidone | Ampicillin | Co-Trimoxazole |
|---|---|---|---|---|---|---|---|---|
| Susceptible | 238 (99.6) | 227 (95) | 194 (81.2) | 209 (84.7) | 6 (2.5) | 37 (15.5) | 33 (13.8) | 7 (2.9) |
| Resistant | 0 (0) | 2 (0.8) | 36 (15.1) | 10 (4.2) | 13 (5.4) | 202 (84.5) | 110 (46) | 228 (95.4) |
| Intermediate | 1 (0.4) | 2 (4.2) | 9 (3.8) | 20 (8.4) | 220 (92.1) | 0 (0) | 96 (40.2) | 4 (1.7) |
aData are presented as No. (%).
5. Discussion
Most of outbreaks, which occurred in Iran from 1977 to 2005, were caused by Ogawa serotype. In recent years, a change has been made in the number of the dominant types of outbreaks in Iran and there has been a shift between Ogawa and Inaba, as the main types of outbreaks in the country (4). Based on the main results of this study, the highest level of susceptibility was observed in the case of ciprofloxacin (99.6%) and then azithromycin (95%). Nevertheless, it is noteworthy that the levels of resistance to tetracycline (15.1%) and doxycycline (4.2%), which are mentioned as the main drugs, in most of sources, are raised (11). Hence, the large number of tetracycline resistant cases (14.7%) is remarkable. Various studies in Iran and elsewhere have reported resistance of V. cholerae to chloramphenicol, erythromycin, kanamycin, tetracycline and sulfamethoxazole/trimethoprim (12). There was a significant relationship between the antibiotic resistance to tetracycline and doxycycline (P = 0.000), i.e. if a person is resistant to one of these two antibiotics, there is a chance of more than 90% for him/her to be resistant to the other drug, as well.
Comparing the results of this study, with other studies, the following results have been achieved. The Barati and colleagues study shows that the resistance to co-trimoxazole has had an increase and there has not been a notable change in ciprofloxacin susceptibility (6). In the study of Abera, the resistance to co-trimoxazole was 100%. A high level of resistance to chloramphenicol (94%) and ampicillin (89%) was observed. In this study, all cases were susceptible to doxycycline. The antibiotic susceptibility to ciprofloxacin and erythromycin in that study is almost similar to the results of our study; however, the resistance to ampicillin is greater while for tetracycline is lower (13). Data generated in the present study revealed that tetracycline, one of the main antimicrobial agents used for cholera treatment, was the most effective antibiotic. Our previous study, during the 2005 outbreak, also showed that all isolated stains of V. cholerae were susceptible to tetracycline. In Rahbar et al. study, all strains of V. cholerae that were susceptible to tetracycline, were also susceptible to doxycycline. Doxycycline is used as the first line drug for the treatment of cholera in Iran (5).
In Seas et al. study, data from these well-conducted trials show clearly that the quinolones are equally effective, as the standard therapy (multiple dose tetracycline regimen or single dose doxycycline regimen), in all clinical parameters (i.e., duration, total volume of stools). However, earlier eradication of bacterium from the stool was attained (14). In Talkington et al. study, all cases were susceptible to doxycycline and azithromycin. The susceptibility to azithromycin was similar to our study; however, in our study, susceptibility to doxycycline was lower than the result of Talkington study (15). In Pal et al. study, all the strains were similarly susceptible to ampicillin, chloramphenicol, gentamicin, ciprofloxacin and tetracycline. Ogawa biotype was resistant to furazolidone, nalidixic acid and neomycin. However, the results of the study of Pal et al. are considerably different from the results of our study, in terms of susceptibility to ampicillin and tetracycline and, considering the susceptibility to ciprofloxacin and resistance to co-trimoxazole, they were similar (16). In Rahbar et al. study, the researchers studied the V. cholerae epidemic, which occurred in 2005, and showed that all isolated strains were resistant to co-trimoxazole, nalidixic acid and furazolidone. On the contrary, all strains were sensitive to tetracycline, doxycycline, ciprofloxacin, erythromycin and ampicillin (11).
The results of our study show that the resistance to the doxycycline and tetracycline, which are mentioned by multiple authors as the most common antibiotic drugs for treating cholera, is increasing. However, the drug resistance to ciprofloxacin is very low. The results of this study can be used as an evidence to formulate new guidelines for the treatment of cholera.