1. Background
Crimean-Congo hemorrhagic fever (CCHF) is a fatal infectious disease with an average death rate of 50%. The disease is caused by the Nairovirus group from the Bunyaviridae family (1) and is transmitted through the saliva of blood-sucking arthropods (Ixodidae ticks), or by contact with the blood and tissues of infected livestock. Moreover, transmission of CCHF virus from person to person may occur by close contact with infected patients or via nosocomial transmission (1-6). A number of tick genera are capable of becoming infected with the CCHF virus, including Hyalomma spp. and Rhipicephalus spp., but the most common vectors appear to be members of the Hyalomma genus (2, 6, 7).
Crimean-Congo hemorrhagic fever has been reported in 30 countries in Africa, the Middle East, Europe, and Asia (4, 8). It is prevalent in most of Iran’s neighboring countries, including Pakistan, Afghanistan, Russia, Turkey, Iraq, Kazakhstan, Kuwait, Oman, Saudi Arabia, Tajikistan, and the United Arab Emirates (4). Although there had been sporadic reported cases of the disease in livestock and humans since 1970 in Iran, the first reported outbreak occurred in 1999. Since that time, CCHF has been considered one of the country’s major public health challenges (3, 4). Currently, CCHF is prevalent in 23 of 30 provinces of Iran; Sistan-Baluchestan, Isfahan, Fars, and Khuzestan are respectively the most heavily-infected provinces (4).
Due to high fatality rates and many challenges in its treatment, prevention, and control, CCHF is a disease that should be dealt with immediately by public health authorities, so the disease is subject to immediate reporting (9). Health center walk-in patients with symptoms of severe headache, sudden onset of high fever, muscular pain, and bleeding should be immediately suspected for CCHF (9, 10). In probable cases, thrombocytopenia, leukopenia, and leukocytosis are detected in the hematological work-up, and are ultimately diagnosed and confirmed by a seropositive test for CCHF. The incubation period of this disease is 1 - 7 days, and onset of disease is usually sudden (11). In 2002, Khuzestan province was ranked as having the lowest rate of infection, with 10 or fewer cases annually (9). Furthermore, Khuzestan is also included as one of the highest-ranking infected areas on this list, with seven probable cases and five confirmed cases (4, 9).
2. Objectives
This retrospective study was conducted to investigate the epidemiological aspects of CCHF and the determine the disease trend in Khuzestan province in 1999 - 2015.
3. Patients and Methods
This survey is a retrospective descriptive study based on statistics from the Khuzestan health center during 1999 - 2015. Various epidemiological parameters, including the annual prevalence of the CCHF and the victims’ age group, occupation, sex, clinical symptoms, living area (urban or rural), and fatality ratio, were collected from the patient-history documents. The recorded data were analyzed with SPSS software, and the case-fatality rates were determined using the formula below (5).
Fatality rate = (The number of deaths due to CCHF during the specific time / Total cases of disease during specific time) × 100.
4. Results
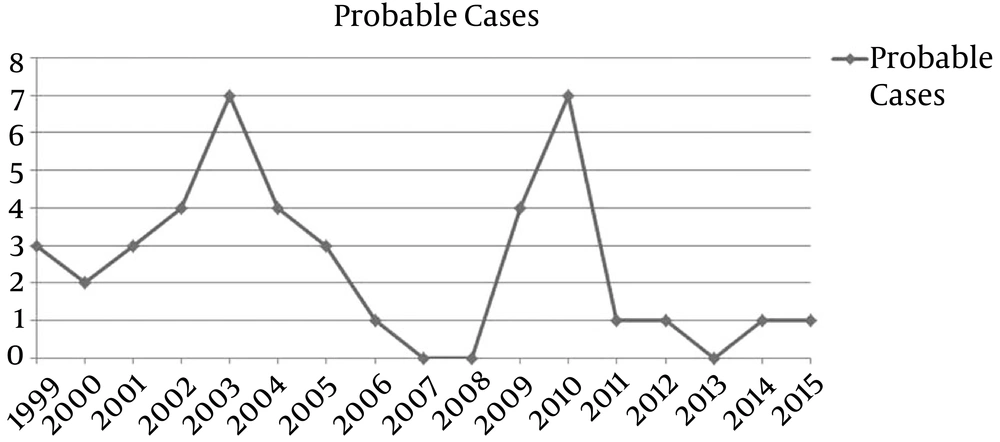
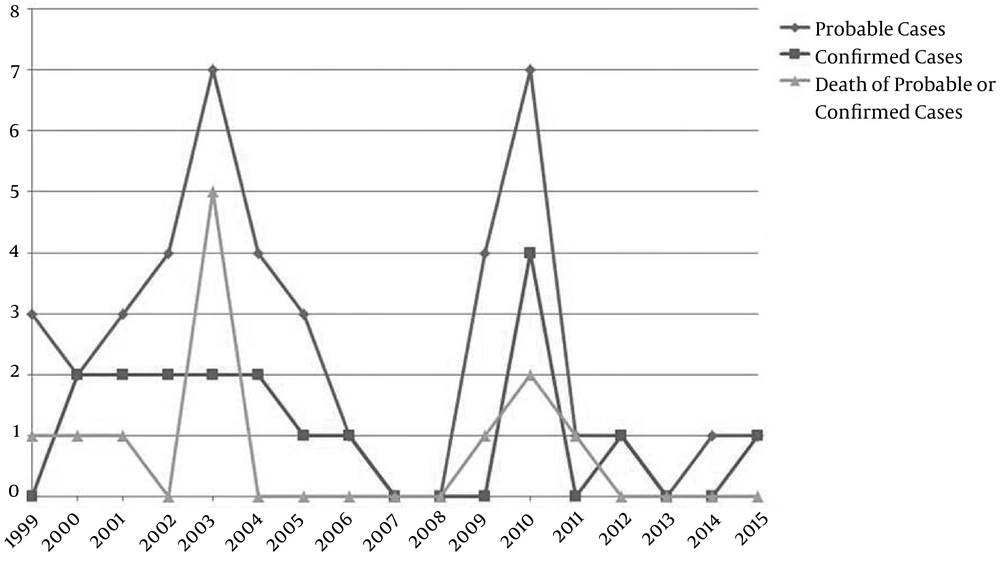
Eighty-one patients with CCHF symptoms were referred to various health centers in Khuzestan province during 1999 - 2015. Among these patients, 42 were diagnosed as probably CCHF-positive with hematological findings positive for thrombocytopenia, of which 17 were confirmed as definite cases with seropositive testing for the CCHF virus. The highest numbers of cases were reported in 2003 and 2010, with seven cases during each of those years; there were five death cases in 2003 compared to two in 2010 (Table 1). However, no CCHF was reported in 2007, 2008, and 2013 (Figures 1 and 2). The annual variations of probable, confirmed, and death cases of CCHF in Khuzestan province during 1999 - 2015 are illustrated in Figures 1 and 2. The most confirmed cases occurred in 2010, whereas the most death cases occurred in 2003, when five out of seven patients died with a probable or confirmed diagnosed.
| Year | No. of Probable Cases (%) | No. of Confirmed Cases | Death of Probable or Confirmed Casesa |
|---|---|---|---|
| 1999 | 3 (7.1) | 0 | 1P |
| 2000 | 2 (4.8) | 2 | 1C |
| 2001 | 3 (7.1) | 2 | 1C |
| 2002 | 4 (9.5) | 2 | 0 |
| 2003 | 7 (16.7) | 2 | 5 (3P and 2C) |
| 2004 | 4 (9.5) | 2 | 0 |
| 2005 | 3 (7.1) | 1 | 0 |
| 2006 | 1 (2.4) | 1 | 0 |
| 2007 | 0 (0) | 0 | 0 |
| 2008 | 0 (0) | 0 | 0 |
| 2009 | 4 (9.5) | 0 | 1P |
| 2010 | 7 (16.7) | 4 | 2C |
| 2011 | 1 (2.4) | 0 | 1P |
| 2012 | 1 (2.4) | 1 | 0 |
| 2013 | 0 (0) | 0 | 0 |
| 2014 | 1 (2.4) | 0 | 0 |
| 2015 | 1 (2.4) | 1 | 0 |
| Total | 42 (100) | 17 | 12 |
aC, confirmed case; p, probable case.
In 95% of the patients, symptoms of fever, bleeding, and thrombocytopenia were detected. Bleeding was not observed in 5% of the patients, and the nose was the most-bleeding organ (Table 2). The prevalence of the disease was 45.2%, 26.2%, 14.3%, and 14.3% in the spring, summer, autumn, and winter, respectively. Of all cases, 57.1% of patients were males and 42.9% were females, and 35.7% of patients lived in rural dwellings compared to 64.3% who were from urban areas. The age groups of 10 - 19 and 20 - 29 years were the highest-risk groups, each with a frequency of 26.2% (Table 3). The occupational groups most often exposed to CCHF were farmers and housewives, with frequencies of 28.6% and 26.2%, respectively (Table 4). The prevalence of this disease was also considerable among students and butchers.
| Bleeding Organ | No. (%) |
|---|---|
| Nose | 28 (66.7) |
| Mouth and gum | 5 (11.9) |
| Hematuria | 4 (9.5) |
| Dysentery or bloody vomit | 2 (4.8) |
| Eye | 1 (2.4) |
| No bleeding | 2 (5) |
| Total | 42 (100) |
| Age, y | Number of Probable CCHF Cases (%) |
|---|---|
| 1 - 9 | 2 (4.8) |
| 10 - 19 | 11 (26.2) |
| 20 - 29 | 11 (26.2) |
| 30 - 39 | 8 (19) |
| 40 - 49 | 7 (16.7) |
| > 50 | 3 (7.1) |
| Total | 42 (100) |
| Occupational Group | Number of Probable CCHF Cases (%) |
|---|---|
| Housewife | 11 (26.2) |
| Farmer | 12 (28.6) |
| Student | 6 (14.3) |
| Butcher | 6 (14.3) |
| Employee | 3 (7.1) |
| Watchman | 1 (2.4) |
| Self-employed | 1 (2.4) |
| Child | 2 (4.8) |
| Total | 42 (100) |
5. Discussion
There have been several reports regarding the prevalence of CCHF in Iran (1-4). However, it is necessary to calculate the disease incidence and trends in provinces with high rates of infection. This information provides a better idea and awareness regarding this disease’s prevalence, and will better illustrate the efficiency of the organizations involved in disease prevention and surveillance programs. Khuzestan province has been ranked as one of the most heavily-infected provinces (4) with seven cases in 2003, of which five led to death. Following this outbreak, the disease demonstrated a downward trend from 2004 until 2008, as there were no reported cases in 2007 and 2008. However, an upward trend was noted again in 2009 and 2010, with seven probable cases reported in 2010; four cases were serologically confirmed and two of them eventually died. The disease followed the same downward trend in Iran from 2000 to 2009 (4), but it followed an upward trend in Turkey during 2002 - 2007 (150 cases in 2002 - 2003 compared to 717 in 2007). In Iran, the highest disease prevalence occurred in 2002 and 2008, with 111 and 120 confirmed cases, respectively; of these, 14 and 19 patients died (3). There were no reported cases in Khuzestan province in 2008.
In this epidemiological survey of Khuzestan province, 42 probable CCHF cases were reported from 1999 to 2015, of which 64.3% were from urban areas and 35.7% were from rural areas. The male:female ratio was 1.3:1.0 and the case-fatality ratio was calculated to be 28.6% (12/42) during this time period. In a similar epidemiological survey of CCHF in Turkey during 2002 - 2007, 1,820 CCHF cases were reported and the fatality ratio was calculated to be 5% (92/1820), of which 69.4% of patients were from rural areas and the male:female ratio was 1.13:1.00 (8). In Iran, 1,638 probable CCHF cases were collected from different provinces from June 2000 until December 2009, of which 635 were confirmed and 89 died (4). Therefore, the fatality ratio was calculated to be 5.4% in Iran during this time period. This ratio has a wide range, 2% - 80%, in different countries (11).
The case-fatality ratio was 28.6% among 38 persons in Mauritania infected with CCHF virus from February to August 2003. The first patient was a young woman who became ill shortly after butchering a goat; she transmitted the infection to 15 hospital health workers and four members of her family (12). In an assessment of patients with CCHF symptoms referred to the Amir-Almoemenin hospital of Zabol county, Sistan- Baluchestan province, southeast Iran, during 2003 - 2005, a total of 65 patients were enrolled. Of them, 52 (80%) were male and 13 (20%) were female. Five patients died (mortality rate 8%). The signs and symptoms included fever (98.4%), headache (80%), myalgia (72.3%), nausea and vomiting (60%), abdominal pain (49.2%), skin rash (13.8%), and splenomegaly (4%). Laboratory findings included thrombocytopenia (100%), leukopenia (70.7%), and anemia (20%) (13).
During the first half of 2009 in Khorasan Razavi province, 13 patients suffered from CCHF, which confirmed the upward trend of the disease compared to the same time in previous years. Four patients were health workers, four were butchers, and the others were farmers (10). In another epidemiological survey from Birjand county, Khorasan province, Iran, a total of 32 probable CCHF patients were hospitalized during 2011 and 2012. Of these, 10 were serologically confirmed. The highest-risk age group was 45 - 50 years. Forty percent of the patients were men and 60% were women. In terms of occupation, 48% of the patients had direct contact with livestock and 70% were from rural areas. In 85% of the cases, the patients had experienced direct contact with livestock and fresh meat. Fever and bleeding were the most common clinical symptoms seen in all of the patients (14).
Eighty-two probable cases were reported in an epidemiological study of CCHF in Fars province during 1999 - 2011, leading to the deaths of 18 patients. Of all patients, 31 were detected as confirmed cases, with nine deaths. Men had the most cases, and the highest-risk occupational groups were farmers, butchers, and slaughterhouse workers. The most cases were reported in summer and spring, which is the ticks’ growing season (15). Two peaks of CCHF were observed in Khuzestan province during 1999 - 2015 (in 2003 and 2010), confirming the probability of re-emergence of the disease. The increased numbers of disease cases in Khuzestan in 2010 were attributed to smuggling of cattle and bufflehead, followed by drought in Pakistan, Afghanistan, and Sistan- Baluchestan. In the last few decades, CCHF has emerged or re-emerged in various countries due to climate and anthropogenic factors, such as land-use changes, agricultural practices, and movement of livestock, which may influence host-tick-virus dynamics (16). Climate changes, unhealthy and illegal slaughter, and smuggling of livestock could also lead to the emergence or re-emergence of the disease, as occurred in many provinces of Iran, including Khuzestan, in 2010.
Finally, considering that the highest-risk occupational groups for CCHF infections are farmers and housewives, and the riskiest age group is 10 - 39 years, these individuals should be instructed and trained with regard to transmission modes, prevention, symptoms, and treatment of CCHF. Particular inspections of veterinary organizations with regard to livestock slaughter and trade, treatment of tick-infested livestock, and training of high-risk groups can help reduce the prevalence of CCHF in Iran.