1. Background
Human immunodeficiency virus (HIV) causes incurable disease of adaptative immunodeficiency syndrome (AIDS), as one of the major global health problems (1, 2). The world health organization (WHO) maintains that more than 35.9 million people worldwide are living with HIV/AIDS (3). The most common sources of morbidity and mortality among HIV-positive individuals at the late stages of the disease when the count of CD4 reaches below 500 µL is opportunistic infections resulted from agents such as fungi that rarely infect immune competent individuals (4). Incidence of opportunistic fungal infections has been progressively increasing in recent years and invasive fungal infections has been reported among 26% of chronically and intensively immunosuppressed patients (5). Infections with Candida albicans (may be the first indication of immunodeficiency), cryptococcal infection, and penicillosis emerge when CD4 count is between 500 – 200 µL, fall below 150 µL, and is less than 100 µL, respectively (6). Candida albicans is a commensal organism that is normally found in the gastrointestinal and reproductive tracts. Under immune compromised conditions, C. albicans can convert from commensal to pathogen and cause symptomatic disease (7). Multi-species oral yeast colonization with inherently drug-resistant organisms is common in HIV infected patients. While C. albicans is the predominant causative agent of all forms of mucocutaneous candidiasis, less frequently members of this genus, notably C. glabrata, C. krusei, C. tropicalis, C. parapsilosi, and C. dubliniensis, have been cited as the causative agents of Oral candidiasis (OC) and isolated in HIV-associated OC (7, 8). Two components of the host immune system as innate and adaptative immune responses work in co-ordination as part of an integrated host immune response to prevent fungal infections (8). A portion of the adaptative immune responses is adaptive T helper (Th) -cell responses, classified as ‘protective’ type-1 (Th1) and ‘non-protective’ type-2 (Th2) (9). Type-1 response which is characterized by the production of Th1 cytokines, such as IFN-γ. These cytokines stimulates the differentiation of CD4 T cells to the Th1 profile, stimulates activation of macrophage and production of opsonizing antibodies and delayed type hypersensitivity. Type-2 response which is characterized by the production of Th2 cytokines, such as IL-4. IL-4 elicits the production of the IgE isotype which is related to allergic reactions and down regulates the Th1 profile (8, 9). IFN-γ, are known to activate phagocytic cells, thus more able to kill Candida. In contrast, the cytokines produced by Th2 cells, such as IL-4, induces alternative macrophage activation (10, 11). TH17 is third subset of effector cell that recently has been identified and characterized by the production of IL-17 (12). Responses of these cells have been implicated in driving protective immune responses against a variety of microbes, including several bacterial and fungal pathogens also IL-17 is probably implicated in the immune pathogenesis of autoimmune responses (13, 14). Mononuclear phagocytic cells are the most important source of IL-6; however, IL-6 is also produced by T and B lymphocytes (15, 16). IL-6 mediates several anti-inflammatory and pro-inflammatory effects, also has been found to serve as a growth factor for the HIV (1).
2. Objectives
Numerous studies have evaluated the effects of HIV and fungal infection on the immune system in vitro and in animal models. To the best knowledge of the present authors, in vivo studies measuring the effects of HIV and fungal infection on cytokine levels in humans have rarely been conducted. Therefore, in this investigation, the levels of IFN-γ, IL-4, IL-6 and IL-17 were measured in HIV-1 infected patients suffering from OC.
3. Patients and Methods
3.1. Study Population and Sampling
This was a cross-sectional study conducted in the department of medical mycology and parasitology between April 2013 and September 2014. This study was approved by ethical committee of Kerman University of Medical Sciences. Written informed consent was obtained from each participant prior to the sample collection. A total of 98 men ranged between 18 - 50 years old referring to Kerman behavioral disorders center (Kerman, Iran) were recruited and evaluated in this study. Subjects were consisted of HIV-positive and HIV-negative persons with and without OC, including HIV-/OC- (control) (n = 32), HIV+/OC- (n = 24), HIV-/OC+ (n = 19) and HIV+/OC+ (23). HIV infection was determined in plasma by ELISA, and confirmed by Western blot, in the Kerman blood transfusion organization, Kerman Iran. The OC lesions were diagnosed on the basis of clinical presentation (white pseudomembranous plaques and/or erythematous areas), findings of direct microscopic examination, and positive culture results (described below). The clinical appearance confirmed by an infectious diseases specialist at center of Behavioral disorders of Kerman Iran. Oral candidiasis-positive had clinically typical visible lesions of oral candidiasis with positive test results for oral Candida colonization. HIV-positive subjects were receiving highly active antiretroviral therapy (HAART) and none of the participant received antifungal drug treatment. Oral swabs of each subject were obtained from tongue or buccal mucosa by using sterile cotton swabs. Samples were collected under complete aseptic conditions and transported immediately to the medical mycology laboratory and processed. Swabs plated on Sabouraud-dextrose agar with chloramphenicol (Merck, Germany) under aerobic conditions at 32°C and in CHROMagar Candida media (CHROMagar, France) in the dark at 35°C for 48 hour to produce species-specific colors and were observed daily for the growth. 10% KOH preparation and Giemsa stain were used for microscopic examination of samples. The diagnosis of OC was confirmed by hyphae being present on a smear and a positive swab culture result that had characteristic colony morphology. Asymptomatic colonization was determined on the basis of the presence of colonies after plate culture but without symptoms or a positive KOH smear result. Chromogenic culture media distinguish C. albicans from other yeast strains on the basis of the color changes produced by the Candida spp colonies. Fresh yeast colonies were processed for germ-tube formation (incubated with rabbit serum at 37°C for 3 hours). Colonies that formed germ tubes were classified as C. albicans. Colonies that not formed germ tube were specified by carbohydrate assimilation tests with RapID™ Yeast Plus System (Remel, USA) according to the manufacturer’s instructions (6). Venus blood (10 mL) was collected in EDTA tubes and stored on ice until isolation of plasma. Plasma was stored at 72°C until use. Plasma concentrations of cytokines were measured by ELISA kits (R and D Systems, USA) according to the manufacturer’s guidelines.
3.2. Statistical Analysis
All statistical analyses were done by SPSS (ver. 20; IBM Inc.). Two-way Analysis of Variance (ANOVA) and Student t-test was performed for the comparison of cytokine levels between groups. P ≤ 0.05 was considered to be statistically significant.
4. Results
Mean of CD4 T cell count in HIV-positive participant were 456 cells/mm3. Out of total 98 samples a definitive diagnosis of OC was made in 42 individual. All participants in this study were male and the mean of age of the study population was 36.5 ± 0.81 years (Table 1).
| Group | Number Of Patients | Mean of Age, y | Sex |
|---|---|---|---|
| HIV+/OC+ | 23 | 39.5 ± 2.72 | Male |
| HIV+/OC- | 24 | 34.3 ± 1.83 | Male |
| HIV-/OC+ | 19 | 40.3 ± 2.92 | Male |
| HIV-/OC- (Control) | 32 | 31.4 ± 1.27 | Male |
| Total | 98 | 36.5 ± 0.81 |
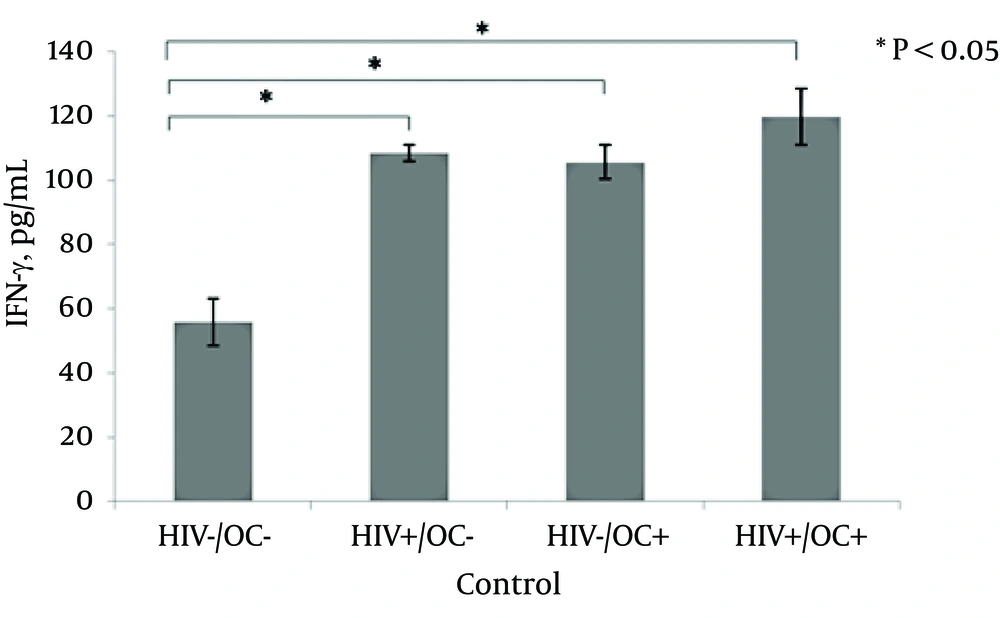
4.1. Effect of HIV and OC on Plasma Concentration of IFN-γ
A two-way ANOVA revealed that a main effect exist for HIV on IFN-γ expression. HIV-positive were significantly more in IFN-γ than HIV-negative ones (P = 0.0001). Also, a main effect for OC on plasma concentration of IFN-γ. Oral candidiasis-positive elicited significantly more IFN-γ than the OC-negative (P = 0.001). There was a significant interaction between OC and HIV in terms of the IFN-γ plasma level (P = 0.005).
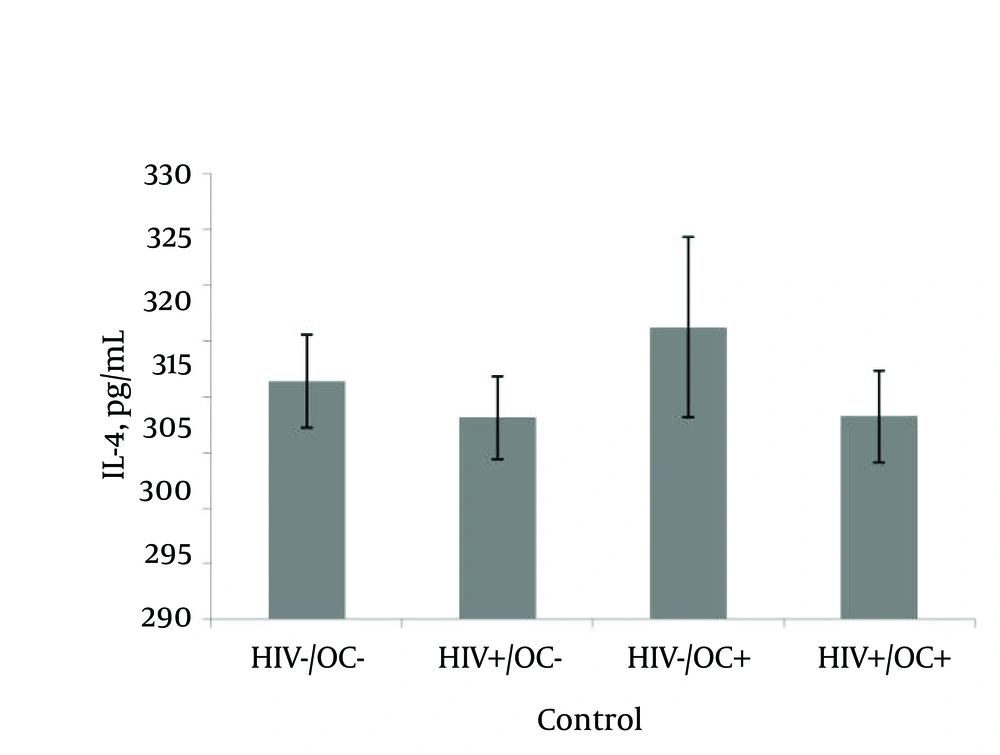
4.2. Effect of HIV and Oral Candidiasis on Plasma Concentration of IL-4
There is no main effect for HIV and OC on plasma concentration of IL-4 (P = 0.24, 0.17, respectively). Also there was not a significant interaction between HIV and OC in terms of IL-4 level (P = 0.28).
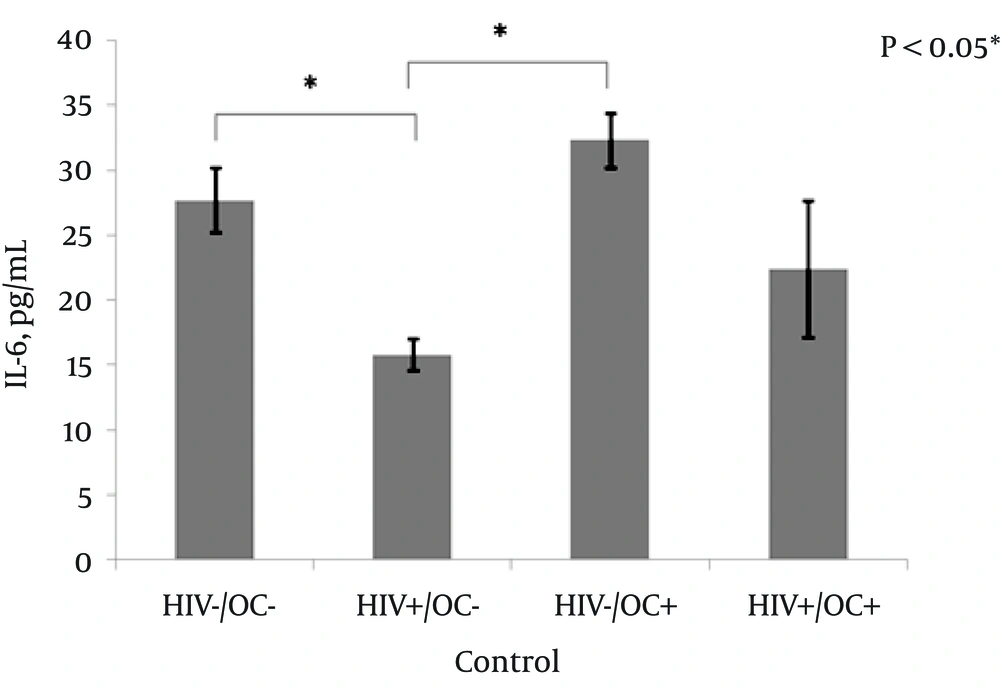
4.3. Effect of HIV and Oral Candidiasis on Plasma Concentration of IL-6
There was a main effect for HIV on IL-6 expression. HIV-negative were significantly more in IL-6 than HIV-positive ones (P = 0.0001). But, not a significant effect for OC on plasma concentration of IL-6 (P = 0.65). Additionally, there was a significant interaction between HIV and OC in terms of the level of IL-6 (P = 0.001).
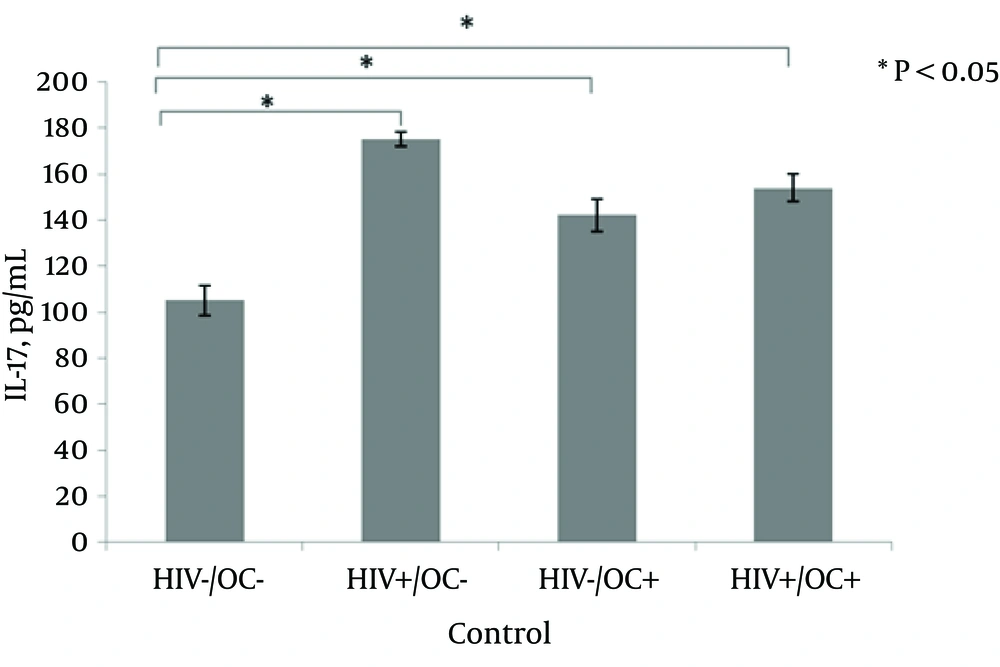
4.4. Effect of HIV and Oral Candidiasis on Plasma Concentration of IL-17
There was a main effect for HIV on IL-17 expression. HIV-negative were significantly lower in terms of IL-17 than HIV-positive ones (P = 0.001). Also, a main effect of OC on plasma concentration of IL-17. OC-positive elicited significantly more IL-17 than Oral Candidiasis-negative (P = 0.03). There was a significant interaction between HIV and OC in terms of the expression of IL-17 (P = 0.0001).
4.5. Plasma Concentration of Cytokines
Analysis of plasma cytokine levels of HIV+/OC+, HIV+/OC-, HIV-/OC+ and HIV-/OC revealed changes in the cytokine profiles. IFN-γ and IL-17 levels were determined to be statistically increased in HIV+/OC+, HIV+/OC- and HIV-/OC+ patients compared with the healthy controls (HIV-/OC-) (P = 0.03, P = 0.001, P = 0.0001, P = 0.01, P = 0.0001, P = 0.0001, respectively; Figure 1 and 4). IL-6 levels were determined to be statistically decreased in HIV+/OC- compared with HIV-/OC+ and HIV-/OC- (P = 0.001, P = 0.005, respectively; Figure 3). There was no significant difference in IL-4 level between groups (Figure 2).
5. Discussion
In the present study, we evaluated the effects of HIV and Candida infection on cytokine levels and the plasma concentration of IL-4, IL-6, IL-17 and IFN-γ were measured as well. The present findings demonstrated that the levels of IFN-γ in the plasma of patients with OC were significantly higher than those without OC. Also, the levels of this cytokine in HIV-positive individuals were significantly higher than HIV-negative cases. Interesting, according to the findings of this study, in patients without OC, the shift to OC+ would cause significant increase in the levels of IFN-γ in both HIV-positive and HIV-negative patients with different slops. The increased levels of IFN- γ suggest that inflammatory processes are enhanced. Results related to IFN-γ have been controversial, since both increase and decrease have been reported (17). Previous studies have also demonstrated that fungal infection and/or HIV infection can affect IFN-γ production. Lilly et al. showed HIV-positive subjects with or pharyngeal candidiasis (OPC) changes in the levels of most tissue-associated cytokines. These included increased levels of IFN-γ (18). Shellito et al. (19) assayed cytokine production by CD4+T cells of normal mice challenged with Pneumocystis and showed a rapid increase in CD4+T cells that produced IFN-γ. Fatahinia et al. (20) showed propolis treatments alone suppressed IFN-γ in the sera of mice when compared with old mice that receiving propolis altogether with C. albicans. IL-4 is a Th2 cytokine which is predominantly produced by activated CD4+ T cells. It is also produced by NK cells, mast cells, and basophils and stimulates activation and differentiation of B-cell, secretion of IgG1 and IgE, activation of T cell, and MHC II expression on B cells. Macrophages seem to play a protective role in the mouse model of OC, since neutralization of IL-4 results in the delayed clearance of fungi (13). According to the results of the present study, OC and HIV infection could not alter the plasma concentration of IL-4, as the level of this cytokine in patients compared to non-infected controls were not showed significantly different. Several studies have demonstrated that the increased secretion of IL-4 is related to in vivo HIV-1 infection. However, there are conflicting reports on the effect of HIV-1 infection on IL-4 production and also reduced or normal IL-4 levels have also been reported in HIV-infected individuals (21). Increased IL-4 and IL-5 mRNA levels in C. albicans antigen-activated peripheral blood mononuclear cells (PBMC) from HIV-infected patients with OPC indicated a shift from a Th1 profile to a less polarized and protective Th2/Th0 profile in HIV-infected group of patients, especially the ones that underwent C. albicans infection. Therefore, in HIV or other immunosuppressive diseases in which an increased level of IL-4 is observed, fungal infection can cause life-threatening diseases (21). IL-6 stimulates the acute phase response (innate immunity) and promotes B-cell proliferation (adaptive immunity). Monocytes, macrophages, T lymphocytes, endothelial cells and fibroblast are the source of this cytokine (22). As mentioned in literatures, IL-6 acting as a growth factor for HIV (encourage HIV replication and proliferation) and compared to healthy individuals be elevated in HIV infection (1). Also have revealed that this cytokine enhances resistance to invasive aspergillosis and candidiasis in mice (16). This experiment did not detect any evidence for effect of OC on IL-6 plasma concentration and OC+ was not significantly altering IL-6 than the OC- subjects. On the other hand HIV significantly alters the plasma level of IL-6. As HIV-negative were significantly more in IL-6 than HIV-positive ones. In other words, HIV reduced the plasma concentration of IL-6. In HIV-negative and HIV-positive patients following shift from OC- to OC+, plasma concentration of IL-6 elicited not significantly. This finding confirms the significant interaction between OC and HIV in terms of the level of IL-6. Th17 cells are a recently identified subtype of CD4+ T cells that respond fungal antigens and are important in mucosal immunology also because HIV infection results in loss of CD4+ T, Th17 cells potentially play an important role in HIV pathogenesis (23). Studies have shown a role for IL-17 in immunity against extracellular pathogens and shown that Th17 cell activation promoted deleterious inflammation and defective fungal clearance in pulmonary aspergillosis and gastrointestinal candidiasis (24). In mice, deficiency of IL-17 causes increased susceptibility to disseminated candidiasis (25, 26). Therefore expected that IL-17 levels rise in fungal infections. Results of this study showed OC significantly elicited plasma concentration of IL-17 in HIV-negative subjects while, in HIV-positive patients OC decreased plasma level of this cytokine. Results of studies on IL-17 levels in HIV infection is different as to whether IL-17 are increased, decreased, or not affected in plasma after HIV infection (27, 28). For instance, one study has shown that in HIV-infected children there was a significant loss of IL-17 producing PBMC (29). In contrast to these findings, the results of our study showed HIV-negative were significantly lower in terms of IL-17 than HIV-positive ones. According to the results presented here, it appears that IL-17 play significant roles in defense against OC because it was more increased in OC patients in comparison to OC negative subjects than other cytokines. Based on the fact that IL-17 is the first line of adaptive immune responses against infections, hence, it appears that adaptive immunity of HIV positive patients also follows this pattern. This study is the first to have evaluated plasma concentration cytokine in plasma of HIV-1 patients suffering from OC in a clinical setting. Key finding of the present study was that fungal infection and HIV alone and together could seriously alter immune system function as assessed by measuring the levels of the plasma cytokines. Therefore, these results provide important new information relative to the putative immune-based factors associated with resistance and/or susceptibility to OC in HIV-positive persons. However, more research on this topic needs to be undertaken before the association between immune system response and opportunistic fungal infections in HIV-positive patients.