1. Background
In recent years, Acinetobacter baumannii has emerged as an important pathogen in nosocomial infections and especially infects critically ill patients admitted to the intensive care units (ICUs) (1, 2). Septicemia, pneumonia, urinary tract infection, wound infection and meningitis are among the infections caused by this pathogen (3). In the hospital environment, resistance of A. baumannii to antimicrobial agents raises concerns (4). Carbapenem resistant A. baumannii are great concerns for physicians because carbapenems are common choice to treat infections caused by this pathogen (4, 5). In addition, therapeutic efficacy of carbapenems is limited due to spread of carbapenem resistant A. baumannii (4, 6). Carbapenem resistance is now observed worldwide in A. baumannii and these isolates are usually resistant to all classes of antimicrobial agents. A plenty of outbreak due to carbapenem resistant A. baumannii are reported from different countries and this situation had a worrying trend (4). Carbapenem resistance in A. baumannii is mediated by combined different mechanisms including: reduced permeability, changes in penicillin binding protein, AmpC stable derepression, efflux pumps and mostly by production of oxacillinases (OXAs) and less common by metallo-β-lactamase (MBLs) genes (7-9). Clonal transmission of drug resistant A. baumannii is reported globally (10). Inter hospital transmission of carbapenem resistant A. baumannii is demonstrated (4). It is well documented that in the nosocomial outbreaks, in most of the cases, one or two epidemic clones are involved in a given hospital (4). For epidemiological purposes and to control the spread of resistant iaolates, rapid diferrentiation of epidemic strains from the numerous incidental strains is necessary (11, 12). Molecular typing such as repetitive sequence-based polymerase chain reaction (rep-PCR) is required to determine the clonal relatedness of A. baumannii (12). The rep-PCR is beneficial for the molecular typing of A. baumannii (11).
2. Objectives
The current study aimed to determine the antimicrobial susceptibility pattern, prevalence and types of oxacillinase and metallo-β-lactamase genes and molecular typing by rep-PCR in the clinical isolates of A. baumannii.
3. Materials and Methods
3.1. Collection and Identification of Acinetobacter baumannii Isolates
From July 2011 to January 2013, a total of 124 non-duplicated A. baumannii isolates were collected from various clinical specimens in two teaching hospitals in Ahvaz, south-est of Iran. Bacterial isolates were initially identified as A. baumannii by biochemical tests (13). Suspected isolates were confirmed by PCR to identify blaOXA-51-like gene with specific primers (listed in Table 1) to amplify a 353 base pair sequence (14). DNA template for PCR was obtained by boiling method (15). Each reaction was carried out in a final volume of 25 µL containing 1x PCR buffer, 1 U Taq polymerase, 1.5 mM MgCl2, 200 µM of dNTP (SinaClon, Iran), 10 pmol of each primer (Eurofins MWG Operon, Germany) and 1 µL of the extracted DNA. PCR conditions were programmed in Mastercycler Eppendorf (Eppendorf, Germany) as follows: Initial denaturation at 94°C for 3 minutes; 35 cycles of 94°C for 45 seconds, annealing 57°C for 45 seconds, extension 72°C for 1 minute and final extension 72°C for 5 minutes. PCR products were separated on 1.5% agarose gel (SinaClon, Iran) by electrophoresis, stained with ethidium bromide (SinaClon, Iran) and then visualized under UV illumination (Syngene GeneGenius gel documentation system). Acinetobacter baumannii ATCC 19606 was used as positive control (14).
| Primer | Forward Sequence 5’ - 3’ | Reverse Sequence 5’ - 3’ | Reference |
|---|---|---|---|
| blaOXA-51-like | TAATGCTTTGATCGGCCTTG | TGGATTGCACTTCATCTTGG | (14) |
| blaOXA-23-like | GATCGGATTGGAGAACCAGA | ATTTCTGACCGCATTTCCAT | (16) |
| blaOXA-24-like | GGTTAGTTGGCCCCCTTAAA | AGTTGAGCGAAAAGGGGATT | (16) |
| blaOXA-58-like | AAGTATTGGGGCTTGTGCTG | CCCCTCTGCGCTCTACATAC | (16) |
| blaIMP | TCGTTTGAAGAAGTTAACGG | ATGTAAGTTTCAAGAGTGATGC | (17) |
| blaVIM | GGTGTTTGGTCGCATATCGCAA | ATTCAGCCAGATCGGCATCGGC | (17) |
| blaSPM | AAAATCTGGGTACGCAAACG | ACATTATCCGCTGGAACAGG | (18) |
| REP | REP-I, III: GCGCCGICATCAGGC | REP-II: ACGTCTTATCAGGCCTAC | (19) |
Sequence of Primers Used in the Study
3.2. Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing of all isolates was performed using Kirby-Bauer method according to the clinical and laboratory standard institute (CLSI, 2011) guidelines. The following antimicrobial agents were tested: imipenem 10 µg, meropenem 10 µg, polymyxin-B 300 U, gentamicin 10 µg, ceftriaxone 30 µg, colistin 10 µg, piperacillin 100 µg, piperacillin-tazobactam 100/10 µg, cefepime 30 µg, tobramycin 10 µg, amikacin 30 µg, tetracycline 30 µg, ciprofloxacin 5 µg, trimethoprim-sulfamethoxazole 1.25/23.75 µg, ceftazidime 30 µg, rifampin 5 µg, tigecycline 15 µg, aztreonam 30 µg and ampicillin-sulbactam (10/10 µg), (MAST, Group Ltd, Merseyside, UK). Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were used as control strains (20). Minimum inhibitory concentration (MIC) of imipenem, meropenem, colistin and tigecycline were determined by E-test strips (Liofilchem, Italy). Measures were obtained according to the CLSI guidelines. The US food and rug drug administration-approved criteria and Jones criteria were used for Enterobacteriacea and tigecycline breakpoint, respectively (21, 22).
3.3. Screening the metallo-β-Lactamase Producing Isolates
All isolates were screened for MBL production by an imipenem-EDTA (ethylene diamine tetra-acetic acid) double disk synergy and E-test MBL. Briefly, an overnight culture suspension of each sample was adjusted to a turbidity equivalent to 0.5 McFarland and inoculated on the surface of a Mueller-Hinton agar plate. Two 10 µg of imipenem disk (MAST, Group Ltd, Merseyside, UK) were placed on the plate 10 mm apart from edge to edge. Then 10 µL of 0.5 M EDTA solution (SinaClon, Iran) was directly added to one of them to obtain the desired concentration (750 µg). The plates were incubated at 35°C for 18 hours. After incubation, inhibition zones of the imipenem and imipenem-EDTA disks were measured and compared. If enlarged zone with imipenem-EDTA was 7 mm greater than the imipenem disk alone, it was considered as MBL positive revealing the inactivation of metallo-β-lactamase (class B) activity by EDTA (23, 24). Also an E-test MBL strip containing a double sided seven dilution range of imipenem (4 to 256 µg/mL) and imipenem (1 to 64 µg/mL) in combination with a fixed concentration of EDTA (Liofilchem, Italy) was used. The results were interpreted according to the manufacturer’s instruction.
3.4. PCR Amplification of OXA and Metallo-β-Lactamase Genes
Multiplex PCR was performed to detect blaOXA-23-like, blaOXA-24-like and blaOXA-58-like using specific primers as previously described (16). DNA template was obtained by boiling method (15). Each PCR reaction was performed in a final volume of 25 µL with 1x PCR buffer, 1 U Taq polymerase, 2 mM MgCl2, 200 µM of dNTP (SinaClon, Iran), 0.2 µM of each primer (TAG, Copenhagen A/S Denmark) and 1 µL of template DNA. PCR conditions were programmed in Mastercycler Eppendorf (Eppendorf, Germany) as follows: Initial denaturation at 94°C for 5 minutes; followed by 30 cycles at 94°C for 30 seconds, 53°C for 40 seconds and 72°C for 50 seconds and final extension at 72°C for 6 minutes. PCR products were separated by electrophoresis on 1.5% agarose gel (SinaClon, Iran) and after staining with ethidium bromide, visualized under UV gel documentation system Acinetobacter baumannii reference strains including: NCTC 13304, NCTC 13302, NCTC 13305 were used as positive control for blaOXA-23-like, blaOXA-24-like and blaOXA-58-like, respectively (16). For each gene, one amplicon was sequenced (Bioneer, South Korea) blaVIM, blaIMP and blaSPM were sought by singleplex PCR and primers previously described (17, 18). Two clinical isolates of P. aeruginosa harbored blaIMP and blaVIM were sequenced using automated sequence analyzer (Bioneer, South Korea) and used as positive control to identify the genes. The DNA of blaSPM-positive P. aeruginosa was purchased from Pasteur Institute of Iran and used as positive control in PCR reactions.
3.5. The rep-PCR
To investigate genotyping and identification of various clones, all isolates were subjected to rep-PCR with emphasis on carbapenem resistant isolates. Specific primers were used according to the previously described Bou et al. protocol (19). Template for PCR was extracted by phenol-chloroform method. Each reaction mixture was done in the total volume of 25 µL with 1x PCR buffer, 3.5 mM of MgCl2, 300 µM of dNTP, 3% dimethyl sulfoxide (DMSO) (SinaClon, Iran), 0.5 µM of each primer (TAG, Copenhagen A/S, Denmark), and 1U of Taq polymerase and 1 µL of genomic DNA. Amplification conditions were as follows: 94°C for 10 minutes; 30 cycles of 94°C for 1 minute, annealing temperatures 45°C for 1 minute, 72°C for 2 minutes and 72°C for 16 minutes. Products were separated by electrophoresis on 1.2% agarose gel (SinaClon, Iran); after staining with ethidium bromide, they were visualized under UV gel documentation system; then they were photographed and compared together by visual inspection (19). All fingerprints were observed by one observer. Snelling et al. protocol was used for classified various clones (11).
3.6. Nucleotide Sequence Accession Number
The nucleotide sequences obtained in this study were submitted to the GenBank nucleotide sequence database under the accession numbers: HG937619 for blaOXA-23-like, HG937620 for blaOXA-24-like and HG937621 for blaOXA-51-like.
3.7. Statistical Analysis
The results were analyzed using the SPSS version 16 to obtain frequencies and comparison among clones. Non-parametric chi-square test was used. A P value < 0.05 was considered statistically significant.
4. Results
4.1. Bacterial Isolates
Totally, 124 single-patient isolates were recovered. All isolates were positive for blaOXA-51-like and identified as A. baumannii. The rate of isolates from each ward and specimen are shown in Table 2.
| Ward | Rate of Isolates | Specimen | Rate of Isolates |
|---|---|---|---|
| ICU | 74.2 | Tracheal aspirate | 57.3 |
| Out patients | 8.1 | Cerebrospinal fluid | 11.3 |
| Neurosurgery | 4 | wound | 10.5 |
| Dermatology | 4 | Urine | 8.1 |
| Nephrology | 3.2 | Discharge | 5.6 |
| Orthopedic | 2.4 | Blood | 3.2 |
| Woman | 2.4 | Pleura | 1.6 |
| Surgery | 0.8 | Catheter | 1.6 |
| Neonatal | 0.8 | Eye infection | 0.8 |
The Rate of Acinetobacter baumannii Species Isolated From Each Ward and Specimen
4.2. Antimicrobial Susceptibility
The results of antimicrobial susceptibility test by disk diffusion method are shown in Table 3. Colistin and polymyxin-B were the most active agents against the tested isolates. According to the results of MICs by E-test, among 124 isolates, 97 (78.2%) were resistant to imipenem. However, meropenem resistance was observed in 91 (73.4%) of the studied isolates. Only one isolate (0.8%) was resistant to colistin and 123 isolates (98.2%) were susceptible to this antibiotic. No tigecycline resistant isolate was observed and 99 (79.8%) and 25 (20.2%) isolates were sensitive and intermediate to this antibiotic, respectively.
| Antibiotic | Sensitive | Intermediate | Resistant |
|---|---|---|---|
| Imipenem | 24.2 | 1.6 | 74.2 |
| Meropenem | 19.4 | 0.8 | 79.8 |
| Ceftazidime | 15.3 | 2.4 | 82.3 |
| Cefepime | 16.1 | 4 | 79.8 |
| Ceftriaxone | 1.6 | 12.1 | 86.3 |
| Colistin | 98.2 | NA | 0.8 |
| Piperacillin | 12.1 | 3.2 | 84.7 |
| Piperacillin-tazobactam | 16.9 | 1.6 | 81.5 |
| Polymyxin-B | 100 | NA | NA |
| Gentamicin | 28.2 | 4.8 | 66.9 |
| Tobramycin | 33.9 | 1.6 | 64.5 |
| Amikacin | 21 | 12.1 | 66.9 |
| Tetracycline | 21.8 | 12.1 | 66.1 |
| Ampicillin-sulbactam | 32.3 | 21.8 | 46 |
| Ciprofloxacin | 13.7 | 1.6 | 84.7 |
| Trimethoprim-sulfamethoxazole | 19.4 | 4.8 | 75.8 |
| Rifampin | NA | 3.2 | 96.8 |
| Aztreonam | NA | 4.8 | 95.2 |
| Tigecycline (FDA) | 6.5 | 58.1 | 35.5 |
| Tigecycline (Jones) | 45.2 | 50.8 | 4 |
The Results of Antibiogram Analysis of Acinetobacter baumannii Isolatesa
4.3. PCR Amplification of OXA Genes
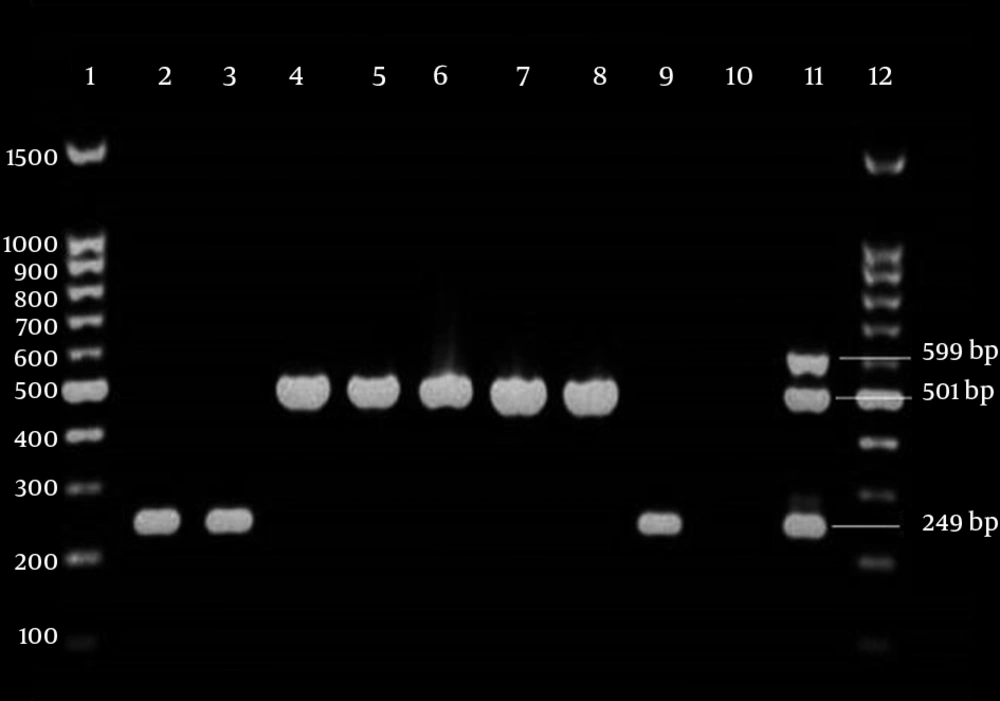
Multiplex PCR analysis identified blaOXA-23-like in 83 (85.6%) of carbapenem resistant isolates. Six isolates (6.2%) contained blaOXA-24-like (Figure 1). All isolates were negative for blaOXA-58-like. Eight isolates were carbapenem resistant but had only blaOXA-51-like and other studied isolates were negative in the other studied genes. No amplification products were obtained in carbapenem susceptible isolates.
Lanes 1 and 12, 100 bp DNA ladder; lanes 2, 3 and 9, isolates with blaOXA-24-like in 249 bp; lanes 4 - 8, isolates with blaOXA-23-like in 501bp; lane 10, negative control (distilled water). lane 11, positive control Acinetobacter baumannii NCTC 13304, NCTC 13302 and NCTC 13305 were used as positive controls for blaOXA-23-like, blaOXA-24-like and blaOXA-58-like, respectively.
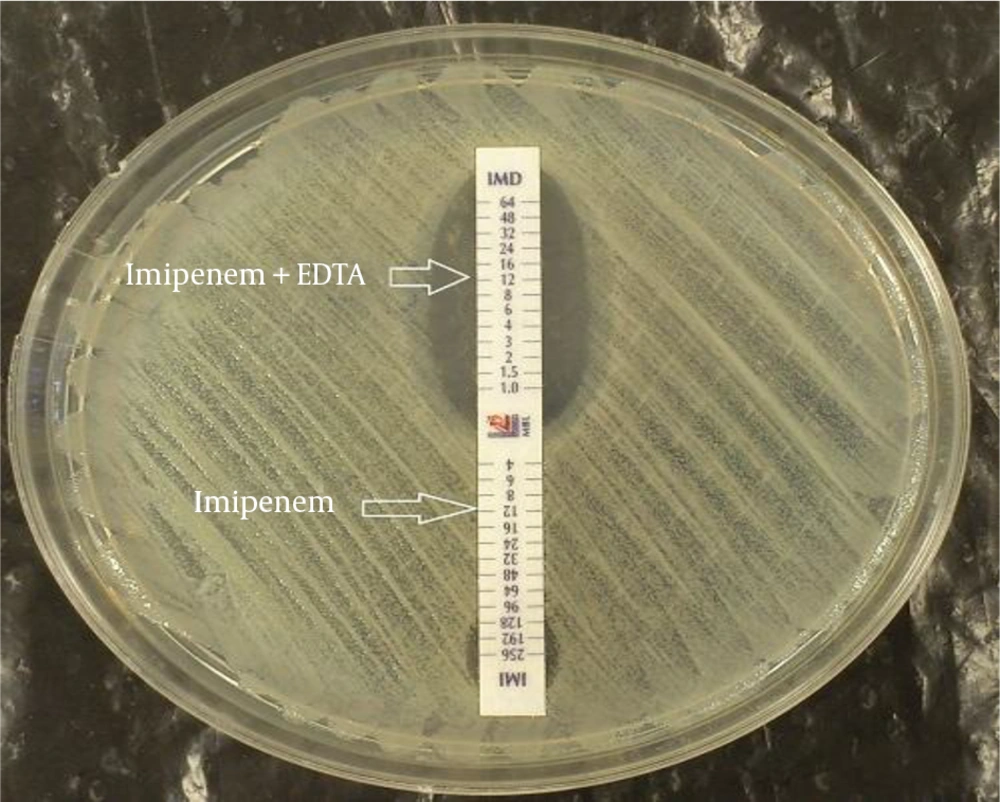
4.4. Metallo-β-Lactamase E-Test
To study the MBL production, carbapenem resistant isolates were evaluated by double disk synergy (DDS) test and E-test MBL strips. Of the 97 carbapenem resistant isolates, 41 (42.3%) exhibited a > 7 mm inhibitory zone and were categorized as MBL producer. However 56 isolates (57.7%) were negative for MBL production. Results of MBL E-test showed that among 97 carbapenem resistant isolates, 77 (79.4%) were positive for metallo-β-lactamase production and 20 isolates (20.6%) were negative (Figure 2). PCR did not detect metallo-β-lactamase genes, including blaVIM, blaIMP and blaSPM, among the studied isolates.
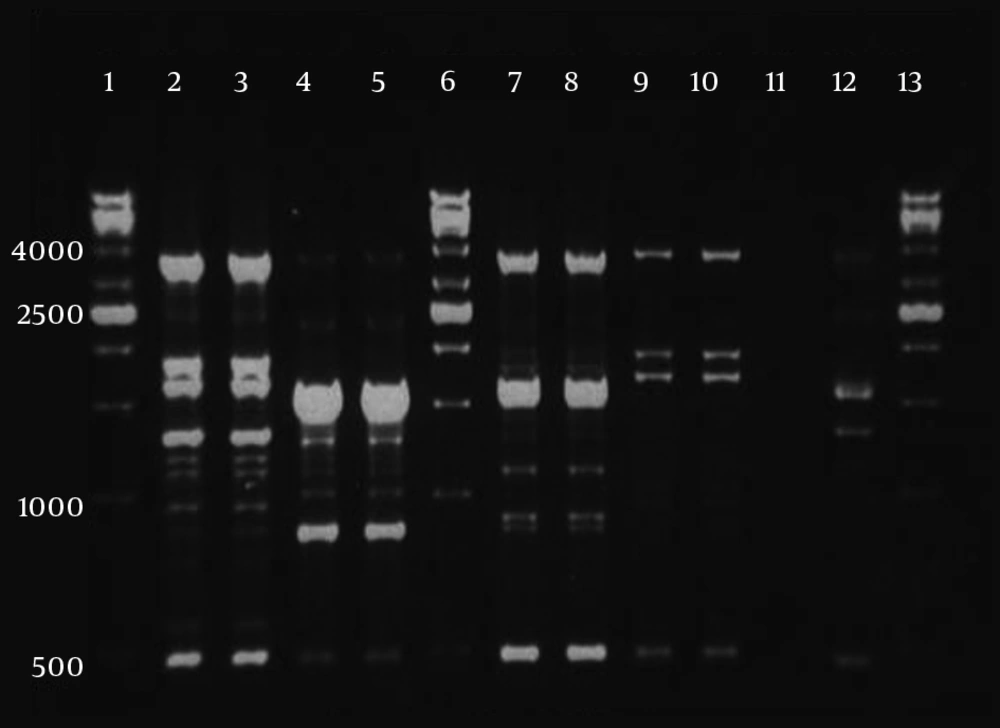
4.5. REP PCR
Among carbapenem resistant isolates, six clones (A - F) were observed which three of them were more prevalent (Figure 3). Genotype A was the most prevalent (P value < 0.001) and 30.9% (30 isolates) belonged to this genotype. The prevalence of other genotypes were as follows: 28 isolates (28.9%) belonged to clone B, 26 isolates (26.8%) to clone C, 10 isolates (10.3%) to clone D and 2 isolates (2.1%) to clone E. Clone F contained only one isolate (1%). Carbapenem susceptible isolates (27 isolates) had unique genotypes.
5. Discussion
In the current study most of the isolates (74.2%) were obtained from patients in ICUs and in accordance to other researches worldwide, the rate of infection caused by A. baumannii is high in ICUs (25, 26). Previously, it was reported that A. baumannii is more prevalent among endotracheal aspirate samples. Moreover, ventilator associated pneumonia is one of the frequent nosocomial infections caused by this organism (27-31). In accordance to the mentioned studies, most of the current study samples (57.3%) were isolated from tracheal aspirates. In the present study, antimicrobial susceptibility pattern showed that colistin and polymyxin-B are the most effective agents against A. baumannii isolates, in vitro. Colistin is the last line antimicrobial agent to treat multidrug resistant A. baumannii (26, 32). Although, colistin resistant isolates are reported globally (32), in the current study only 0.8% of isolates were colistin resistant.
This result indicates that colistin can be used to treat A. baumannii infections in the studied hospitals. Afterwards, among the tested antimicrobial agents, the highest rate of resistance was observed against rifampin; 96.8% and 3.2% of the isolates were resistant and intermediate to this antibiotic, respectively. No isolate was sensitive to rifampin; hence, it is suggested t that rifampin might be ineffective to treat A. baumannii infections in the studied hospitals. Carbapenems are successfully used to treat multidrug resistant A. baumannii infections; however, in recent years increase of carbapenem resistant A. baumannii isolates compromised their use (4, 26, 33). The emergence of carbapenem resistant A. baumannii is a global concern (4). In the current study the rates of resistance to imipenem by E-test and disk diffusion method were 78.2% and 74.2%, respectively. In addition, 79.8% and 73.4% of the isolates were resistant to meropenem by disk diffusion and E-test, respectively.
There is a discrepancy between carbapenems E-test and disk diffusion method. Based on E-test, 78.2% of the isolates were resistant to imipenem; while disk diffusion method showed that 74.2% of the isolates were resistance to imipenem. In contrast, meropenem E-test detected 73.4% of isolates as resistant; whilst, according to disk diffusion more isolates (79.8%) were recorded as meropenem resistant. However, authors could not elucidate this difference. In A. baumannii, the most common carbapenemase genes involved in carbapenem resistance are, blaOXA-23-like, blaOXA-24-like, blaOXA-58-like and blaOXA-143-like (26, 34). In the current study, multiplex PCR detected 85.6% of carbapenem resistant isolates carrying blaOXA-23-like. The spread of OXA genes varies in different parts of the world and blaOXA-23-like is reported from 31% to 94% (7, 12, 35-39). The current study found that 6.2% of carbapenem resistant isolates harbor blaOXA-24-like. Some authors worldwide, reported the rate of blaOXA-24-like from 0 to 85.43% (7, 33, 36, 38-40).
The results of the current study were consistent with those of other studies and the findings for blaOXA-23-like and blaOXA-24-like were in the reported ranges. In contrast to other studies that reported the range of blaOXA-58-like from 2% to 84.92% (12, 35-38, 40), the current study could not find any isolates positive for blaOXA-58-like. Albeit the reported co-existence of OXAs genes (29, 41, 42), coexistence between these genes was not observed in the current study and all A. baumannii isolates only had one of the blaOXA-23-like or blaOXA-24-like genes. In the current study, 42.3% and 79.4% of the isolates were MBL positive by DDs test and MBL E-test, respectively. Despite phenotypic tests, no blaIMP, blaVIM and blaSPM genes were detected by PCR and the isolates were negative for these genes. There are some possibilities about this phenomenon: 1) the MBL production may be false positive and due to bactericidal activity of EDTA, which may result in increased inhibitory zone and not associated with true MBL production (43); 2) MBL production my be true positive due to other MBL genes such as blaNDM that were not investigated in the current study (44). Similar results are reported that A. baumannii isolates were MBL producer by phenotypic tests but no MBL encoding genes were detected (45, 46).
It is reported that MBL E-test has good sensitivity for MBL detection and could detected MBL both chromosomally and plasmid mediated in aerobic and anaerobic bacteria (47). According to the E-test results, it is possible that the current study isolates were true MBL producers. Interestingly the study found eight carbapenem resistant isolates that were negative for blaOXA-23-like, blaOXA-24-like, blaOXA-58-like and MBL genes and only harbored blaOXA-51-like. Similarly, Nowak et al. reported that seven isolates of carbapenem resistant A. baumannii only had blaOXA-51-like (29). Carbapenem resistance in these isolates may be associated with other mechanisms such as: modification of penicillin binding proteins, loss of porins and decreased permeability, AmpC stable derepression or over expression of efflux pump (4, 8, 9). It is noteworthy that, insertion of ISAba1 in upstream of blaOXA-51-like can lead to caebapenem resistance in A. baumannii (48).
The relationship between harboring blaOXA-51-like and resistance to carbapenem in the eight isolates still need to be investigated. The current study also aimed to investigate the clonality of A. baumannii isolates by rep-PCR. Genotypic comparison by rep-PCR revealed that carbapenem resistant isolates belonged to six clones. All clones were spread in the ICUs. Clone A was dominant (30.9%) and clone F had the lowest prevalence (1%). Clonal dissemination of carbapenem resistant A. baumannii was previously reported in different studies. It has been establish that multidrug resistant of A. baumannii isolates with similar genotype can disseminate among various wards, different hospitals and even among cities (4, 10, 12, 49-51). In the current study, the vast majority of carbapenem resistant isolates (94/97, 96.9%) belonged to one of the four dominant genotypes indicating clonal dissemination of resistant isolates in the studied hospitals.
In conclusion, overall, the rate of carbapenem resistant isolates were high in the studied hospitals. Colistin and polymyxin-B were the effective antimicrobial agents, in vitro. Since in the current study blaOXA-58-like or MBL genes were not detected, it seems that carbapenem resistance is mostly related to blaOXA-23-like and blaOXA-24-like, and these genes may play an important role in carbapenem resistance in the isolates. In addition, four clones of carbapenem resistant of A. baumannii isolates are disseminated in the two studied hospitals and clone A was dominant. In accordance to other studies, in the current investigation most of the resistant isolates belonged to four clones indicating clonal dissemination of A. baumannii in the studied hospitals and that effective infection control strategies are necessary to control the spread of these resistant isolates.