1. Introduction
Intra-abdominal abscesses generally develop as a result of abdominal surgery, intra-abdominal pathologies (e.g. diverticulitis, appendicitis, biliary disorders, pancreatitis, and organ perforations), or penetrating abdominal trauma. Abscesses caused by infectious bacteremia reaching the abdomen from a distant focus are very rare (1).
The Streptococcus anginosus group of bacteria, formerly called the S. milleri group, has three members: S. intermedius, S. constellatus, and S. anginosus. These microorganisms are low-virulence bacteria existing as commensals in the oral flora and gastrointestinal tracts of humans (2). S. anginosus may spread to the blood in individuals with poor oral hygiene in cases of oral infections, such as gingivitis and tooth abscesses, that develop following the loss of mucosal unity. This may lead to infections throughout the body, primarily as brain and liver abscesses. While similar cases are more prevalent among patients with immunodeficiency and underlying gastrointestinal tract pathology, they also occur in immunocompetent patients, although rarely (2). This paper describes a case of intra-abdominal abscess and primary peritonitis caused by S. anginosus, which is very rare and was considered to have been caused by oral flora in an immunocompetent patient.
2. Case Presentation
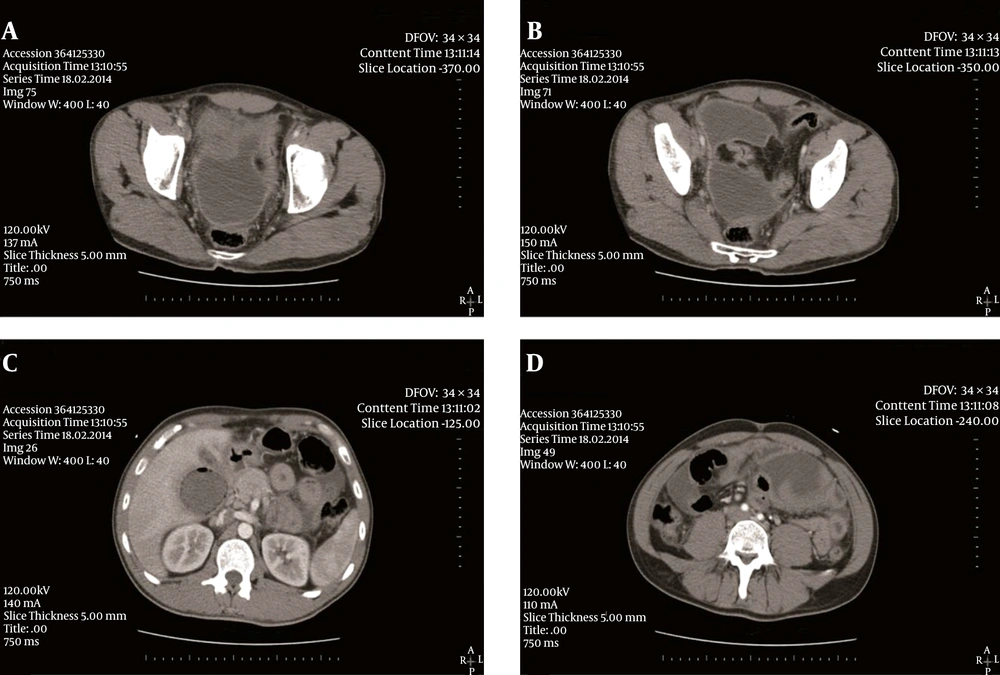
A 32-year-old male patient presented to the emergency department with complaints of nausea, vomiting, and diffuse abdominal pain in all quadrants, especially in the epigastrium. On physical examination, diffuse abdominal tenderness and rebound tenderness were detected, particularly in the epigastrium and right upper quadrant. Laboratory assessment revealed a leukocyte count of 20,500/mm3 with 85% polymorphonuclear leukocytes (PNLs)/neutrophils, hemoglobin of 12.5 g/dL, hematocrit of 37.2%, AST of 26 U/L, and ALT of 29 U/L. Abdominal computed tomography (CT) showed free fluid approximately 1 cm thick around the liver and heterogeneous areas of abscess formation in the right lateral gallbladder, which measured approximately 5 × 5 cm in size and was partly encapsulated, containing free air. The CT also demonstrated diffuse free fluid between the bowel loops and pelvis, as well as a hydropic gallbladder with pericholecystic fluid, wall thickening, and free air trapped in the lumen (Figure 1A - 1D).
Due to these findings on examination in the emergency department, the patient was scheduled for surgery with an initial diagnosis of intra-abdominal abscess and/or gallbladder perforation. Diffuse adhesions between the bowels and seropurulent free liquid in the abdomen were detected on exploration, and a sample was taken for cultures. A partly encapsulated abscess pouch was also identified near the gallbladder, and samples were collected for cultures. On continued exploration, no perforation was detected in the gallbladder, while hyperemia was noted on all peritoneal surfaces. Fluids within the abdomen were aspirated, adhesions between the bowels were opened, and approximately 100 cc of pus was drained from the abscess. An aspiration drainage tube was inserted in the abscess pouch.
Until the culture report was received, the patient was treated with intravenous ceftriaxone at a daily dose of 2 g per day and metronidazole 500 mg twice per day. S. anginosus was reproduced in the culture sample taken from the intra-abdominal abscess. Since the results of antibiotic susceptibility testing revealed that the reproducing microorganism was sensitive to ceftriaxone, the treatment was continued in the same manner. On clinical follow-up, the patient’s leukocyte count was found to have fallen to 8,200/mm3 (with 55% PNLs). The patient was discharged without complications on the sixth postoperative day, and his antibiotic treatment was completed with 4 weeks of oral medication.
3. Discussion
Intra-abdominal infections are an inflammatory response of the peritoneum to microorganisms and their toxins, resulting in accumulation of purulent exudate in the abdominal cavity. Peritonitis is classified as primary, secondary, or tertiary. Primary peritonitis, also called spontaneous peritonitis, develops without any complications arising in the gastrointestinal system, such as a visible perforation or anastomotic leak. Thus, the infection is thought to reach the peritoneum in a hematogenous manner. Abscesses are another form of intra-abdominal infections. They develop in some patients depending on the type of microorganism that has led to the intra-abdominal infection, the quantity of inoculum, and the infection period (3).
The most common causes of intra-abdominal abscesses are gastrointestinal perforations, postoperative complications, penetrating traumas, and genitourinary infections. In one-third of cases, the abscess arises as a sequela of diffuse peritonitis (1). Furthermore, many publications have reported that organ abscesses may also be caused by oral infections, such as gingivitis and dental abscesses, with poor oral hygiene and dental problems. Various reports have shown that bacteremia development with impairment of mucosal integrity due to poor oral hygiene may lead to hepatic abscesses (4, 5). We present a patient with no regular teeth-cleaning regimen and poor oral hygiene, who had not undergone dental check-ups for a long period and had dental caries.
Ultrasonography (USG) is a useful non-invasive method that is easily applied for identifying intra-abdominal inflammatory processes (6). With USG, even peritoneal fluid of < 100 mL can be identified. If peritoneal fluid is detected on USG, diagnostic aspiration can be carried out under USG guidance. On Gram staining of the fluid, detection of white blood cells or bacteria generally indicates emergency laparotomy. Culdocentesis can be carried out in cases of pelvic peritonitis. A large number of white blood cells may be detected during abdominal aspiration, and an offensive odor may occur due to an exudative polymicrobial anaerobic infection (6). Since the patient presented to our hospital’s emergency department with an acute abdomen history, including diffuse abdominal rigidity, diffuse peritonitis was initially considered. Therefore, contrast-enhanced CT of the abdomen was performed. Although the importance of USG and Gram staining in intra-abdominal abscesses is highlighted in the literature, this method is preferred mostly for elective patients and for isolated abscess formation. Since our case was assessed under emergency conditions and an abdominal CT scan was performed with a pre-diagnosis of acute surgical abdomen (diffuse peritonitis), there was no need for USG.
Computed tomography is an invaluable diagnostic procedure for patients with suspected intra-abdominal infections (7), and it should include images of the entire abdomen and pelvis. The diagnostic value of CTs performed using intravenous, oral, and rectal contrast materials is higher than without contrast. Intracavitary air, inhomogeneity of contents, and screening of one abscess capsule leads to a diagnosis of intra-abdominal abscess. If edema develops in the mesenteric adipose tissue, this indicates inflammation (7). On the contrast-enhanced abdominal CT of our patient, increased hypodensity around the right lobe of the liver was observed, which led to the diagnosis of abscess formation (Figure 1).
The treatment approach for intra-abdominal infections encompasses surgical exploration, termination of the infectious period, and supportive care to enhance the patient’s response to sepsis treatment. The underlying pathology should be removed surgically, and drainage of the infection is necessary (7). In our case, the abdominal fluids were aspirated and the abscess was drained. Meanwhile, intravenous ceftriaxone and metronidazole were administered (Table 1).
| Reference | Patient Age (y)/Sex | Underlying Conditions | Blood Culture | Organ Dissemination | Antimicrobial Therapy After Diagnosis | Outcome and Follow-Up | |||
|---|---|---|---|---|---|---|---|---|---|
| Brain | Liver | Spleen | Other | ||||||
| Mofredj 1999 (8) | 60/Male | COPD, tooth cavities | + | + | + | IV amoxicillin followed by 1 month oral amoxicillin | Healed, right-hand paresis (5 months) | ||
| Lee et al. 2005 (9) | 58/Male | Total left hip arthroplasty | + | + | Peri-prosthetic abscess | IV ceftriaxone + arthroplasty removal + extraventricular drainage + hepatic | Deceased | ||
| Lombardi et al. 2008 (10) | 35/Male | Chronic alcholism, moderate BPCO, duodenal ulcer | - | + | Peritonitis | Splenectomy, appendectomy, peritoneal drainage | Healed | ||
| Kitagawa et al. 2010 (11) | 66/Female | Neurofibromatosis type 1, gastro- intestinal stromal tumor (GIST) | + | Tumor abscess | Sulbactam/cefoperazone, partial resection | Healed | |||
| McKenzie et al. 2010 (12) | 15/Male | Allergy | + | + | IV meropenem, vancomycin, appendectomy, debridement of abscess | Healed | |||
| Mutneja et al. 2014 (13) | 57/Male | Osteoarthritis, urethral stricture, sinusitis | - | + | Lung abscess | IV ceftriaxone, vancomycin, metronidazole | Healed | ||
| Walkty et al. 2014 (14) | 47/Male | Alcoholism | + | Abscess in leg muscles | IV ceftriaxone, metronidazole | Healed | |||
| Present study | 32/Male | Tooth decay | Abscess near liver | IV ceftriaxone, metronidazole | Healed | ||||
S. anginosus bacteria are commensal in the oropharyngeal isthmus, urogenital canal, and gastrointestinal tract (2). In cases of poor oral hygiene or alcoholism, its concentration in the saliva increases (15). In most publications, the clinical significance of bacteremia related to S. anginosus is noted (16), and it has also been reported that it can lead to serious pyogenic infections that cause abscess formation later on (16, 17). An infection may occur in the central nervous system, head and neck, abdominal cavity, or chest cavity (16, 17). While peritonitis and abscess formation due to S. anginosus is uncommon, such cases have not been defined in the literature. The poor oral hygiene of our reported patient suggests a hematogenous pathogenesis caused by a gastrointestinal focus.
In conclusion, except in immunodeficient patients or in pathologies of the bile duct and gastrointestinal system, the incidence of intra-abdominal abscesses caused by S. anginosus is relatively low. It should be kept in mind that this oral flora bacterium may cause transient bacteremia and deep-seated organ abscesses in immunodeficient patients with poor oral hygiene. Such patients with intra-abdominal abscesses should be treated with antibiotics and surgery.