1. Background
Toxoplasma gondii is one of the most important infectious diseases, having a worldwide distribution. Acquired toxoplasmosis is usually benign and asymptomatic, but it can be dangerous and have serious consequences in immunocompromised people and pregnant women. The disease is transmitted through consumption of contaminated water and food, as well as across the placenta in women whose first acute exposure to T. gondii occurs during pregnancy (1, 2). The prevalence of toxoplasmosis in humans varies depending on age, geographic region, temperature, humidity, eating habits and the presence of cats in the home. About 30% to 60% of the world’s human population is infected with T. gondii (3, 4).
Rapid and appropriate diagnosis of toxoplasmosis is of great importance, as timely diagnosis and appropriate treatment can significantly reduce complications of this disease (4). Inoculating a susceptible animal with a sample from the patient, performing a cell culture and observing the organism in tissue sections or a smear prepared from body fluids is a process with suitable sensitivity and specificity to diagnose toxoplasmosis; however, this technique is not usually used in medical diagnostic laboratories, due to the need for special facilities, the relatively long time needed to determine the test result and the risk of human and environmental contamination. Detecting antibodies against T. gondii in an individual’s serum is the common method to diagnose toxoplasmosis (5).
IgM antibodies are usually produced within the first week of the disease and usually decrease within a few months; however, in some cases, they persist for years. IgG-type antibodies are produced after one or two weeks, reach their maximum level within six months and then fall to a minimum within two years but remain present throughout the patient’s life (4). Among the available methods to detect anti-T. gondii antibodies in serum, ELISA is the most suitable due to the simplicity of implementation, relatively high sensitivity, accessibility of materials and means in the form of commercially available kits and lack of need for expensive devices. Although methods such as immunoblotting and radioimmunoassay are also of suitable diagnostic value, they are not used in most medical diagnostic laboratories due to the complexity of implementation (4, 6).
The ELISA method does have some problems, including unacceptable false-positive and -negative results from kits; differing stability of immunoglobulins detectable by antigens used in these methods; and the incidence of false-positive results due to the presence of rheumatoid factors and natural antibodies, which complicate the interpretation of test results and the final test outcome (4, 7). Most of these problems are created by antigens used in the tests designed for this purpose. Past research has shown that the use of desirable antigens can lead to increased test sensitivity and decreased costs compared with commercial kits. In addition, diagnosing and distinguishing between the chronic and acute forms of this disease requires several serum tests performed at time intervals. This is important for the diagnosis of infection in pregnant women, as the parasite may be transmitted to the fetus during the period of diagnosis. Several studies have been conducted to identify compounds of T. gondii for use as antigens in serological tests designed to diagnose toxoplasmosis to resolve the above-mentioned problems (6, 7).
2. Objectives
In this study, an indigenous diagnostic ELISA kit was prepared and its sensitivities and specificities were compared with commercial kits using the above-mentioned strain antigens. The commercially available kits are all produced in other countries using non-Iranian RH antigens, which may affect the results. In this study, due to the high sensitivity and specificity of ELISA (98% - 99%) for the diagnosis of toxoplasmosis, this method is considered as the reference for the prepared indigenous kit.
3. Methods
3.1. Antigen Preparation
The local RH strain of T. gondii was prepared for ELISA testing according to the method described by Dahl and Johnson (8), with some modifications. Fifty male mice BALB/C with average weight of 25 - 30 gm, 5 - 6 weeks of age, were inoculated intraperitoneally with 0.02 mL of T. gondii RH strain parasite and 109 tachyzoites. After 4 days, 1 mL of sterile saline was injected intraperitoneally and then aspirated and examined under a light microscope. Next, 0.02 mL of the fluid was placed into the peritoneal cavity of other mice for maintenance. The fluid was centrifuged and washed with PBS containing Tris-buffered ammonium chloride and incubated in a water bath to destroy red blood cells. The suspension was centrifuged and washed and forced through a syringe (needle size 27) to release the tachyzoites from the peritoneal cells. These were filtered through polycarbonate membrane (pore size 3 mm), centrifuged and washed. After washing, the tachyzoites were counted and their viability was determined using trypan blue stain. The antigens were sonicated in an ice bath 5 times for 30 s and centrifuged at 12000 rpm for 45 min at 4°C. Protein concentration was determined using the method described by Lowry et al. (9).
3.2. Serum Samples
In this study, 200 serum samples from patients with T. gondii whose IgM and IgG antibodies had been detected using commercial kits were selected to assess the sensitivity of the prepared indigenous test. The specificity of the method was evaluated using 40 heterologous serum samples (10 serum samples each from groups of patients with tuberculosis, leukemia and hydatid cysts). The patients were confirmed to be healthy (having no anti-T. gondii IgG and IgM antibodies in their serum) using commercial ELISA kits. In addition, 200 negative-control serum samples were obtained from clinically healthy individuals.
3.3. Design of Indigenous ELISA Using Local Antigens from the RH Strain of T. gondii
The optimum dilutions were determined by checkerboard titration of antigen, serum and conjugate as described by Lind et al. (10), with some modifications. Microplates (Greiner, Germany) were coated with 100 µL of sonicated tachyzoites of T. gondii RH strain with 0.3 mg/mL concentration, diluted 1:50 in carbonate buffer (pH = 9.6), and then incubated 180 min at 37°C.
The plates were washed three times with 300 µL PBS containing 0.1% Tween 20 and blocked with 5% nonfat dry milk for 60 min at 37°C. After washing, 100 µL of serum sample, diluted 1:10 in PBS, was added and the microplate was incubated for 90 min at 37°C. After removing as above, 100 µL of alkaline phosphatase-labeled anti-goat conjugate (Sigma-Aldrich), diluted 1:3000 in PBS for IgG and 1:1000 for IgM, was added to the wells, and then the microplates were incubated at 37°C for 60 minutes. After removing, 100 µL of substrate solution (10 mg/mL 4-nitrophenylphosphate in 10 ml diethanolamine buffer, pH = 9.6) was added and the microplate was left for 30 min at room temperature. The reaction was stopped with 100 µL of 20% sulfuric acid, and the optical density at 450 nm was read in an ELISA reader (ELX800-Biotec). The cutoff value of optical densities (OD) was determined by the method of Hillyer et al. (11): the mean OD of negative control sera plus two standard deviations.
4. Results
The results obtained with commercial ELISA kits and ELISA using local antigens for T. gondii antibody detection were as follows. Serum samples from 100 healthy individuals were tested using indigenous ELISA with anti-T. gondii IgG, and the cutoff value with 95% confidence was detected to be 0.368. Similarly, serum samples from 100 healthy individuals were examined using ELISA with anti-T. gondii IgM, with a cutoff value of 0.369. Patient serum samples containing anti-T. gondii IgG tested positive with indigenous ELISA in 98 of 100 cases (98%); thus, the sensitivity of the test was estimated to be 98%. The sensitivity of commercial ELISA was 100% (Table 1).
| Number | OD | Number | OD | Number | OD | Number | OD |
|---|---|---|---|---|---|---|---|
| 1 | 0.520 | 26 | 0.513 | 51 | 0.471 | 76 | 0.602 |
| 2 | 0.508 | 27 | 0.472 | 52 | 0.401 | 77 | 0.531 |
| 3 | 0.473 | 28 | 0.453 | 53 | 0.465 | 78 | 0.431 |
| 4 | 0.460 | 29 | 0.506 | 54 | 0.485 | 79 | 0.530 |
| 5 | 0.486 | 30 | 0.463 | 55 | 0.604 | 80 | 0.419 |
| 6 | 0.470 | 31 | 0.508 | 56 | 0.435 | 81 | 0.519 |
| 7 | 0.482 | 32 | 0.401 | 57 | 0.590 | 82 | 0.450 |
| 8 | 0.465 | 33 | 0.505 | 58 | 0.513 | 83 | 0.422 |
| 9 | 0.430 | 34 | 0.569 | 59 | 0.413 | 84 | 0.432 |
| 10 | 0.526 | 35 | 0.426 | 60 | 0.572 | 85 | 0.400 |
| 11 | 0.440 | 36 | 0.400 | 61 | 0.412 | 86 | 0.520 |
| 12 | 0.459 | 37 | 0.503 | 62 | 0.467 | 87 | 0.487 |
| 13 | 0.399 | 38 | 0.501 | 63 | 0.433 | 88 | 0.300 |
| 14 | 0.453 | 39 | 0.409 | 64 | 0.439 | 89 | 0.417 |
| 15 | 0.411 | 40 | 0.445 | 65 | 0.416 | 90 | 0.500 |
| 16 | 0.455 | 41 | 0.300 | 66 | 0.492 | 91 | 0.438 |
| 17 | 0.512 | 42 | 0.480 | 67 | 0.515 | 92 | 0.448 |
| 18 | 0.502 | 43 | 0.440 | 68 | 0.504 | 93 | 0.601 |
| 19 | 0.432 | 44 | 0.403 | 69 | 0.436 | 94 | 0.419 |
| 20 | 0.405 | 45 | 0.451 | 70 | 0.503 | 95 | 0.481 |
| 21 | 0.483 | 46 | 0.600 | 71 | 0.521 | 96 | 0.484 |
| 22 | 0.600 | 47 | 0.511 | 72 | 0.450 | 97 | 0.442 |
| 23 | 0.451 | 48 | 0.417 | 73 | 0.592 | 98 | 0.485 |
| 24 | 0.421 | 49 | 0.406 | 74 | 0.441 | 99 | 0.407 |
| 25 | 0.601 | 50 | 0.450 | 75 | 0.508 | 100 | 0.503 |
The 100 patient serum samples containing anti-T. gondii IgM tested positive with indigenous ELISA in 99 cases (99%), establishing the sensitivity of the test as 99%, whereas the sensitivity of commercial ELISA was 100% (Table 2). There was no statistically significant difference between the tests (P value ≥ 0.05). To determine specificity, 40 serum samples were taken from patients with leukemia, hydatid cyst or tuberculosis. These samples, when examined with indigenous ELISA using anti-T. gondii IgG, gave a negative result in all 40 cases (100%). Thus, the specificity of the test was determined to be 100%, equivalent to commercial ELISA.
| Number | OD | Number | OD | Number | OD | Number | OD |
|---|---|---|---|---|---|---|---|
| 1 | 0.637 | 26 | 0.651 | 51 | 0.423 | 76 | 0.432 |
| 2 | 0.853 | 27 | 0.546 | 52 | 0.525 | 77 | 0.660 |
| 3 | 0.451 | 28 | 0.620 | 53 | 0.425 | 78 | 0.485 |
| 4 | 0.448 | 29 | 0.434 | 54 | 0.435 | 79 | 0.522 |
| 5 | 0.538 | 30 | 0.412 | 55 | 0.511 | 80 | 0.410 |
| 6 | 0.528 | 31 | 0.514 | 56 | 0.426 | 81 | 0.506 |
| 7 | 0.729 | 32 | 0.499 | 57 | 0.601 | 82 | 0.462 |
| 8 | 0.551 | 33 | 0.453 | 58 | 0.501 | 83 | 0.460 |
| 9 | 0.645 | 34 | 0.508 | 59 | 0.408 | 84 | 0.520 |
| 10 | 0.456 | 35 | 0.601 | 60 | 0.520 | 85 | 0.415 |
| 11 | 0.438 | 36 | 0.446 | 61 | 0.451 | 86 | 0.541 |
| 12 | 0.616 | 37 | 0.450 | 62 | 0.440 | 87 | 0.416 |
| 13 | 0.482 | 38 | 0.503 | 63 | 0.635 | 88 | 0.650 |
| 14 | 0.433 | 39 | 0.430 | 64 | 0.850 | 89 | 0.536 |
| 15 | 0.661 | 40 | 0.615 | 65 | 0.431 | 90 | 0.619 |
| 16 | 0.486 | 41 | 0.532 | 66 | 0.422 | 91 | 0.433 |
| 17 | 0.483 | 42 | 0.647 | 67 | 0.518 | 92 | 0.411 |
| 18 | 0.523 | 43 | 0.410 | 68 | 0.721 | 93 | 0.513 |
| 19 | 0.412 | 44 | 0.540 | 69 | 0.551 | 94 | 0.452 |
| 20 | 0.507 | 45 | 0.413 | 70 | 0.643 | 95 | 0.507 |
| 21 | 0.464 | 46 | 0.498 | 71 | 0.409 | 96 | 0.300 |
| 22 | 0.462 | 47 | 0.402 | 72 | 0.455 | 97 | 0.600 |
| 23 | 0.416 | 48 | 0.522 | 73 | 0.437 | 98 | 0.445 |
| 24 | 0.542 | 49 | 0.511 | 74 | 0.615 | 99 | 0.449 |
| 25 | 0.417 | 50 | 0.711 | 75 | 0.481 | 100 | 0.500 |
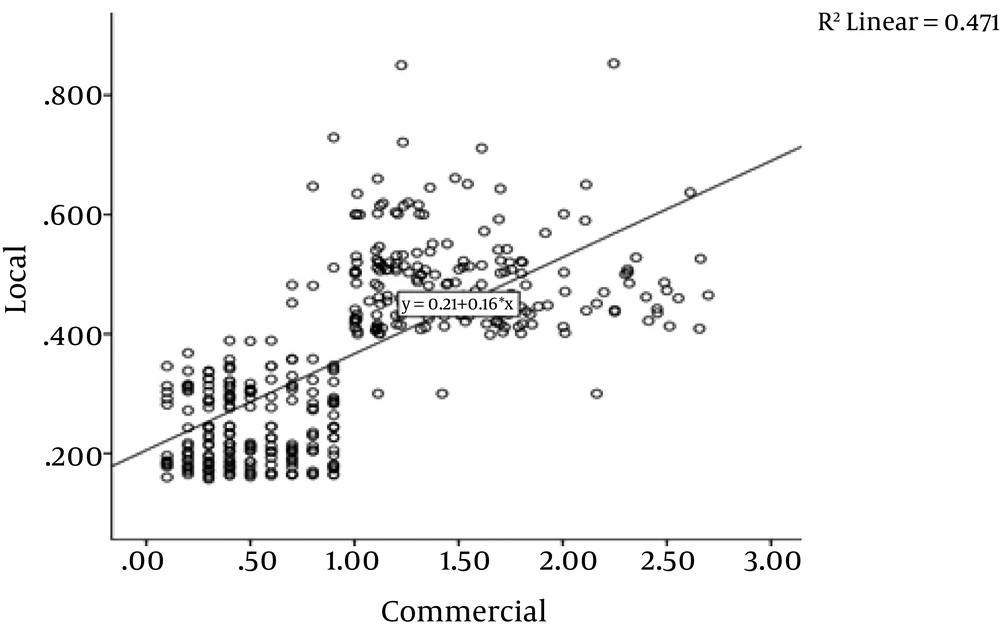
However, when the same samples were examined with indigenous ELISA using anti-T. gondii IgM, the results were 28.6% among leukemia patients, 21.4% for hydatid cyst patients and 16.7% for tuberculosis patients. Semiquantitative analysis using Pearson’s correlation coefficient gave similar results: 0.69 R value and P ≤ 0.001 for the correlation between commercial and indigenous ELISA (Figure 1).
5. Discussion
It is estimated that one third of the people in the world have been exposed to the parasite T. gondii (3). In Iran, toxoplasmosis continues to be a public health problem, and the seroprevalence of this infection is highly varied in different regions (2, 12-14). Khuzestan, southwest of Iran, is endemic for T. gondii. Previously, we have detected T. gondii from a variety of human and animal sources (1, 2, 15-17). Therefore, epidemiological study of the parasite is essential in this region.
One of the most commonly used screening methods for T. gondii infection is ELISA. ELISA is fast and easy to interpret, making it appropriate for routine screening of humans and having the potential for automatization (4, 6). One of the customary questions in this regard deals with the specificity and sensitivity of commercial ELISA kits. T. gondii is known to have different lineages, I, II and III, as well as genetic diversity in different parts of the world (17-21); could these characteristics affect the serological results? Accuracy of antigen preparation and standardization are important factors for researchers. Standardization of assays for T. gondii-specific antigens is also important for monitoring infection, as large differences in assay calibration could lead to misinterpretations of the clinical course when different assays are used. Furthermore, purchasing commercial kits can be a major problem for geographically remote or developing countries, where infectious diseases are typically the main public health problem. Therefore, preparation of indigenous diagnostic kits is very significant.
In the present study, we compared the sensitivity and specificity of standard ELISA assays using locally isolated antigens and using a commercial kit. The commercial ELISA kit gave more sensitive and more specific results (both 100%) than the indigenous ELISA using anti-T. gondii IgG (98% and 99%). The specificity of indigenous ELISA using anti-T. gondii IgM was far less and probably proved a cross-reaction with other disease antigens. However, no statistically significant differences were found between the tests.
Our results can be compared with those in a 1995 study by Zhang et al. (88.9% sensitivity and 95.7% specificity) (22), a 1990 study by Malik et al. (62.5% sensitivity) (23), a 2007 study by Shaapan et al. (49% sensitivity with local antigens from the RH strain of T. gondii) (24), a 2011 study by Hassanain et al. (61.4% sensitivity) (25) and a 2013 study by Al-Olayan (50% sensitivity) (26). The higher level of sensitivity in our study might be linked to our antigen preparation methods and to our region. Most specificity in our study showed non- cross reaction. McCabe and Remington found in 1988 that the peritoneal fluid of mice infected with the RH strain of T. gondii was able to characterize anti-T. gondii IgG in human serum (27). Yamamoto et al. reported in 1998 that the antigenic compounds in the peritoneal fluid of mice infected with tachyzoites of the RH strain of T. gondii accurately characterized anti-T. gondii IgG, IgM and IgA in human serum samples and could be utilized as an antigen in serological tests (28). Ghazy et al. recommended utilization of 65 KDa antigen of T. gondii in commercial kits for diagnosis of toxoplasmosis in human serum (29).
Our conclusion is that local antigens are more suitable than commercial antigens for this purpose, as they allow for easier preparation, less expense and greater sensitivity. We recommend utilization of soluble antigens obtained from locally isolated tachyzoites to diagnose toxoplasmosis in humans using ELISA, which showed statistically equivalent diagnostic potency and sensitivity in our study compared with a commercial ELISA kit.