1. Background
Staphylococci are well known as the normal flora of the skin and mucous membranes of animals and human (1-3). However, staphylococcal infections are often caused by strains that have colonized in parts of the human body and make the colonized persons a reservoir for the spread of the organisms (4, 5). Due to the biofilm producing ability of staphylococci, they are mostly associated with chronic and implanted medical devices infections (6, 7). Staphylococcus epidermidis was the first species identified as biofilm producer; however, the same capacity was subsequently implicated in S. aureus and other coagulase negative Staphylococci (CoNS) (8, 9).
Biofilm structure contains bacteria in which cells adhere to each other on a surface and are surrounded in exopolysaccharide matrix (10). The bacteria enclosed in a biofilm make them intrinsically resistant to many antimicrobial drugs and host defenses (9, 11). The slime production in CoNS isolates occurs in three steps: attachment of bacteria to a biomaterial or artificial surface, formation of an extracellular slime such as polysaccharide intercellular adhesin (PIA) which mediates cell to cell adhesion and disassembly of the biofilm, followed by community expansion (12, 13).
It has been shown that both S. aureus and S. epidermidis contain the intercellular adhesion (ica) operon responsible for biofilm formation (14). This operon contains the icaA, icaD, icaB and icaC genes which are regulated through the product of icaR gene (15). The ica operon (icaADBC gene cluster) encodes the PIA; thus, there is a correlation between the presence of this operon and slime production in staphylococci, especially CoNS (13, 16).
2. Objectives
Identifying and controlling biofilm-forming staphylococci can be one of the essential steps for prevention and management of nosocomial infections. This study aimed to determine the biofilm producing ability and the presence of icaA/D genes among staphylococcal clinical isolates and their probable association with their antibiotic resistance profile.
3. Methods
3.1. Clinical Samples
This cross-sectional study was conducted between February and August 2013 at two Teaching hospitals (Nemazee and Faghihi) of Shiraz, a major city in the Southwest of Iran. Totally, 151 staphylococcal isolates (79 S. aureus isolates and 72 S. epidermidis isolates) were obtained from different clinical specimens and various wards of the studied hospitals. The clinical samples were blood, pus, wound, urine, endotracheal tube (ETT), sputum, cerebrospinal fluid (CSF), skin, etc.
3.2. Identification of Isolates
The isolates were recognized as S. aureus and S. epidermidis using the conventional microbiological methods, including colony morphology, Gram stain, catalase activity, growth on mannitol salt agar, DNase and tube coagulase tests, and susceptibility to novobiocin and polymyxin B. The preliminary differentiation of methicillin-resistant S. aureus ( MRSA) and methicillin-sensitive S. aureus (MSSA) isolates was based on resistance to cefoxitin (30 μg) (MAST, UK) using the disc diffusion assay according to Clinical and laboratory standards institute (CLSI) recommendations (17). The confirmed isolates were stored at -70°C for further analysis.
3.3. Biofilm Production Assay
Biofilm producing isolates were detected using the Congo red agar (CRA) method. Congo red stain (PML, Canada) was prepared as a strong aqueous solution by dissolving 37 g of the stain in 50 mL of distilled water which was sterilized (at 121°C for 15 minutes) separately from 15 g brain heart infusion agar (BHI) (Merck, Germany) in 450 mL distilled water. Congo red solution was added to the agar at the temperature of 50 - 55°C. Finally, 37 g sucrose was filtered using 0.45 μm Millipore filter (Sigma, UK) and added to the culture medium. After plating of staphylococci and overnight incubation at 37°C, biofilm producing isolates appeared as black crusty colonies, while non-biofilm producing isolates developed pink or red colonies.
3.4. Antimicrobial Susceptibility Testing
Antibiotic susceptibility against ampicillin, clindamycin, gentamicin, ciprofloxacin, trimethoprim-sulfamethoxazole, erythromycin, tetracycline, rifampin, linezolid, and vancomycin was tested on Muller-Hinton agar (Oxoid, UK) using the disk diffusion method according to CLSI recommendations (17). All the discs were obtained from Rosco Co., Denmark. S. aureus ATCC 25923 (a methicillin-sensitive strain) was used as control strain in antibacterial susceptibility tests. The diameters of the inhibition zones were interpreted according to the guidelines of CLSI (17).
3.5. DNA Extraction and PCR Assay
Genomic DNA was extracted from individual isolates using the small-scale phenol-chloroform extraction method and subjected to polymerase chain reaction (PCR) (18). For molecular confirmation of MRSA isolates, the presence of mecA gene was sought by a set of previously described primers (19). All staphylococcal isolates were analyzed for the presence of icaA and icaD genes by the primers described by Arciola et al. (20). MRSA reference strain subspecies COL, which was applied as mecA, icaA, and icaD positive genes, was kindly provided by the professor Alborzi clinical microbiology research center, Shiraz, Iran.
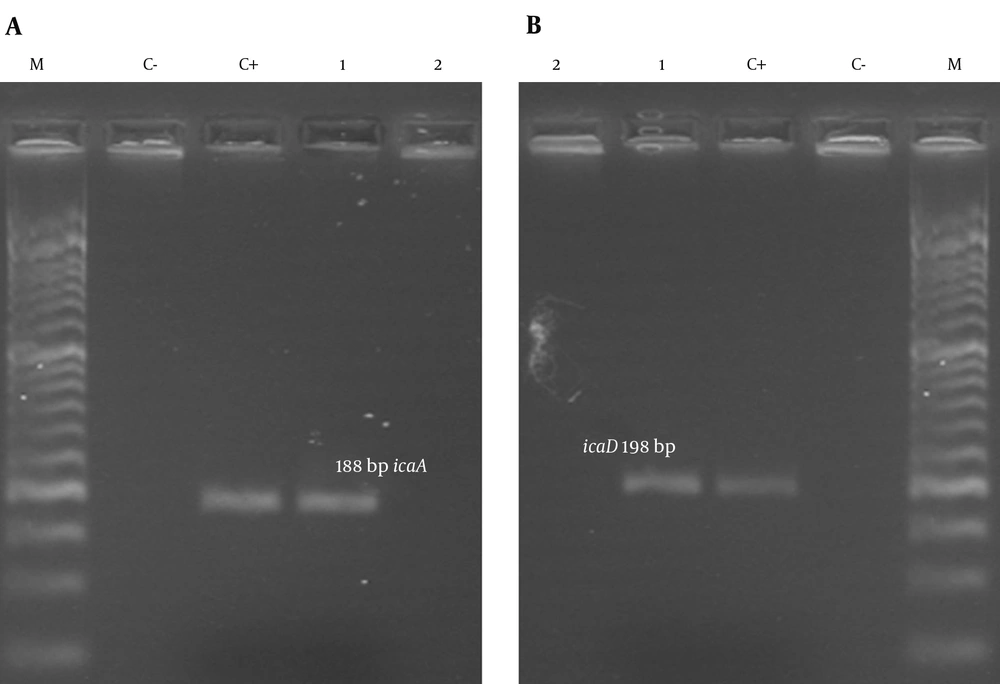
PCR was performed in a final volume of 25 μL, containing 3 μL DNA template, 2.5 μL PCR buffer (1X), 1 μL deoxyribonucleotide triphosphates solution (dNTPs, 200 μM), 1.5 μL MgCl2 (1.5 mM), 0.25 μL Taq DNA polymerase (1 Unit) and 1 μL each specific primer (1 μM) (Table 1). PCR tests were carried out in a thermocycler 5530 (Ependrof master, Germany) as follows: 5 minutes initial denaturation at 94°C, 30 cycles of denaturation at 94°C for 45 seconds, annealing (for icaA at 50°C for 45 seconds and for icaD at 56°C for 45 seconds), extension at 72°C for 1 minute, and final extension at 72°C for 10 minutes. All the reagents were obtained from Ampliqon Co., Denmark. In each run of PCR products, one negative (DNase-free water) and one positive control were included in agarose gels. Then, PCR products were loaded into 1.5% agarose gel and stained with 1% ethidium bromide (Merck, Germany) and visualized under UV trans-illuminator.
| Primer | Oligonucleotide Sequence (5′ - 3′) | Product Size, bp | Reference |
|---|---|---|---|
| mecA-F | GTGAAGATATACCAAGTGATT | 147 | 19 |
| mecA-R | ATG CGCTATAGATTGAAAGGAT | ||
| icaA-F | TCTCTTGCAGGAGCAATCAA | 188 | 20 |
| icaA-R | TCAGGCACTAACATCCAGCA | ||
| icaD-F | ATGGTCAAGCCCAGACAGAG | 198 | 20 |
| icaD-R | CGTGTTTTCAACATTTAATGCAA |
The List of Used Primers in the Present Study
3.6. Statistical Analysis
Analysis was performed by using SPSSTM software, version 16.0 (Chicago, IL, USA). The results are presented using descriptive statistics in terms of relative frequency. Values were expressed as the percentages of the group (for categorical variables). Chi-square test was used to determine any statistical association. Statistical significance was regarded as P values < 0.05.
4. Results
4.1. Detection of Slime Production in Staphylococci by the CRA Assay
Of 79 S. aureus isolates, 34 (43%) were identified as MRSA and 45 (57%) as MSSA. The distribution of biofilm producer staphylococci according to the source of isolates is presented in Table 2. Among S. aureus isolates examined with CRA assay, 43 (54.4%) showed the ability to produce biofilm; of the MRSA and MSSA isolates, 22 (64.7%) and 21 (46.7%) isolates produced black colonies, respectively, and this difference was not statistically significant (P = 0.17). On the other hand, out of 72 clinical isolates of S. epidermidis, 51 (71%) were biofilm producers. The relative frequency of biofilm producing S. epidermidis isolates (70.8%) was significantly higher than that of S. aureus isolates (54.4%) (P < 0.038). The most common source of biofilm producing isolates in both S. aureus and S. epidermidis isolates was ETT with the rate of 100% biofilm formation. The results of antibiotic resistance pattern of biofilm producing staphylococci are shown in Table 3. Overall, none of S. aureus and S. epidermidis isolates were resistant to linezolid and vancomycin. Interestingly, most of biofilm producing isolates exhibited higher rates of antibiotic resistance compared to non-biofilm producing isolates.
| Specimen | S. aureus | S. epidermidis | ||
|---|---|---|---|---|
| CRA + Positive/Total | icaA/D + Positive/Total | CRA + Positive/Total | icaA/D + Positive/Total | |
| ETT | 5/5 | 5/5 | 8/8 | 8/8 |
| Wound | 10/16 | 13/16 | 9/12 | 11/12 |
| Urine | 8/14 | 8/14 | 5/7 | 6/7 |
| Sputum | 5/11 | 7/11 | 5/8 | 5/8 |
| Blood | 8/10 | 10/10 | 13/15 | 15/15 |
| CSF | 3/7 | 3/7 | 4/7 | 5/7 |
| Skin | 1/4 | 1/4 | 3/7 | 3/7 |
| Other | 3/12 | 3/12 | 4/8 | 6/8 |
| Total, No. (%) | 43 (54.4)a | 50 (63.3)b | 51 (70.8)a | 59 (81.9)b |
Results of Biofilm Production in Staphylococci Isolates Based on the Source of Isolation
| Antibiotic | S. aureus | S. epidermidis | ||
|---|---|---|---|---|
| Total (N = 79) | CRA + (N = 43) | Total (N = 72) | CRA + (N = 51) | |
| Ampicillin | 76 (96.2)b | 43 (100) | 63 (87.5) | 48 (94.1)c |
| Tetracycline | 45 (57) | 29 (67.4)c | 41 (56.9) | 25 (40)c |
| Ciprofloxacin | 32 (40.5) | 24 (55.8)c | 37 (51.4) | 28 (54.9) |
| Erythromycin | 45 (57) | 27 (62.8) | 50 (69.4) | 35 (68.6) |
| Clindamycin | 40 (50.6)b | 23 (53.5) | 48 (66.7) | 34 (66.7) |
| Gentamycin | 29 (36.7) | 19 (44.2) | 26 (36.1) | 20 (39.2) |
| Rifampin | 20 (25.3) | 11 (25.6) | 9 (12.5) | 5 (9.8) |
| Co-trimoxazole | 8 (10.1) | 6 (13.9) | 49 (68.1) | 37 (72.5) |
| Linezolid | 0 | 0 | 0 | 0 |
Results of Antibiotic Resistance Pattern of Staphylococci Isolates Based on the Ability of Biofilm Productiona
4.2. Detection of Slime Production in Staphylococci by PCR
The results of PCR on icaA and icaD genes revealed that the presence of each gene in staphylococcal isolates was related to the presence of the other one. Slime production was confirmed by the presence of icaA/D genes in 50 (63.3%) S. aureus isolates. Among S. epidermidis isolates, 59 (81.9%) carried the icaA/D genes. The icaA/D genes were more prevalent among S. epidermidis isolates than S. aureus ones and the difference was statistically significant (P < 0.011). The presence of the icaA (188 bp) and icaD (198 bp) genes in all the investigated staphylococci was shown by the amplification of the corresponding fragments (Figure 1).
5. Discussion
The biofilm formation on mucosal and inanimate surfaces such as invasive medical devices has been considered as a major virulence determinant in staphylococci (13). In view of large number of infections caused by biofilm- producing bacteria, it seems that early detection and elimination of these bacteria are necessary.
To evaluate slime production among staphylococci, usually a phenotypic method along with ica operon detection is used. The CRA method due to its easiness and good sensitivity has been widely used for phenotypic detection of biofilm production in different bacteria (21). In the present study, 54.4% and 70.8% of S. aureus and S. epidermidis isolates were recognized as biofilm producer by CRA method, respectively. As indicated by Osman et al. CRA is a reliable and suitable method for routine evaluation of slime production (7). Several studies previously applied CRA phonotypical method to assay biofilm formation among staphylococci isolates in Iran and obtained various results based on the source of isolation, type of species, and geographic region. In the survey of Eftekhar et al. in Tehran, 53.3% of MRSA isolates were assessed to be potential biofilm producers (22). Solati et al. in a multicenter hospital study reported a rate of 50% biofilm formation by S. epidermidis isolates (11). Ohadian Moghadam et al. showed high rates of biofilm production (more than 80%) among S. aureus isolates obtained from bourn wound samples in Tehran, North of Iran (23). In another study from Kashan, all MRSA isolates from nasal carries were able to form biofilms (24). These variations in frequency of biofilm producing staphylococci are documented in other parts of the world, as well. The rates of biofilm production in staphylococci isolates have been reported in the range of approximately 30% to more than 70% in different Asian, African, and European countries (20, 25, 26).
In the present study, three major sources of biofilm producing isolates were ETT, wound, and blood samples. In accordance with our findings, medical instruments were suggested as a common source of biofilm producing staphylococci (27, 28). However, such high rates of biofilm producing isolates from wound and blood samples in our study are not uncommon, since several authors have shown high rates of biofilm formation among staphylococci obtained from these settings (29-31).
Our results demonstrate that biofilm forming isolates exhibited remarkable rates of antibiotic resistance compared to non-biofilm producing isolates. Antibiotic resistance is a growing health concern, especially in developing countries (32). Among biofilm producing S. aureus isolates, the resistance rate against tetracycline and ciprofloxacin was significantly higher compared to non-biofilm producing isolates. On the other hand, S. epidermidis biofilm producers revealed higher resistance to ampicillin and tetracycline compared to non-biofilm producing isolates (P < 0.05). In two Iranian studies, similar to our findings, most of the biofilm forming staphylococci isolates had higher antibiotic resistance and multiple drug resistance (MDR) rates (23, 24). The same findings have been reported by Sahal et al. in Turkey, indicating that majority of strong biofilm forming S. epidermidis strains were β-lactams resistant, and notably 100% of them were MDR (33).
The fundamental role of co-expression of the icaA and icaD genes in biofilm formation among S. aureus and S. epidermidis causing catheter-associated and nosocomial infections through the regulation and production of PIA has already been emphasized (8). In the present investigation, the icaA and icaD were evaluated because the detection of these genes implies the biofilm formation by staphylococcal isolates. In addition, these genes regulate the slime production (7, 13). In our study, the presence of icaA gene in all tested isolates was associated with the presence of icaD gene and vice versa, which has also been mentioned by other authors (28, 34). The frequency of icaA/D genes among our staphylococci isolates was relatively high; however, such remarkable rates of ica operon among staphylococci isolates are not unexpected, since the same finding has been implicated in several studies (19, 34, 35).
The results of this study and previous studies indicate a high prevalence of the icaA/D genes among staphylococci isolates, and that their presence is not necessarily associated with in-vitro formation of biofilm (36). In the current study, the proportion of S. epidermidis isolates that were positive for icaA/D genes in PCR method was higher than the proportion of those that were positive in CRA method. This discrepancy can be attributed to the presence of other molecules involved in the biofilm formation such as ClpP, BHP, and Aae among CoNS isolates (13). Moreover, different studies have demonstrated that the expression of the ica locus is considerably variable and can be affected by many factors, which, in turn, results in the increase or decrease of biofilm production (7). The elucidation of the adhesive processes among clinical isolates might be a solution for developing anti-adhesive approaches to fight with infections due to opportunistic bacteria.
There are some limitations in our study. First, we did not perform other phenotypic methods used in the confirmation of biofilm formation. Second, other genes involved in the slime production process were not evaluated in this study.
5.1. Conclusions
CRA method is a practicable procedure that is in agreement with genotypic methods, particularly among S. aureus isolates. The remarkable rate of icaA/D genes and higher rate of antibiotic resistance among biofilm producing staphylococci isolates found in the present study suggest their potential risk for establishing persistent infection and therapeutic failure in hospitalized patients. However, further studies are needed to evaluate the role of slime production in nosocomial infections.