1. Background
World Health Organization (WHO) has reported that 130 million infants are born each year, 8 million die during the first day of life, and more than 10 million die before they become 5 years old (1). It is estimated that neonatal mortality is one-third of children mortality in the world, and infections are one of the main factors causing neonatal mortality (2). Blood Stream Infections (BSI) and Urinary Tract Infections (UTI) especially in the new born babies are considered as one of the main and important factors which cause neonatal diseases and mortality in the world, especially in developing countries (3). Many babies are born prematurely for many reasons such as: ascending genital tract infection, multiple pregnancies, infections, short time between pregnancies; so, they are admitted to Neonatal Intensive Care Units (NICUs) (4). Infections like sepsis, meningitis, infant convulsion, urine infections and diarrhea are one of the main problems in hospitalized infants in NICU (5).
The rate of blood infection in developing countries is 3 to 20 times higher than the other countries, and more than half of the hospitalized infants in NICUs are affected by blood infection (2). A full period of infancy consist of the first four weeks of term infants or four weeks after a preterm infant leaves the hospital (6). Neonatal sepsis is the disease of the infants less than a month (28 days) having clinical symptoms, and their blood culture is positive. Two forms of sepsis related to the age of sepsis are: Early onset and late onset. Early septicemia happens a little after birth (before 48 hours). In principle, early septicemia is caused during the first week after birth and specifically is resulted by existing organism in the uterus (5). Late septicemia occurs 48 hours after birth in neonatal with clinical symptoms. Late septicemia is recognized after the first week of life and is acquired from the care giving environment (5).
Host sensitivity, economical-social factors, activities in neonatal and obstetrics and gynecology wards, and the mother's health and nutrition conditions are the factors that causing neonatal sepsis. Infants suffering from septicemia, especially the early septicemia, often have got one or more risk factors related to pregnancy or childbirth. Among the risk factors are early childbirth, low birth weight, premature rupture of membranes, prolonged premature rupture of membrane and infectious childbirth caused by birth trauma and hypoxia (7). One of the best specific diagnostic methods of neonatal septicemia is isolation of a pathogenic microorganism from blood (5).
Urinary tract infections are the other prevalent infections. The UTI is one of the most common pediatric infections. It may cause permanent kidney damage. Occurrences of a first-time symptomatic UTI are highest in boys and girls during the first year of life and are markedly decreased after that. Urinary tract infection in newborns is frequently associated with bacteremia and may result in long-term complications. In some cases, it leads to neurological or predisposing structural abnormalities in child. Urinary tract infection occurs in 3% to 5% of girls and 1% of boys. Incidence of UTI in neonates has a particular importance because UTI in this age group (with an incidence of about 5%) does not cause any clinical symptoms except fever and if it is not known, it will cause renal damage (scar) (8, 9).
2. Objectives
Septicemia is the most prevalent cause of mortality in developing countries. The problem of neonatal UTI due to its vast consequences in old age groups has got special importance and because the most organisms causing the same infections are Gram-negative organisms. Today, resistance of organisms, especially Gram-negatives, against antibiotic treatment has been seen abundantly; therefore, this study aimed to diagnose and study the bacterial factors causing neonatal blood and urine infections in NICUs of three hospitals and to determine their antibiotic resistance patterns.
3. Materials and Methods
This cross-sectional descriptive study was conducted in NICUs of three hospitals (Imam Hussein Hospital, Children Hospital Center and Bahrami Hospital) in Tehran City, Iran, for a period of seven months from September 2011 to April 2012. Sampling was performed on hospitalized infants suspected with blood and urine infections in NICUs of three above-mentioned hospitals before they were given any antibiotic therapy under proper aseptic conditions. The 2 to 3 mL blood sample was obtained from peripheral veins, inoculated on the BHI agar (Merck, Germany) and incubated in 37°C for 24 hours (it was continued until 72 hours for late-growing bacteria). The samples were simultaneously inoculated on MAC Conkey (Merck, Germany) agar and blood agar (Merck, Germany) for 24 and 72 hours of incubating, respectively (72 hours to grow late-growing bacteria).
Urine samples were collected using urine bags and about 5cc of it were poured in to sterile tubes and a full loop; this was cultured in Eosin Methylen Blue (EMB) (Merck, Germany) and blood agar and incubated for 24 hours in 37°C. Positive urine cultures were defined as more than 100,000 CFU/mL bacterial colonies by bag specimen collection. After the growth of the bacteria (in blood and urine samples), first Gram stain was performed, then other biochemical, distinctive and specific tests were performed based on the morphology observed in a microscope. For Gram-negative bacteria detection, a set of gallery tests including TSI (Triple Sugar Iron), CIT (Simon Citrate), SIM (Sulfide Indole Motility), Urea, MR (Methyl-Red), VP (Voges-Proskauer), ARG (Arginine dehydrolase), OD (Ornithine de carboxylase), LD (Lysine de carboxylase) (Merck, Germany) were used, and the obtained results were gained based on the tables in the book of Koneman.
For the final confirmation of the results, some samples were chosen randomly, and the API20E kit (BioMerieux, France) was used and the results obtained from the kit were compared with the ones already obtained. For Gram-positive bacteria, catalase test, coagulase test, sensitivity to novobiocin disk test, growth on mannitol salt agar and DNAse were performed. Determination of antibiotic sensitivity was done by disk diffusion (Kirby-Bauer) method. The results were studied using CLSI (Clinical and Laboratory Standards Institute) standard tables (10). The birth weights of the infants were classified into 4 groups: less than 1000 g (≤ 1000), between 1001 - 1500 g, between 1501 - 2000 g and more than 2001 g (2001 ≥). The results were compared between the two groups of infants with early or late-onset sepsis.
4. Results
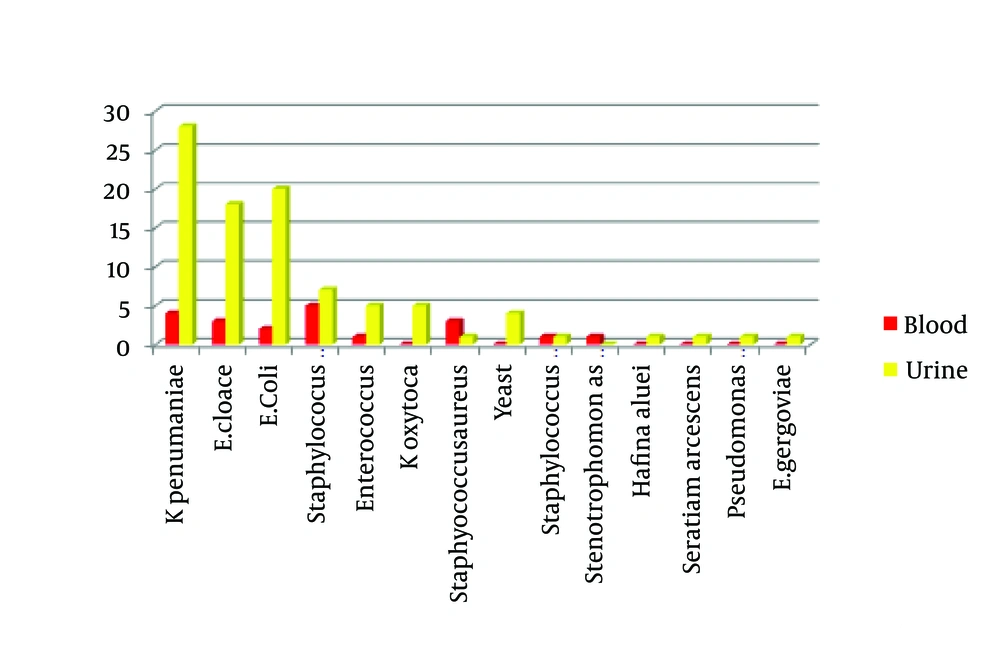
From a total of 105 blood and urine samples, 20 (19%) were blood samples and 85 (81%) were urine samples, 63.8% of the patients were boy infants, and 36.2% were girl infants. Forty- one babies (39%) were born by natural birth and 64 (61%) by cesarean birth. Among the born sick infants, most of them ranged between 1000 and 1500 g of weight (33%). Three of the infants under study died because of infection, three of whom suffered from blood infection and the rest of the infants were alive. Sixty-two percent of the infants suffered from early septicemia (age less than 72 hours), and 38% from late septicemia (more than 3 days of age). From the bacteria obtained, 81 (77.2%) were Gram-negative organisms, and 24 (22.8%) were Gram-positive organisms. Klebsiella pneumonia (30.5%), Enterobacter cloacae (21%), Escherichia coli (12.4%), Staphylococcus epidermidis (11.4%) were the most abundant organisms obtained (Figure 1).
Among the antibiotics used in order to perform antibiogram, the most antibiotic sensitivity was shown to ciprofloxacin (84.2%) among Gram-negative organisms (Table 1) and to vancomycin (83.3%), among the Gram-positive bacteria (Tables 2 and 3).
| Antibiotic Bacteria | CFX | MFX | T | NI | CIP | TS |
|---|---|---|---|---|---|---|
| K. pneumoniae | 31 | 7 | 21.9 | 48.9 | 6.2 | 28.2 |
| E. cloacae | 31.9 | 4.5 | 9 | 54.5 | 9 | 9 |
| E. coli | 53.9 | 30.8 | 46.1 | 7.7 | 30.8 | 53.9 |
| K. oxytoca | 60 | 20 | 20 | 20 | 20 | 20 |
a Abbreviations: CFX, Cefalexin; CIP, Ciprofloxacin; MFX, Moxifloxacin; NI, Nitrofurantoin; T, Tetracycline; TS, Cotrimoxazole.
| Antibiotic Bacteria | GM | OX | AK | NI | VA | A | P | TS |
|---|---|---|---|---|---|---|---|---|
| Staphylococcus epidermidis | 41.6 | 8.3 | 0 | 0 | 0 | 1.6 | 100 | 50 |
| Staphylococcus aureous | 75 | 75 | 75 | 0 | 0 | 50 | 100 | 50 |
| Staphylococcus haemolyticus | 100 | 50 | 0 | 0 | 0 | 100 | 100 | 50 |
a Abbreviations: A, Ampicillin; AK, Amikacin; GM, Gentamicin; NI, Nitrofurantoin; OX, Oxacillin; P, Penicillin; TS, Cotrimoxazole; VA, Vancomycin.
| Antibiotic Bacteria | P | VA | TS | CAZ | E |
|---|---|---|---|---|---|
| Enterococcus faecalis | 100 | 66.6 | 100 | 83.3 | 66.6 |
a Abbreviations: CAZ, Ceftazidim; E, Erythromycin; P, Penicillin; TS, Cotrimoxazole; VA, Vancomycin.
5. Discussion
Because distribution of infectious factors and infections resulted from the same infectious factors, in any country is influenced by factors like the level of health, cultural, social, economic conditions and the amount of hospital staff knowledge and awareness (from the physicians to the nurses and the lab technicians); therefore, generalization of the obtained results from the performed studies in other countries to Iran does not seem to be fair and correct. The results of the present study showed that from a total of 105 infants under study, 19% suffered from septicemia, 81% suffered from urine infection. In a study performed in Pakistan by Shams et al. it was shown that 40% of the neonates suffered from bacteria septicemia (11). In another study by Agnihotri in India, it was also reported that the rate of those suffering from septicemia was 19.19%. Therefore, the rate of those suffering from sepsis is lower in Iran compared to the other developing countries such as India and Pakistan (12).
In this study, the basis for dividing septicemia in two types of early and late was suffering from septicemia before or after 72 hours. The basis of this timing was also before or after 72 hours in studies done by Stoll et al. while the basis of this grouping in the study performed by Agnihotri was before and after one week (12, 13). Mane et al. in 2010, also issued similar results like the previous ones. In this study, just like the 4 ones mentioned above, the most abundant organisms causing both urine infection, and septicemia were K. pneumoniae (30.5%), E. cloacae (21%), E. coli (12.4%) (14). But in 2010, in a study by Qu et al. negative coagulase staphylococcus were reported as the main factors of causing neonatal blood infections (15). The rate of boy infants' suffering in this study was 63.8%, which was higher than that of girls (336.2%), especially, the rate of boy infants' suffering from urine infection was considerably higher than that of the girl infants.
In the study which Babazono performed on neonatal urine infections in NICU in Okayama in 2008, the rate of boy infants' suffering (32.7%) in comparison to that of girl infants (15.9%) was reported higher (16). In the study done by Gheibi et al. among the Gram-negative organism, the most sensitivity to ciprofloxacin (92.8%), and among the Gram-positive to vancomycin (90%) were reported which is the same as our study results (17). Another similar result is in the study which Mane et al. performed in the state of Nagpoor in India, which the most influential antibiotic for Gram-negative bacteria was ciprofloxacin with sensitivity of 66.6%, and for Gram-positive bacteria vancomycin and pristinomycin with a sensitivity of 100% (14). In the study done by Qu in 2010, all negative coagulase staphylococcus separated from neonatal infections were resistant to penicillin and were sensitive to vancomycin (15).
In this study, the highest rate of suffering was among infants with birth weight of 1000 - 1500 g (31.4%), and after that among infants with birth weight of 1501 - 2000 g (25.8%). In the study of neonatal urine infection by Bauer in 2003, the most infection rate was seen among infants with weight lower than or equal to 1500 g (8). In the year 2006, a study by the name of pediatric urinary tract infections was performed; its results showed that E. coli, K. pneumoniae, E. cloacae were the most abundant separated organisms (18). Microbic spectrum of separated organisms from infant suffering septicemia and urine infection in our country, Iran, is mostly similar to that of neighboring developing countries. Regarding the genetic, social, cultural, hygienic, nourishing differences affecting on the prevalence of bacterial factors of septicemia and urine infection in prenatal and neonatal, different studies have been performed to understand the microbic factors in different parts of the world.
Today, in spite of the considerable developments in the fields of hygienic antimicrobial treatments and protective or supportive treatments, offensive infections have always been of important factors in prenatal and neonatal mortality. Whit regard to the prevalence of sepsis and urine infections in recent years, and mortality caused by them, and also with regard to the findings in the present study, we come to this conclusion that the rate of suffering from infections, especially septicemia and urine infections, is still high in our country, Iran. Therefore, it is very important to learn more about the disease and its producing factors, especially to diagnose its favoring factors. Whit regard to a general principle which says prevention always precedes treatment; so, by knowing contributing factors of septicemia and urine infection, it will be possible for us to prevent most of them, and with determination of antibiotic sensitivity and investigation of antibiotic sensitivity of the separated organisms, it paves the way for us to provide a correct and suitable treatment and prevent resistant methods, and in this way, help suitably the type of treatment and its duration, and from the other side, be able to witness the decrease of hospital costs and expenses and ultimately that of economic.