1. Introduction
Alternaria spp. rarely causes disease in normal individuals despite its widespread distribution in nature. However, in the recent years, there is an increasing rate of infection caused by Alternaria spp. in immune-suppressed patients. The subspecies able to cause opportunistic infections in human are Alternaria alternata, A. tenuissima, A. infectoria and A. chartarum (1). The infections in human usually appear as skin or subcutaneous infections, but eye infections, invasive or noninvasive rhinosinusitis and onychomycosis could also be seen. The infection reveals itself as skin, subcutaneous infection or rhinosinusitis in immune-suppressed patients with risk factors like organ transplantation and Cushing syndrome. Onychomycosis is frequently associated with a history of nail trauma or contaminations with soil. Alternariasis responds well to classical antifungal treatment and skin, subcutaneous tissue and nail infections are well-treated with itraconazole (2, 3).
2. Case Presentation
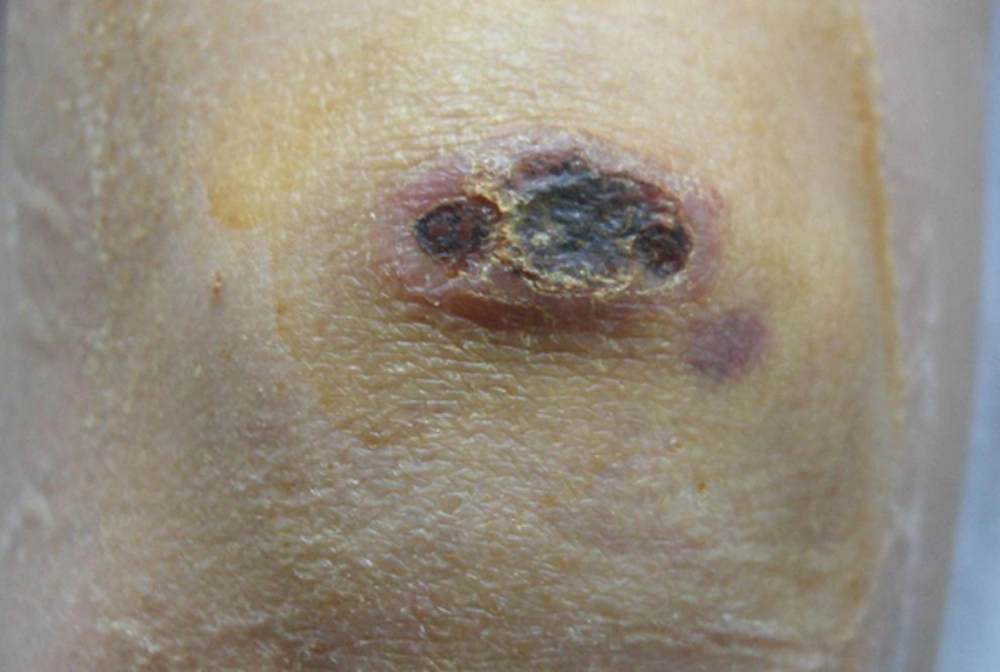
A 32-year-old female patient with chronic renal failure due to secondary hypertensive nephrosclerosis and a history of renal transplantation from a cadaver 4 months ago after 7 years of peritoneal dialysis and 4 years of haemodialysis was reported. Most patients with genetic hemochromatosis have mutations of the HFE gene and excess amount of ferrum in blood. She had been receiving desferrioxamine treatment for the last year. The patient had been treated with antithymocyte globulin, tacrolimus, mycophenolate mofetil and corticosteroid for immune suppression and trimetoprim sulfamethoxazole and acyclovir for prophylaxis. The patient was currently receiving tacrolimus, mycophenolate mofetil and corticosteroid treatment. In the post transplantation period, a urinary infection was detected in patient and treated successfully with piperacillin and imipenem. After transplantation, the patient was discharged with a serum creatinine level of 0.7 mg/dL. The patient arrived to our clinic with a complaint of ulcerative nodular lesion which is 2 × 2 cm in size located at fronto-superior right-knee area (Figure 1).
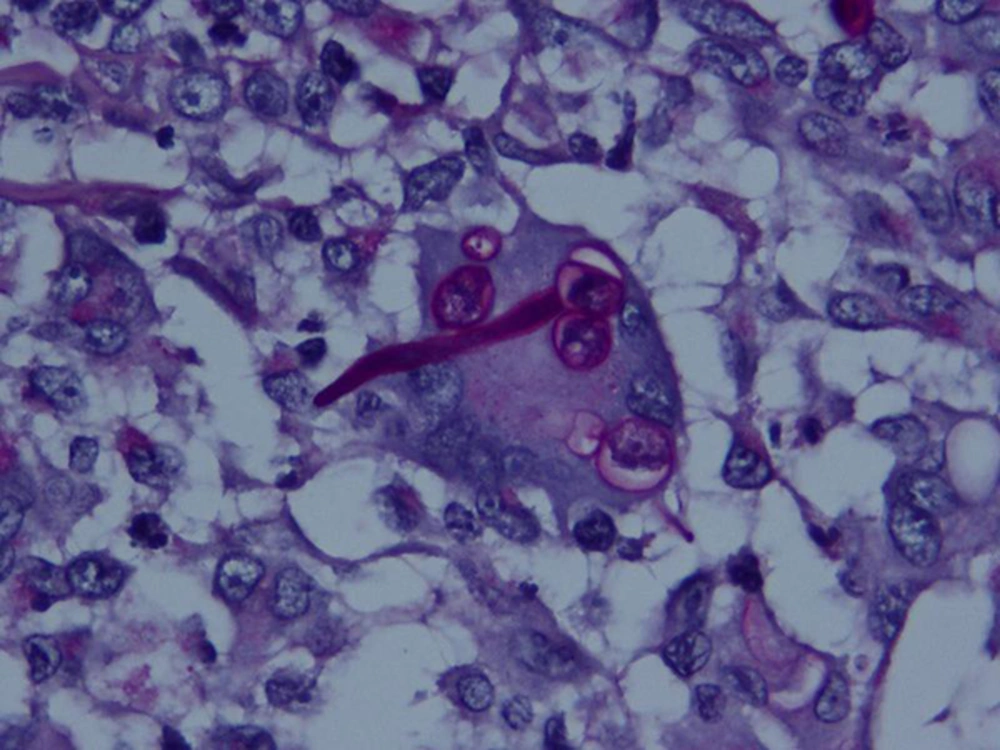
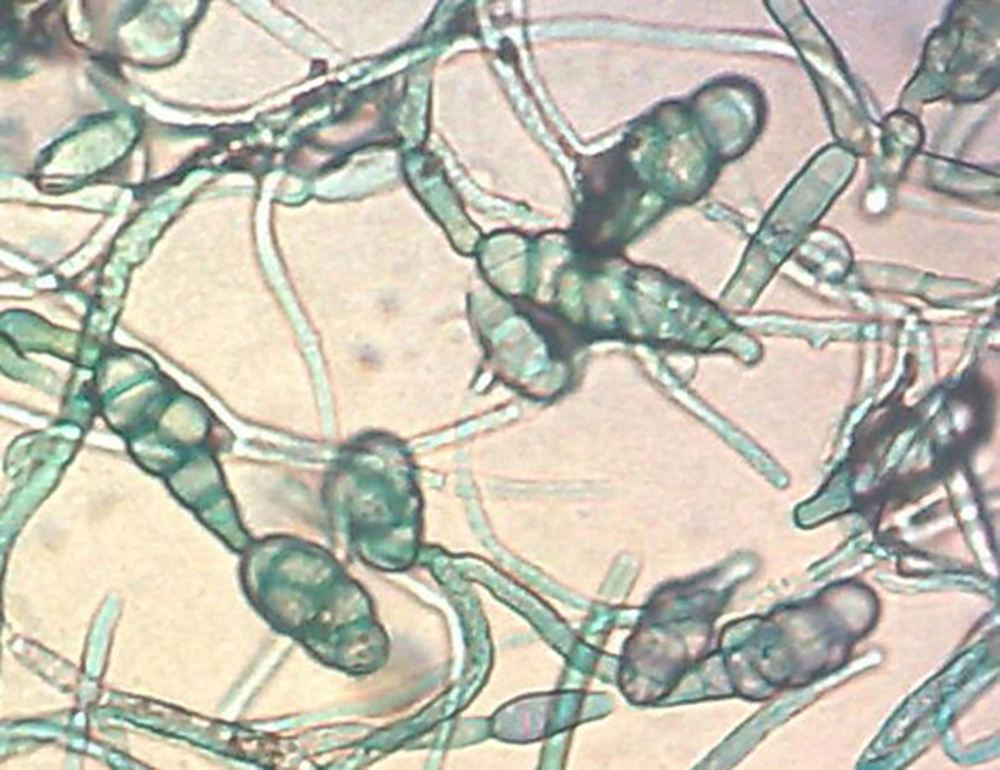
The pathological examination of biopsy taken from the lateral border of ulcerative lesion revealed that it had pseudoepithelial hyperplasia, polymorph plasma cells, inflammation areas with histiocytes and hypha like constractions among inflammatory cells (Figure 2). Coagulase negative staphylococci were assessed in specimen cultures. In mycological Sabouraud dextrose agar (Himedia, India) cultures, greenish-brownish grey colonies with black punctations on the middle mold colonies with a loose structure grew within 3 - 4 days. The colonies evaluated to have fulfilling the whole plaque, brown-greenish grey in color, black punctuations on the middle loose hypha structure (Figure 3). In micromorphological evaluation, hypha structure had compartments. At the distal ends of the structures, colorful macroconidia with dark brown colors, cylindrical, branching or breeding, horizontal or vertical comportments are detected (Figure 4). With these evaluations, the agent was thought to be Alternaria spp. The patient received 200 mg × 2/day itraconazole as treatment together with reduction in mycophenolate mofetil intake to 360 mg/day. Serum tacrolimus level inspected during antifungal treatment and reduced during itraconazole treatment. The macroscopic healing of the lesion was observed in the first two weeks and surgical nodulectomy performed in one month. The healing of lesion followed periodically and no recurrent or new lesion occurred.
3. Discussion
Although rare in normal individuals, Alternaria may be a cause of infection in immunosuppressed patients (3, 4). The port to enter the individual is usually the skin, which lost its uniform structure. Patients usually arrive with skin or subcutaneous infections. The infection may rarely appear as oculomycosis, sinusitis, onychomycosis and invasive infections (4, 5). In our case; there was no history of trauma, although the patient had skin infection. However, realizing the localization of skin lesions (elbows) implied that micro traumas had been the reason for skin infections. Cutaneous and subcutaneous Alternariasis cases may have visual clinical variations. In most patients, erythema, desquamation or red papule formation are inspected. Especially after corticosteroid treatments, erosions or ulcerations may develop. When the infection develops together with penetration caused by trauma, clinical view is like a purplish reddish plaque with an ulcer in the middle. Besides, in healthy patients, it can be seen as a crust ulcer form (1, 6). In our patient, nodular, crusted ulcerative form developed without trauma.
In our case, the molds grew in laboratory suggested Alternaria spp. due to colonial structure, hypha structure, localization of macroconidia on hyphae, horizontal or vertical compartments and tendency of change in compartments structures due to hypha localization. In a study of 156 Alternariasis patients, the rate of skin infections was 88.4% and subcutaneous infections as 11.6% (1). Among these patients, 60% were reported in the four Mediterranean Countries (France, Italy, Spain and Greece) and the average age was 54 (Ranged 6 - 94); the prevalence in men was 65% and 35% in women. The reason for a higher prevalence in men was probably a higher rate of exposure to external effects (1, 5). Although ours is a Mediterranean country, a very limited number of Alternaria cases were reported and according to the literature, this was the fifth case reported in Turkey (7-10).
In a study of 128 patients, predisposing factors of Alternariasis were 51 cases of transplantation (47 solid organ, 4 bone-marrow), 10 cases of Cushing Syndrome without receiving a transplantation and 67 cases of immunosuppressive treatment (1). Although the main cause of Alternariasis is A. alternata, (1), in a study of 156 cases, causative species were as follows; 59 (37.8%) A. alternata and 23 case (14.7%) A. tenuissima. Alternariasis or similar cases may be increased due to the increased number of immunosuppressed patients. From this point of view, skin lesions in these patients must be planned and microbiologically evaluated considering the molds.