1. Background
Acinetobacter species are emerging as one of the most important nosocomial pathogens that cause a variety of infections in patients, especially among those in intensive care units. These patients are at risk of different infections such as ventilator-associated pneumonia, bacteremia, surgical wound infections, meningitis and urinary tract infections (1). Due to resistance to multiple classes of antibiotics, only a few treatment options are available for carbapenem-resistant Acinetobacter baumannii (CRAB). Genetically mobile elements, including integrons, carry diverse arrays of resistant gene cassettes and promote the dissemination of resistance determinants (2). The transfer of integrons carrying resistance gene cassettes to other bacteria results in the emergence of resistance to multiple drugs (3). Acquired carbapenem resistance in Acinetobacter is often associated with acquired carbapenemase production, including OXA-23, OXA-24 and OXA-58 type class D carbapenemases (1).
The insertion sequence ISAba1 has been found to be of concern with several antibiotic-resistant genes, including blaOXA-23, blaOXA-58 and blaOXA-51, and it appears to provide the promoter required for gene expression (4). A strain that is resistant to at least three classes of anti-microbial agents, i.e. all 1) penicillins and cephalosporins (including inhibitor combinations), 2) fluoroquinolones and 3) aminoglycosides, is referred to as being multi-drug resistant (MDR). An MDR strain that is also resistant to imipenem is referred to as extensively drug resistant (XDR) (5). Major epidemiological features of this organism are its propensity for being spread clonally (6). MlVA typing of A. baumannii with eight variable number tandem repeat (MLVA-8), had been optimized by Pourcel et al. and compared with typing methods, including PFGE and SG profiling (7).
2. Objectives
Considering the paucity of epidemiological information on the genetic structure and prevalence of resistant genes in Iran, in this study, we applied MLVA-8 to the typing of an extensively drug-resistant A. baumannii isolates collected at two different hospitals in Tehran, Iran. We also evaluated the occurrence of OXA-like carbapenemase and integrons among XDR strains.
3. Materials and Methods
3.1. Bacterial Isolates
The study was conducted from March 2010 to November 2013 in two hospitals in Tehran, Iran. Acinetobacter was identified by conventional testing methods. One hundred and thirty one isolates were collected from specimens of affected patients, (e.g., sputum, urine, cerebrospinal fluid and pleural effusion).
3.2. Susceptibility Testing
Susceptibility testing to antibiotics, including tigecycline, colistin and other antimicrobial agents, was performed by disk diffusion method as recommended by the clinical and laboratory standards institute (CLSI) (8). Tigecycline (TGC 15 µg), colistin (CO 10 µg), imipenem (IMI 10 µg), meropenem (MEN 10 µg), gentamicin (GM 10 µg), ciprofloxacin (CIP 5 µg), Amikacin (AK 30 µg), cotrimoxazole (TS 25 µg), cefepime (CPM30 µg), cefotaxime (CTX 30 µg), aztreonam (ATM 30 µg), ceftazidime (CAZ 30 µg) and polymyxin B (PB 300 U) were obtained from MAST Pharmaceuticals, Inc. UK. Quality control was performed by testing the susceptibility of Escherichia coli ATCC 25922.
3.3. PCR Amplification
DNA was extracted from the isolates by boiling method (9). All isolates were subjected to multiplex PCR to detect the blaOXA-51-like gene that is unique to A. baumannii species (10, 11) and to detect the genes of the carbapenem-hydrolyzing oxacillinases OXA-23, OXA-58 and OXA-24 (12). PCR primers and the annealing temperature are listed in Table 1. Class 1, 2 and 3 integrons were detected using multiplex PCR, as described by Dillon et al. (13). A. baumannii strain ATCC 17978 and referenced strain COL 20820 was used as positive control for phenotypic tests and detection of bla OXA-51.
| Gene | Primer | Amplicon Size | Annealing |
|---|---|---|---|
| blaOXA-23F | GAT CGG ATT GGA GAA CCAGA | 501 bp | 53 |
| blaOXA-23R | ATT TCT GAC CGC ATT TCC AT | ||
| blaOXA-24F | GGT TAG TTG GCC CCC TTA AA | 246 bp | 53 |
| blaOXA-24R | AGT TGA GCG AAA AGG GGA TT | ||
| blaOXA-58F | AAG TAT TGG GGC TTG TGC TG | 599 bp | 53 |
| blaOXA-58R | CCCCTCTGCGCTCTACATAC | ||
| Isaba-1(F) | CACGAATGCAGAAGTTG | 1200 bp | 49 |
| OXA-23-R | TTAAATAATATTCAGCTGT | ||
| Int-1F | CAGTGGACATAAGCCTGTTC | 160 bp | 62 |
| Int-1R | CCCGAGGCATAGACTGTA | ||
| Int-2F | GTAGCAAACGAGTGACGAAATG | 788 bp | 62 |
| Int-2R | CACGGATATGCGACAAAAAGGT | ||
| Int-3F | GCCTCCGGCAGCGACTTTCAG | 979 bp | 62 |
| Int-3R | ACGGATCTGCCAAACCTGACT |
PCR Primers and the Annealing Temperature Used in This Study
3.4. Molecular Typing
MLVA was used to determine the epidemiological relationship among A. baumannii XDR isolates harboring integrons and carbapenem resistance genes according to Pourcel et al. and the variable number tandem repeat (VNTR) markers used were L-repeats VNTR, including Abaum3530, Abaum3002, Abaum2240, Abaum1988 and S-repeats VNTR, including Abaum0826, Abaum2396, Abaum3468 and Abaum0845 (7). The polymorphism indices of individual loci or combined VNTR loci and confidence intervals (CIs) were calculated using the Hunter-Gaston diversity index (HGDI) by hpa bioinformatic on line tools software (14, 15). The length of repeat, the number of repetitions and deduced sizes of the flanking regions were analyzed (16). Cluster analysis of the MLVA typing data was performed by MLVA plus online tools software.
4. Results
Using PCR for amplification of blaOXA-51, 123 of 131 Acinetobacter isolates were identified as A. baumannii. Thirty isolates (24.4%) were XDR. According to disc diffusion, these isolates were resistant to imipenem, gentamicin, ciprofloxacin, amikacin, cotrimoxazole, cefepime, cefotaxime, aztreonam and ceftazidime. Thirty percent of these XDR isolates were resistant to tigecycline based on the FDA criteria. All isolates were susceptible to colistin and polymyxin-B. The minimum inhibitory concentration (MICs) of imipenem and meropenem for the A. baumannii isolates ranged from 16 to 128 mg/L and 4 to 256 mg/L, respectively. According to the MICs, 30 (100%) of XDR A. baumannii isolates were resistant to imipenem and 29 (96.7%) were resistant to meropenem (MIC ≥ 16 mg/L). bla OXA-58 gene was not detected in XDR isolates.
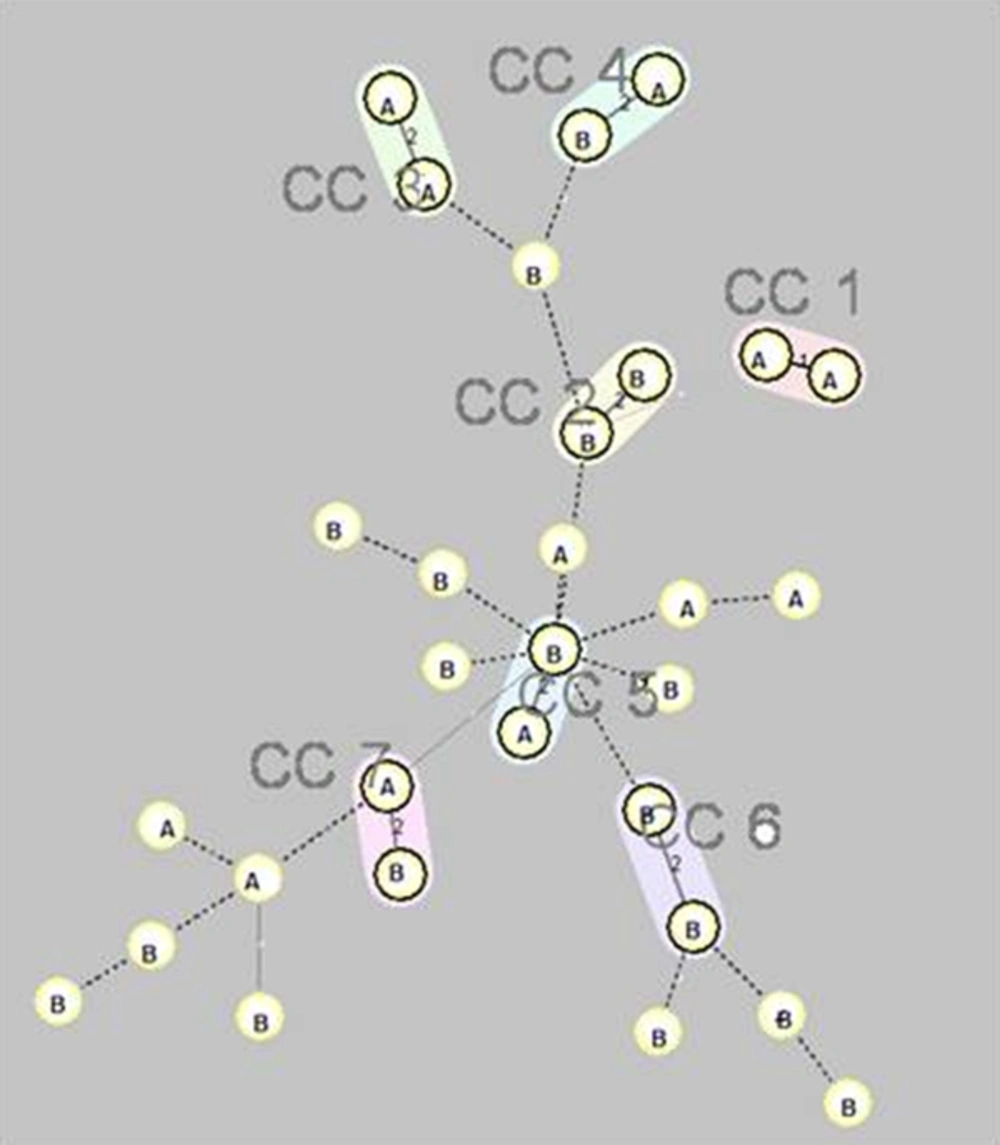
Twenty-eight XDR isolates (93.3%) had positive result for bla OXA-23-like and two (6.7%) for bla OXA-24-like. Using the ISAba1 forward primer and the OXA-23-like gene reverse primer, all isolates yielded a PCR amplicon of 1.2 kb, indicating the location of ISAba1 in the upstream region of the OXA-23-like gene of these isolates. Twenty-nine XDR isolates (96.7%) carrying class 1 integrons and 13 (43.3%) were carrying both class I and II integrons. Class III integrons were not detected. The MLVA typing of the XDR isolates showed seven clonally complexes and 16 singletons. Some isolates with the same clonally complex and obtained from the same ward, were different in the combination of resistance genes. Figure 1 shows the minimum spanning tree presentation of MLVA-8 clustering of the XDR strains. In our study, Abaum3468 had amplification failure.
Seven complexes (cc1 to cc7) are designated and marked by different halo colors. A distance of two loci is indicated by a thin line and a distance of three or more loci is indicated by a broken line. The letters inside the circles (A and B) indicate the name of hospitals.
5. Discussion
Genotyping XDR isolates by MLVA indicated that different strains were co-circulating within the two hospitals. This is the first population genetic study on A. baumannii by MLVA typing in Iran and we demonstrated that an XDR A. baumannii population in our hospitals was genetically diverse, which complicates preventive and infection control measures. Strain typing in another study also showed genotypic diversity within A. baumannii (17), but still other studies described them clonally (18, 19). This phenomenon could be due to the use of three S-repeats VNTR loci with high discriminative power in our study. The four L-repeats, i.e. Abaum3530, Abaum3002, Abaum2240 and Abaum1988, were distributed in the major clones, and the S-repeats, i.e. Abaum0826, Abaum0845 Abaum2396 and Abaum3468 provided a high level of discrimination. The diversity of MLVA S-VNTR markers, led to fine clustering of isolates.
Using pulsed-field gel electrophoresis (PFGE) along with MLVA can provide better tool for epidemiological interpretation that was not used in our study. In a French study, three loci, i.e. Abaum3002, Abaum3530 and Abaum 0826, had amplification failure (20). Nevertheless, in our study Abaum3468 had amplification failure. This reflects the fact that the distribution of the loci in different strains was not uniform. In all of the resistant strains examined, the bla-OXA-23 gene was along with to the insertion sequence ISAba1. The presence of bla-OXA-23 in several different MLVA types in different hospitals implies its mobility. Identification of common genetic elements (ISAba1-bla OXA-23 and the integrons) in isolates with different clonal complexes suggested that horizontal transfer occurred rather than clonally spreading of the isolates. Additional studies with longer period of time are needed to assess this phenomenon. In this study, we detected class I and class II integrons in A. baumannii in 96.7% and 43.3% of the clinical isolates, respectively.
Among 115 class 1 integron-positive isolates, 57 (49.6%) isolates were meropenem and imipenem resistant. There was no association between the presence of class 1 integron and resistance to imipenem and meropenem (P > 0.05); however, a significant association between XDR pattern and presence of class 1 integron (P < 0.001) was found. Since class I integrons carrying multiple resistance gene cassettes, association with XDR resistant strains is not unexpected. In an Australian study, a multiplex PCR method targeting the specific integrase genes (intI) for class I, II and III integrons failed to identify intII (encoding the class II integrase) or intIII (class III) in any isolate (4). In Thailand, among 63 MDR A. baumannii, 31 (67%) and 2 (4%) isolates carried class I and class II integrons. Class III integrons were not detected. The first report of class I integrons in multidrug-resistant A. baumannii in northwest Iran, showed that 92.5% of MDR A. baumannii carried class I integrons. The presence of class 1 integrons had a significant association with resistance in MDR-A. baumannii (21). Moreover, presence of class I and II integrons in 47 (53.4%) of MDR A. baumannii isolates was reported in southern Iran, while similar to the present study, class III integron was not detected (22). Our study showed resistance to most of the available antimicrobial agents for the treatment of infections caused by A. baumannii, except for polymyxin-B and colistin. The broad-spectrum in vitro activity of tigecycline and colistin may make them suitable candidates for use in the treatment of XDR A. baumannii.