1. Background
Viral hepatitis is a growing global public health concern both in developed and developing countries. In 2013, viral hepatitis was the seventh leading cause of death worldwide (1). There are several unrelated hepatotropic viruses causing wide spectrum of liver diseases ranging from simple steatosis infection to hepatocellular carcinoma (HCC). Hepatitis A virus (HAV), hepatitis B virus (HBV), and hepatitis C virus (HCV) are the major causative agents of acute viral infections. Hepatitis A virus infection occurs mostly in children, and accounts for an estimated 1.5 million cases each year. Unlike HBV and HCV, as the main chronic hepatitis viruses, HAV transmits enterically and the following infection is self-limiting and never leads to a chronic hepatitis (2, 3).
Unfortunately, despite therapeutic advances and effective vaccine for HBV, there are nearly 2 billion infected people and more than 240 million chronic carriers, worldwide (4). In addition, about 170 million people have been infected chronically by HCV and approximately 700000 deaths occur annually due to HCV-related liver disease (5). It must be noted that chronic carriers of HBV and HCV viruses are the source of new infections and serious liver diseases, such as cirrhosis, HCC, fulminant hepatitis failure (FHF), and encephalopathy due to super-infection caused by other hepatitis viruses, such as HAV or HDV (6-10).
Serological methods for detection of HBsAg and anti-HCV are routinely used in diagnostic laboratories. However, because of problems with serological assays, such as window period and occult hepatitis B/C infections among serologically negative patients, nucleic acid tests (NATs) are the gold standard for diagnosing of infections and following the treatments.
2. Objectives
The authors performed a molecular-based epidemiological survey to detect and evaluate HAV, HBV, and HCV infections and associated risk factors among patients with acute hepatitis manifestations.
3. Methods
3.1. Ethics Statement
This work was registered with grant No. GD-94118 and financially supported by infectious and tropical diseases research center, faculty of medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz.
3.2. Patients and Samples
The current study was conducted at the virology department of the Faculty of Medicine, Ahvaz Jundishapur University of Medical Sciences. During March to December, 2016, a total of 150 sera were collected from patients with elevated serum aminotransferase levels (at least 2 times greater than the upper reference value). All samples belonged to patients, who attended clinical laboratories in Ahvaz (Pasteur and Jahad Daneshgahi). Patients with fatty liver disease, cirrhosis, hepatocellular carcinoma, and genetic and metabolic disorders were excluded.
3.3. Serological Testing
All sera were tested for anti HAV IgM, HBsAg, and Anti-HCV, using the Enzyme Linked Immunosorbent Assay (ELISA) kit (Diapro, Italy), then stored at -70°C until used for DNA extraction and polymerase chain reaction (PCR).
3.4. Primers
5’-untranslated regions (5’-UTR) of HAV/HCV and X region of HBV (the highly conserved regions) were targeted to PCR detection. VP1/2A junction, S, and core regions of HAV, HBV, and HCV, respectively, were considered in genotype determination assays. By using NCBI Primer BLAST, it was proved that the primers did not attach to any other sequences except HAV, HBV, and HCV. The sequences of all used primers for detection and genotyping were picked from previous studies and shown in Table 1.
| Virus | Primer | Sequence (5’ - 3’) | Amplicon Size | Target Agene | Reference |
|---|---|---|---|---|---|
| HAV | Forward | TTGGAACGTCACCTTGCAGTG | 369 | 5’-UTR | (11) |
| Reverse (outer) | CTGAGTACCTCAGAGGCAAAC | 5’-UTR | |||
| Reverse (inner) | GAACAGTCCAGCTGTCAATGG | 330 | 5’-UTR | ||
| BR-5a (outer) | TTGTCTGTCACAGAACAATCAG | 361 | VP1/2A junction | (12) | |
| BR-9a (outer) | AGTCACACCTCTCCAGGAAAACTT | VP1/2A junction | |||
| RJ-3b (inner) | TCCCAGAGCTCCATTGAA | 234 | VP1/2A junction | ||
| BR-6a (inner) | AGGAGGTGGAAGCACTTCATTTGA | VP1/2A junction | |||
| HBV | Forward | GTCCCCTTCTTCATCTGCCGT | 139 | X gene | (13) |
| Reverse (outer) | GTTCACGGTGGTCTCCATG | X gene | |||
| Reverse (inner) | ACGTGCAGAGGTGAAGCGAAG | 118 | X gene | ||
| Forward | CGTGGTGGACTTCTCTCAATTTTC | 417 | S gene | (14) | |
| Reverse | GCCARGAGAAACGGRCTGAGGCCC | S gene | |||
| HCV | Forward (outer) | CACTCCCCTGTGAGGAACTACTGTC | 306 | 5’-UTR | (15) |
| Reverse (outer) | ATGGTGCACGGTCTACGAGACCTCC | 5’-UTR | |||
| Forward (inner) | TTCACGCAGAAAGCGTCTAGCCATG | 276 | 5’-UTR | (16) | |
| Reverse (inner) | GCGCACTCGCAAGCACCCTATCAGG | 5’-UTR | |||
| Forward (SC2) | GGGAGGTCTCGTAGACCGTGCACCATG | 440 | Core gene | ||
| Reverse (AC2) | GAGMGGKATRTACCCATGAGRTCGGC | Core gene | |||
| Forward (S7) | AGACCGTGCACCATGAGCAC | 416 | Core gene | ||
| Reverse (584) | CCCATGAGGTCGGCRAARC | Core gene |
3.5. Nucleic Acid Extraction
All sera were subjected to nucleic acid extraction using the high pure viral nucleic acid kit (Roche, Germany), according to the manufacturer’s protocol.
3.6. Assay Optimization
After optimizing of primer concentrations and MgCl2 in a final reaction volume of 50 µL, PCR detection of HAV, HBV, and HCV was performed. To determine the optimum annealing temperature, gradient PCR was set at 55°C to 65°C. The best condition for each virus was obtained and then samples along with negative (water) and positive controls (previously known PCR-positive samples of HAV, HBV, and HCV) were amplified.
3.7. HAV and HCV Genome Amplification
The reverse transcription polymerase chain reaction (RT-PCR) with the use of QIAGEN One-Step RT-PCR kit for HAV and HCV was set as follows: RT step 50°C/30 minutes, initial activation at 95°C/15 minutes, 40 cycles of 94°C/30 seconds, 58°C/30 seconds, 72°C/30 seconds, and a final extension step of 72°C/10 minutes. Nested PCR step using 5 µL of RT-PCR step products and inner primer sets of HAV and HCV was performed as follows: initial activation at 95°C/5 minutes, 40 cycles of 94°C/30 seconds, 58°C/30 seconds, 72°C/30 seconds, and a final extension step of 72°C/10 minutes. All reactions were performed at least twice and in the presence of negative and positive controls. The final products were detected by electrophoresis on 2% agarose gel containing DNA Safestain (Sinagene, Iran) under UV transilluminator (VILBERANT LUMART, France). The sizes of the PCR products were estimated according to the migration pattern of a 100-bp DNA ladder (Sinagene, Iran) (Figure 1).
3.8. HAV and HCV Genotyping Assay
Polymerase Chain Reaction-positive samples at the detection step were considered for genotype determination assays. The RT-PCR and nested PCR reactions were carried out like the previous step but this time with specific primers for HAV VP1/2A junction and HCV core region.
3.9. HBV PCR Detection and Genotyping
Molecular detection of HBV DNA was set as follows: initial activation at 95°C/5 minutes, 40 cycles at 94°C/30 seconds, 56°C/30 seconds, 72°C/30 seconds, and a final extension step of 72°C/10 minutes. Semi-nest PCR amplifications were performed similar to the first step with different reverse primers. Hepatitis B virus genotyping was carried out with the same conditions, but using other primer pairs which targeted the S gene on HBV DNA-positive samples. All reactions were performed in duplicate and in the presence of negative and positive controls. The final products were detected by electrophoresis on 2% agarose gel and the size of the PCR products were estimated by the migration pattern of a 100-bp DNA ladder (Figure 1).
3.10. Sequencing Analysis
Positive results from the second rounds of PCR amplifications were sequenced in both directions with the use of big dye terminator v3.1 cycle sequencing kit (Applied Biosystems), according to the manufacturer’s instructions. Forward and reverse sequences were aligned by BioEdit sequence alignment editor version 7.0.5.3 and consensus sequences were obtained. The sequences were deposited at GenBank under the accession numbers KX657751-KX657763 and MF673435-MF673437.
3.11. Phylogenetic Study
The MEGA6.06 software was used for phylogenetic analysis. The multiple sequences alignment of retrieved sequences from GenBank and the sequences of this study were achieved by CLUSTAL W. The bootstrap neighbor joining method with 1000 replicates was performed to determine the evolutionary distances.
3.12. Statistical Analysis
Data are reported as frequency and mean ± standard deviation (SD). The univariate and multiple logistic regression models (backward method) were used for analysis of risk factors. For analysis, SPSS software 22 was used and to test the hypotheses, the significance level was less than 0.05.
4. Results
4.1. Study Population
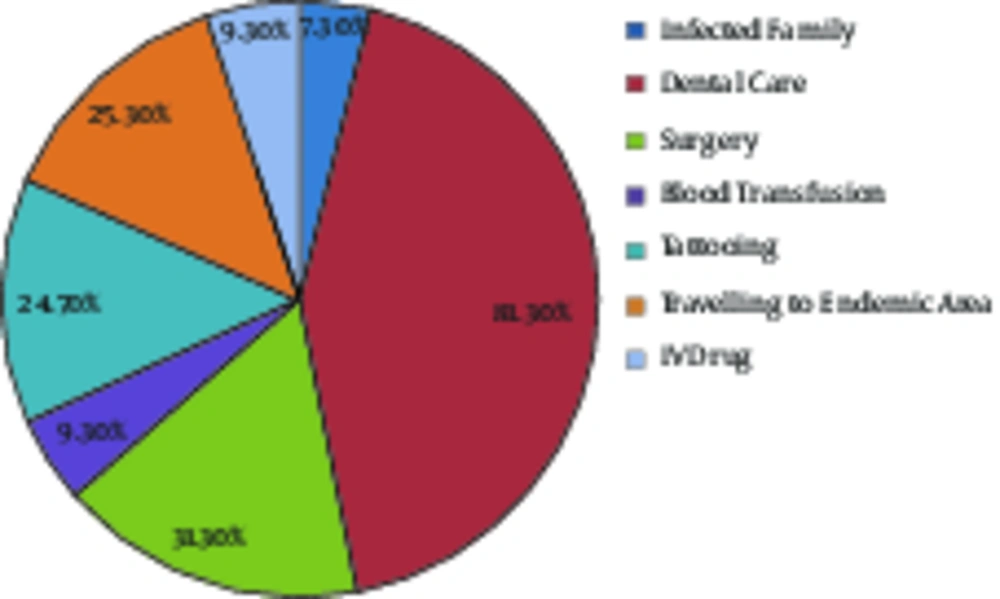
The study was carried out with 150 serum samples from patients with symptoms of acute hepatitis. All patients had high levels of alanine aminotransferase (ALT) and aspartate transaminase (AST). The group included 54 (36%) females and 96 (64%) males with a mean age of 34.25 ± 9.167 years, ranging from 8 to 65 years. The mean ALT and AST levels were 184.77 ± 120.12 and 90.86 ± 15.738, respectively. Distribution of risk factors among the 150 patients is shown in Figure 2.
4.2. Serological Findings
Out of 150 samples, 49 (32.6%), 32 (21.3%), and 38 (25.3%) were positive for anti-HAV, HBsAg, and anti-HCV, respectively. The characteristics of acute hepatitis infection are illustrated in Table 2.
| Variable | HAV RNA | HBV DNA | HCV RNA |
|---|---|---|---|
| Patients | 42 (28) | 28 (18.7) | 34 (22.7) |
| Male | 22 (52.4) | 19 (68) | 27 (79.4) |
| Age, y | 24.3 ± 5.9 | 37 ± 4.9 | 40 ± 5.6 |
| Mean value of ALT, IU/L | 229.74 ± 143.6 | 165.9 ± 101.01 | 173.3 ± 137.6 |
| Mean value of AST, IU/L | 98.5 ± 22.1 | 83.8 ± 9.2 | 90.5 ± 14.4 |
aValues are expressed as No. (%) or mean ± SD.
4.3. HAV Molecular Detection and Genotyping
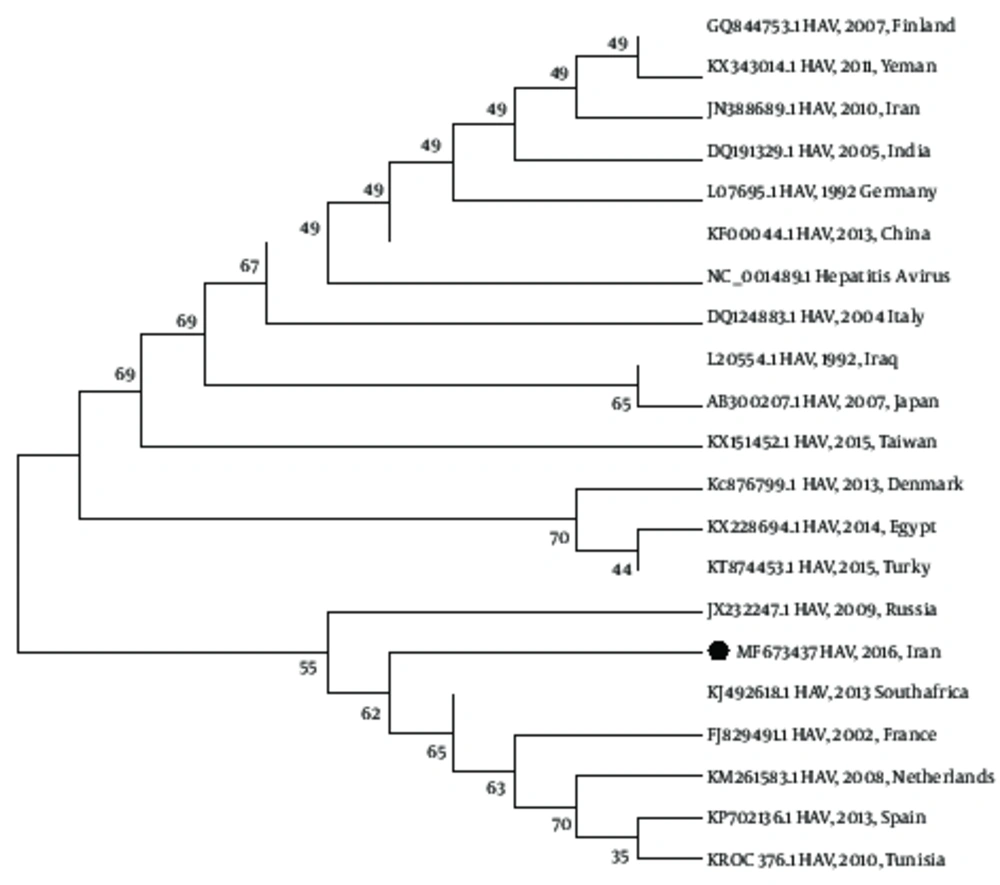
Forty-two of 150 samples (28%) were HAV RNA-positive by RT-PCR. All positive samples were HAV IgM positive as well. The mean range of ALT and AST of these patients were 229.74 IU/L and 98.48 IU/M, respectively. Genotyping via specific primers for VP1/2A region as well as data analysis suggested that all HAV isolates belonged to genotype IB (Figure 3).
4.4. HBV Detection and Genotyping
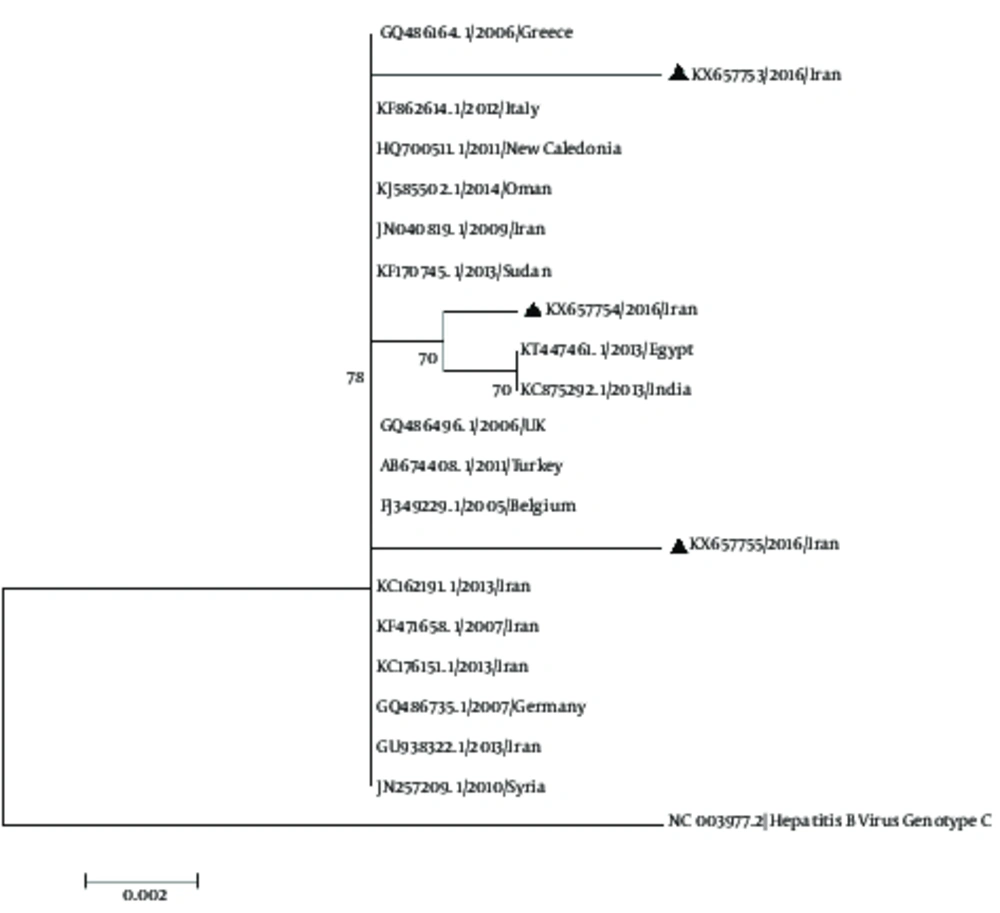
Hepatitis B virus DNA was detected in 28 (18.7 %) of 150 samples, using semi nested PCR. All cases were HBsAg-positive and the mean ALT and AST levels for these patients were 165.9 IU/L and 83.8 IU/L, respectively. These positive samples were subjected to additional PCR amplification on the S gene for genotype determination. The multiple alignments of obtained HBV sequences from this study and those retrieved from GenBank database (representing all 8 genotypes) indicated that all sequences were consistent with genotype D (Figure 4).
A phylogenetic tree based on 393 nt of the HBV S region. The bootstrap neighbor joining method with 1000 replicates was performed to determine the evolutionary distances. HBV genotype C was utilized as an out-group. Sequences are defined by accession number/year/origin of the strain, respectively. The sequences related to this study are marked.
4.5. HCV Detection and Genotyping
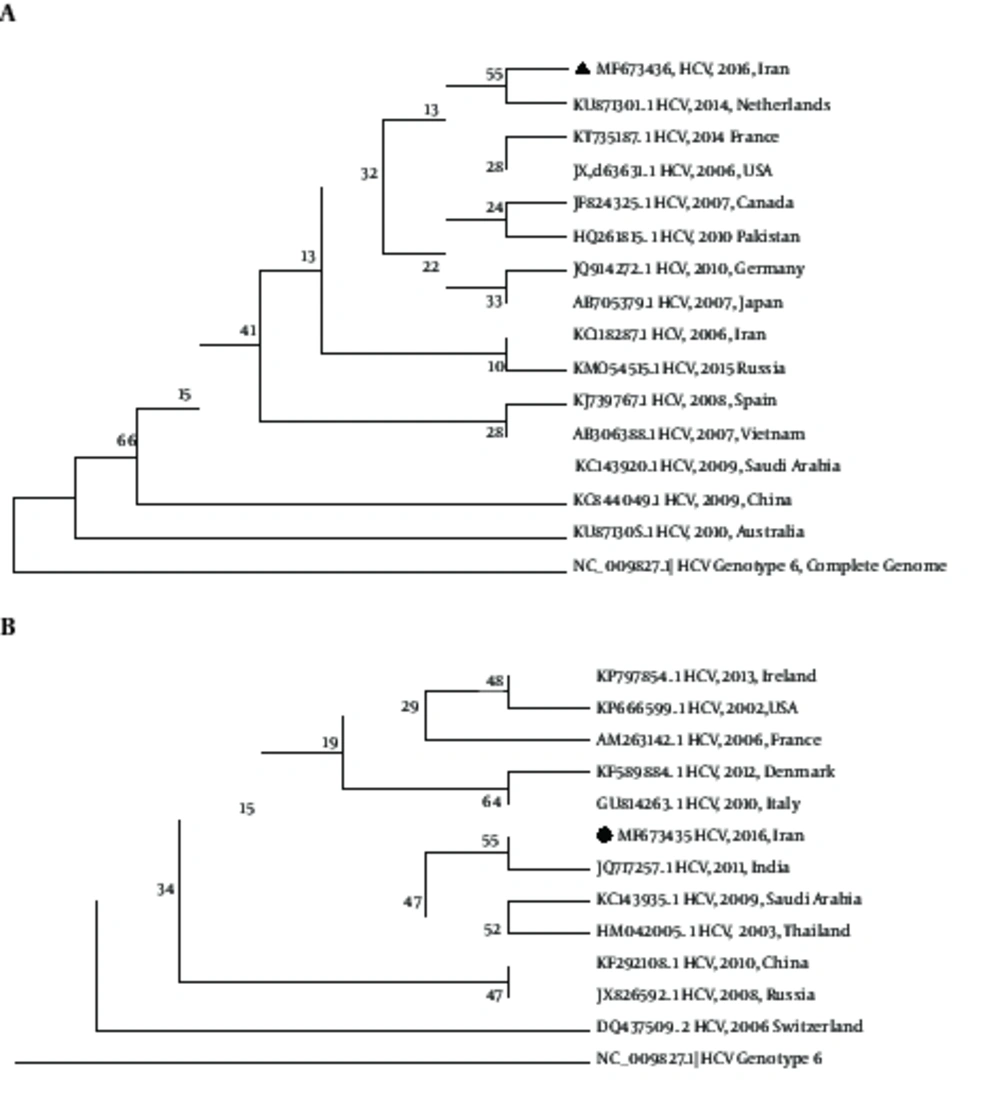
Overall, 34 of 150 (22.7%) samples were positive using RT-PCR, aimed at the HCV 5’-UTR. The mean value of ALT and AST levels in HCV RNA-positive patients were 173.3 IU/L and 90.5 IU/L, respectively. For genotype detection, core region was amplified and comparison between acquired sequences and previously reported sequences indicated that HCV RNA-positive samples could be classified to genotypes 1a (13/34, 38.2%) and 3a (21/34, 61.7%) (Figure 5).
Neighbor-joining phylogenetic tree for core region of HCV genotype 1 (A) and HCV genotype 3 (B). Bootstrap values for 1000 replicates are given on the branches as percentages. HCV genotype 6 was utilized as an out-group. All sequences are defined by accession number / year / origin of the strain, respectively. The obtained strains from this study are marked.
5. Discussion
This research conducted a molecular-based epidemiological survey to detect viral hepatitis in patients with acute hepatitis. In the current study, the total seroprevalence of HAV, HBV, and HCV was found to be 79.3% (119/150). There was not any difference in the prevalence of acute viral hepatitis among the patients, when stratified according to gender. As indicated, in the present study, nearly 20% of sera were negative for HAV, HBV, and HCV. It should be noticed that there are also other viruses causing acute hepatitis, such as HDV, HEV, GB virus C, EBV, B19, herpes simplex virus, etc., which were not considered in this survey (17-21). Therefore, in the current study, HAV, HBV, and HCV-negative cases might be infected with other hepatitis viruses. Thus, further investigation is required for better understanding of the role and epidemiology of viral hepatitis in extension and transmission of liver diseases.
According to the data from the centers for disease control and prevention (CDC), Iran is an endemic region for HAV infection and there is no significant difference in genders (2, 22, 23). In the current study, the overall seroprevalence of anti-HAV and HAV RNA was 32.6% and 28%, respectively, and phylogenetic analysis suggested that all HAV isolates belonged to genotype IB. The mean age of patients with acute HAV infection was lower than those with acute hepatitis B or C (Table 2). The mean of ALT and AST levels in HAV-infected cases were higher than those with HBV and HCV infections (Table 2). Considering several studies, the prevalence of HAV in the country was about 51% to 66% and as Nejati et al. published in 2012, the predominant circulating genotype was IB (12, 23). However, further epidemiological studies are needed to clarify HAV diversity in other regions of Iran. In this study, the associated risk factor for HAV infections was found to be in touch or close contact with an infected relative, but after multivariate analysis using logistic regression, no significant difference was found (Tables 3 and 4). Hepatitis A Virus is transmitted primarily by the fecal-oral route, and vaccination along with health education for improving the sanitation, is the most successful way to control the infection in endemic areas.
| Risk Factor | HAV | HBV | HCV | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neg. | Pos. | P Value | OR | Neg. | Pos. | P Value | OR | Neg. | Pos. | P Value | OR | |
| Infected relative | 0.042 | 3.43 | 0.966 | 0.96 | 0.287 | 0.32 | ||||||
| No | 103 (95.4) | 36 (85.7) | 113 (92.6) | 26 (92.9) | 106 (91.4) | 33 (97.1) | ||||||
| Yes | 5 (4.6) | 6 (14.3) | 9 (7.4) | 2 (7.1) | 10 (8.6) | 1 (2.9) | ||||||
| Dental care | 0.695 | 1.21 | 0.903 | 1.07 | 0.410 | 0.68 | ||||||
| No | 21 (19.4) | 7 (16.7) | 23 (18.9) | 5 (17.9) | 20 (17.2) | 8 (23.5) | ||||||
| Yes | 87 (80.6) | 35 (83.3) | 99 (81.1) | 23 (82.1) | 96 (82.8) | 26 (76.5) | ||||||
| Surgery | 0.001 | 0.03 | 0.096 | 0.41 | 0.009 | 2.87 | ||||||
| No | 62 (57.4) | 41 (97.6) | 80 (65.6) | 23 (82.1) | 86 (74.1) | 17 (50) | ||||||
| Yes | 46 (42.6) | 1 (2.4) | 42 (34.4) | 5 (17.9) | 30 (25.9) | 17 (50) | ||||||
| Blood transfusion | 0.244 | 0.40 | 0.27 | 0.31 | 0.438 | 0.54 | ||||||
| No | 96 (88.9) | 40 (95.2) | 109 (89.3) | 27 (96.4) | 104 (89.7) | 32 (94.1) | ||||||
| Yes | 12 (11.1) | 2 (4.8) | 13 (10.7) | 1 (3.6) | 1210.3 | 2 (5.9) | ||||||
| Tattooing | 0.003 | 0.05 | 0.137 | 1.96 | < 0.001 | 4.80 | ||||||
| No | 72 (66.7) | 41 (97.6) | 95 (77.9) | 18 (64.3) | 96 (82.8) | 17 (50.0) | ||||||
| Yes | 36 (33.3) | 1 (2.4) | 27 (22.1) | 10 (35.7) | 20 (17.2) | 17 (50) | ||||||
| Travelling to endemic area | 0.002 | 0.10 | < 0.001 | 4.97 | 0.862 | 1.08 | ||||||
| No | 72 (66.7) | 40 (95.2) | 99 (81.1) | 13 (46.4) | 87 (75) | 25 (73.5) | ||||||
| Yes | 36 (33.3) | 2 (4.8) | 23 (18.9) | 15 (53.6) | 29 (25) | 9 (26.5) | ||||||
| IV drug | 0.998 | 0.00 | 0.660 | 0.70 | 0.058 | 2.89 | ||||||
| No | 94 (87) | 42 (100) | 110 (90.2) | 26 (92.9) | 108 (93.1) | 28 (82.4) | ||||||
| Yes | 14 (13) | 0 (0.0) | 12 (9.8) | 2 (7.1) | 8 (6.9) | 6 (17.6) | ||||||
aValues are expressed as No. (%).
| Virus | Risk Factor | B | S.E | Wald | df | P Value | OR |
|---|---|---|---|---|---|---|---|
| HAV | Age | -0.336 | 0.066 | 25.706 | 1 | 0.001 | 0.72 |
| AST | 0.050 | 0.031 | 2.593 | 1 | 0.107 | 1.05 | |
| Tattooing | -4.815 | 3.613 | 1.776 | 1 | 0.183 | 0.01 | |
| IV drug | -19.506 | 8556.313 | 0.000 | 1 | 0.998 | 0.00 | |
| Constant | 5.484 | 3.487 | 2.473 | 1 | 0.116 | 240.74 | |
| HBV | AST | -0.065 | 0.023 | 8.046 | 1 | 0.005 | 0.94 |
| Surgery | -1.263 | 0.573 | 4.865 | 1 | 0.027 | 0.28 | |
| Travelling to endemic area | 1.594 | 0.477 | 11.169 | 1 | 0.001 | 4.92 | |
| Constant | 3.978 | 1.988 | 4.003 | 1 | 0.045 | 53.41 | |
| HCV | Age | 0.099 | 0.030 | 11.123 | 1 | 0.001 | 1.10 |
| Tattooing | 1.274 | 0.446 | 8.179 | 1 | 0.004 | 3.58 | |
| Constant | -5.238 | 1.142 | 21.024 | 1 | 0.001 | 0.01 |
Iran is classified as an area with low to intermediate prevalence of HBV. The estimated rate of HBV infection in this country is about 3%, and is higher in males than females (2.55% versus 2.03%, respectively). Previous epidemiological studies indicated that HBV genotype D is the most prevalent genotype in Iran (24-28). In the current study, the S region was analyzed to determine HBV genotypes and data revealed that all HBV sequences had molecular characteristics of genotype D. Compared with the RefSeq and original GenBank resources, five substitutions were found at the nucleotide level, G362T, C391G, A543C, T562C, and C584G, all of which were missense (C121F, R131G, Q181H, S188P and S195W). In the current study, the multivariable analysis showed that the risk of acute hepatitis B infection increased nearly 5 times by traveling to the endemic area (Table 3 and 4). Hepatitis B Virus transmits by contact with contaminated body fluids, such as blood, blood products, and semen. The national HBV vaccination program for newborn and healthcare workers in Iran was started since 1993. However, a major proportion of community is unvaccinated and susceptible to the infection. Therefore, HBV vaccination as well as consultation services about the serious risks of blood-borne pathogens among unvaccinated people traveling to areas with intermediate or high prevalence of HBV infection is essential.
In the present study, HCV prevalence rate was estimated through the amplification of 5’-UTR, a highly conserved region among all genotypes, especially genotypes 1 to 6. Since the study of sequence diversity among different isolates is crucial, especially for analyzing response to therapy, sequencing of other regions, such as core and NS5B, is recommended for achieving high accuracy of virus dynamics and genotyping (29-32). Iran is categorized as a low-HCV prevalence region and HCV seroprevalence can vary from 0.08% to 1.6% in different provinces (32-34). Like many European countries, the predominant HCV genotypes among Iranian patients are 1 and 3, while in other Middle East countries, the main genotype is 4. During the recent years, the pattern of HCV genotypes has changed in the country and a shift in prevalent subtype from 1a to 3a was noticed.
The current results are in line with this observation and genotype 3a was found as the most prevalent HCV genotype (61.7%). This is probably associated with the increase of Intravenous Drug Users (IDUs) and needle sharing, since genotype 3 is commonly found in IDUs. According to the reports of CDC, Intravenous (IV) drugs and needle sharing are the most common risk factors for infection with HCV in many countries. However, the current results indicated that tattooing has a significant relationship with HCV infection in Ahvaz city and can increase the risk of infection by 3.5 times (Table 4). It has been declared that the risk of HCV infection rises with increasing of covered areas and the number of tattoos (35). Since tattooing is especially popular among young people, a comprehensive educational program should be performed about the important risk of blood borne infections for the youth community.
6. Conclusions
The current study showed the molecular epidemiology of circulating viral hepatitis in the country and may contribute to the information on the genetic diversity of viral hepatitis worldwide. It can also underlines the necessity of further studies and evaluation of preventive programs, such as rigorous screening and treatment, vaccination in high risk groups, social services like the needle exchange program (NEP) and consultation among young people to reduce risk factors in the country.