1. Background
The incidence of opportunistic fungal infections, particularly candidiasis, is increasing in immunocompromised patients, due to taking long-term antifungal agents, hospitalization, organ transplantation, and malignancies (1, 2). Candida albicans are considered as an important opportunistic pathogen with the unique characteristic of transition of yeast form to hyphae (3), which leads to serious life-threatening infection in cases with immunodeficiency disorders (4, 5). Based on worldwide reported cases, antifungal resistance in Candida species is emerging. Biofilm formation in Candida spp. is known as a major factor associated with drug resistance and development of pathogenicity, causing failure of therapeutic strategies (3, 6).
Previous studies have indicated that a network of genes are responsible for biofilm formation, and progress of growth and extension to the infected site. Hyphal wall protein (Hwp1) exerts a vital adhesion molecule and has a significant role in the pathogenicity of C. albicans and accelerates their ability to change yeast form to hyphae, which contributes to biofilm formation (5). One specific feature of Candida species biofilms is protection of the fungal population against host immune system defenses and antifungal drug diffusion. Therefore, new therapeutic strategies towards inhibition or control of the biofilm development seems to be a critical concern (1, 3, 5, 6).
Broad and prolonged utilization of currently available antifungal drugs, mostly the azoles, for treating Candida infections results in the emergence of azole-resistance in C. albicans strains (1, 3, 7). Consequently, the use of new metal nanoparticles is highly considered as a potential promising antifungal strategy. A variety of synthetized nanoparticles with antifungal properties are under evaluation. It has been established that zinc oxide nanoparticles (ZnO NPSs) have appropriate antifungal traits; however, ZnO may increase the effectiveness of antifungal agents (1-3, 8-10). Moreover, in a recent study reported by Barad et al., zinc oxide nanoparticles coated by chitosan and chitosan-linoleic acid showed enhanced antifungal properties (1). The antimicrobial activity of different forms of chitosan has been little studied previously (11-13). Neutrophils and macrophages are inflammatory phagocytes that induce reactive oxygen species (ROS) production as a defense mechanism towards microbes or other agents. On the other hand, several investigations proved that different nanoparticles comprised of metal oxide particles can induce ROS production in inflammatory phagocytes (14, 15).
2. Objectives
Herein, this study evaluated ZnO NPs activities on the expression of Hwp1 gene in C. albicans, using real-time PCR. In addition, the effect of ZnO NPs on generation of ROS from BALB/c mouse macrophage as well as its cytotoxicity on HepG2 cells were examined.
3. Methods
3.1. Ethics Statement
This research approved by ethics committee of Tarbiat Modares University, Tehran, Iran (IR.PMU.REC 1392.335).
3.2. Microorganisms and Media
In this study, a standard strain of Candida albicans (ATCC10231) and a determined fluconazole resistant clinical species of C. albicans isolated from vulvovaginal candidiasis was selected and cultured on Sabouraud Dextrose Agar (SDA, Sigma Aldrich, USA). ZnO NPs were synthesized and coated by linoleic acid conjugated with chitosan to increase antifungal activity, according to a method described previously (1). Briefly, chitosan (CS) was conjugated to linoleic acid (LA), and CS-LA was added to ZnO nano particles. The CS-LA coated by ZnO nano particles were collected by centrifugation and washed using distilled water. This solution was stored in the refrigerator until use. Antifungal activity of nanoparticles was tested using the minimum inhibitory concentration (MIC) of ZnO NPs against the standard species and fluconazole resistant clinical isolate, according to Clinical Laboratory Standard Institute protocol (CLSI M27-S3). For this purpose, the yeast cells were diluted in sterile phosphate buffer (PBS) and 1 × 103 yeast cells were prepared and seeded on 96-well microplates, containing the RPMI medium (Gibco, Thermo Fisher Scientific, USA). Different concentrations of nanoparticle (0.25 to 128 µg/mL) was added to the suspension and incubated at 37ºC for 24 hours. In each serial, one positive control with no nanoparticle and one negative control with no fungal suspension were designed (1).
3.3. Reactive Oxygen Species Production
Peritoneal exudates macrophages were harvested by peritoneal lavage of BALB/c mice (16). In summary, 1 × 103 cells/well was added to 96-well flat-bottomed plates (Nunc, Thermo Fisher Scientific, Germany), followed by incubation at 37°C for four hours under humidified 5% CO2 atmosphere. The non-adhering cells were then removed by washing the wells three times with PBS. The adherent cells were incubated for the desired time and cultured in complete RPMI 1640 medium and different concentrations of MIC and higher doses, including 32, 64, and 128 μg/mL of ZnO NPs was added to macrophage culture as triplicate wells with final volume of 200 μL/well as the positive control and unstimulated macrophages were considered as negative controls, respectively. The cultured cells were incubated at 37°C for 48 hours under humidified 5% CO2 atmosphere. The two groups of cells were evaluated for generation of ROS using Dichlorofluorescein Diacetate (DCFH-DA) (Sigma-Aldrich, USA) clarified by Carlson et al. (17).
3.4. Cell Cytotoxicity Assay
The effects of ZnO NPs on the viability and proliferation of HepG2 cells (purchased from institute Pastor, Iran) was investigated using the MTT assay (18). For this purpose, the HepG2 cells were seeded at a density of 1 × 104 in 96-well plates and incubated with different concentrations of ZnO NPs (32, 64, and 128 μg/mL) for 48 hours. Then, appropriate amounts of MTT (3-(4, 5-dimethylthiazol-2yl) 2,5-diphenyltetrazolium bromide) (Sigma Aldrich, USA) (5 mg/mL in PBS) was added to wells and the plates were incubated for four hours. The supernatants were then gently removed, and isopropanol and HCl (Sigma Aldrich, USA) was added for dissolving the formazan crystals. The plates were incubated overnight and the absorbance of each well was measured by the enzyme linked immunosorbent assay (ELISA) reader (Multiskan MS, England), at a wavelength of 540 nm.
3.5. Biofilm Formation and MTT Assay
Biofilm formation of standard and clinical isolates of C. albicans were examined using the MTT assay. Initially, 1 × 106 of yeast cells of Candida were cultured on 96 sterile flat-bottom-well microplates, containing yeast nitrogen base, YNB (Merck, Germany), incubated at 37°C for 90 minutes to grow the yeast cells biofilm. Later, free-living cells were washed and biofilm formation was assessed by adding 200 μL of YNB with 50 mM glucose. The plates were incubated at 37°C for 48 hours, and after this time, different concentrations of ZnO nanoparticles was added to each well and the biofilm was made by adherent yeast cells. Also, the untreated cells were considered as the control group. Finally, the MTT salt was added to each well, incubated for four hours, and then DMSO was added to wells and optical absorbance was measured at wavelength of 540 nm (19) by the ELISA reader (Memmert, Germany).
3.6. RNA Extraction, cDNA Synthesis and Real-Time PCR
The expression level of Hwp1 gene in ZnO NPs-treated and untreated C. albicans strains was compared using real-time PCR. RNA extraction of C. albicans was carried out using glass beads and the denaturing buffer agents in an RNase-free environment, as explained previously (7). For eliminating genomic DNA contamination, the extracted RNA was treated with one unit of DNaseI (Fermentas, Thermo Fisher Scientific, Germany) per 10 μL of RNA at 37°C for one hour. The cDNA was synthesized using a two-step RT-PCR kit (Vivantis, Malaysia) and then used in real-time PCR assay. SYBR® Green I (Fermentas, Thermo Fisher Scientific Inc., Germany) was used for detection of genes amplification as follows; denaturation at 95°C for five minutes, annealing for 30 seconds at 65°C for ACT1 and at 58° C for Hwp1, and elongation at 72°C for 10 seconds, followed by final termination for 30 seconds at 72°C. Each reaction was normalized by ACT1 gene as a housekeeping gene. The PCR primer sequence was used in this study, as shown in Table 1.
| Primer Name | Sequence (5' → 3') | PCR Product Size (bp) |
|---|---|---|
| ACT1-F | CCAGCTTTCTACGTTTCC | 200 |
| ACT1-R | CTGTAACCACGTTCAGAC | 572 |
The Nucleotide Sequence of Primers Used for Real Time PCR Amplification in This Study
3.7. Statistical Analyses
Statistical analyses were conducted using the Statistical Package for Social Sciences (SPSS), version 18.0 released for Microsoft Windows (SPSS Inc, Chicago, Illinois). The mean of the Ct of Hwp1 gene before and after treatment by ZnO NPs is expressed as a mean ± standard deviation. The levels of ΔCt of the Hwp1 gene before and after incubation with NPs were compared using paired t-test, separately. In all tests, a P value of less than 0.05 was considered significant.
4. Results
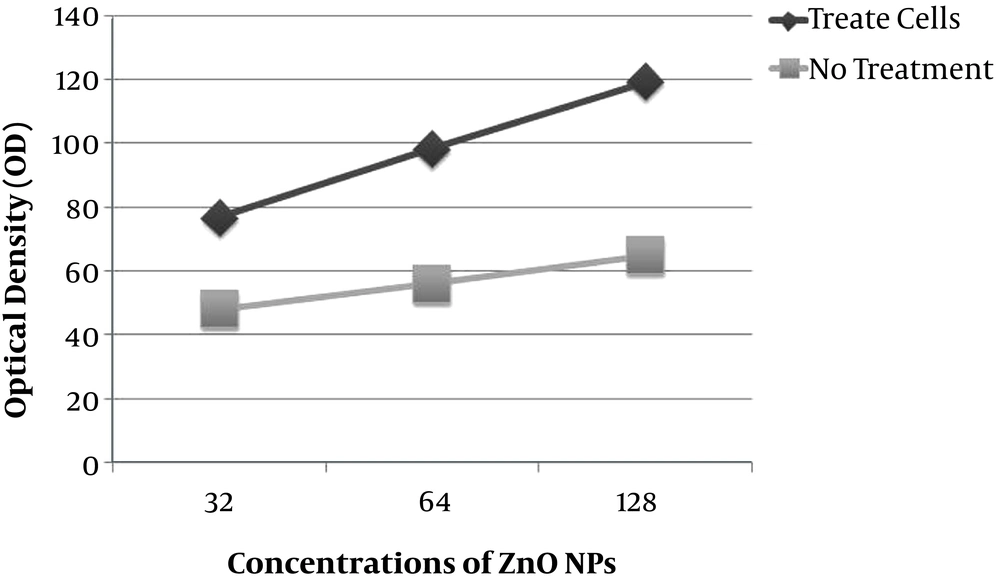
4.1. ROS Generation by Macrophages of BALB/c Mice
Reactive oxygen species generation was measured by fluorescein diacetate (DCFH-DA). For this, 1 × 106 macrophages, obtained from BALB/c mice, were treated with 32, 64 and 128 μg/mL of ZnO NPs in a 96-well plate against a control group for 24 hours and then, fluorescence intensity of Dichlorofluorescein (DCF) was assessed by SpectraMAX Gemini plus fluorescent microplate reader. These findings showed that the amount of ROS production by macrophages exposure to ZnO NPs increased significantly in all tested concentrations compared to the control group without any nanoparticle treatment (P = 0.001). Indeed, the highest level of ROS was produced at concentration of 128 μg/mL of ZnO NPs, however, it occurred in a dose-dependent manner. These data are shown in Figure 1.
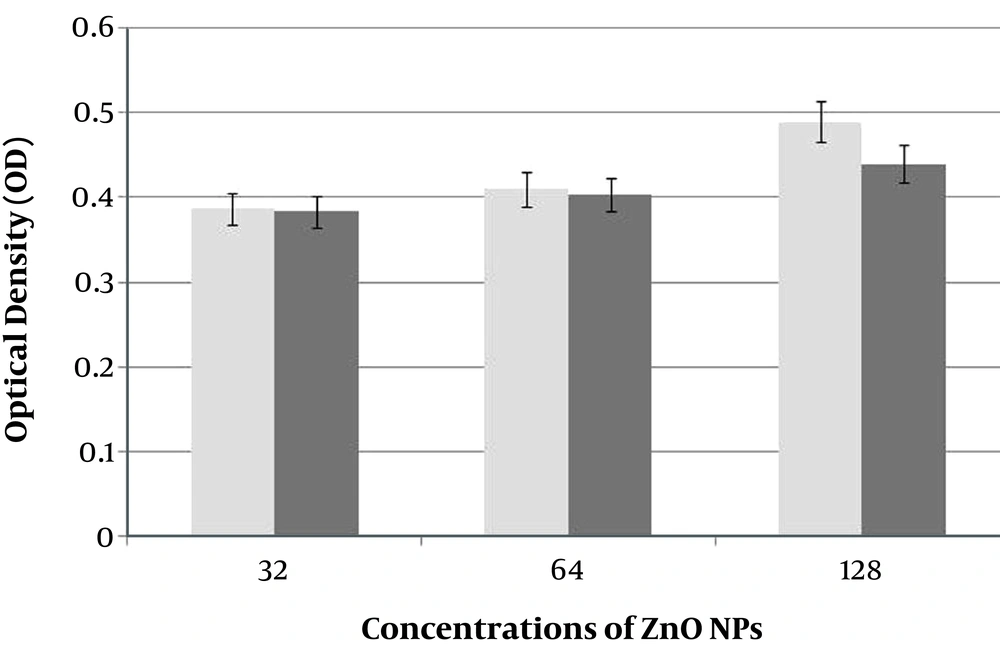
4.2. Cytotoxicity Assay on HepG2 Cells
The cytotoxicity of ZnO NPs on HepG2, hepatocellular carcinoma cell line, was evaluated. The MTT analysis demonstrated that there was a significant difference between ZnO NPs treated cells and non-treated cells at different concentrations of nanoparticle (Figure 2). This means that this nanoparticle did not show any cytotoxic effect on HepG2 cell line in vitro.
4.3. Biofilm Formation
The ability of biofilm formation of C. albicans was evaluated using the MTT assay. The obtained results indicated that treatment of C. albicans with ZnO nanoparticles significantly decreased yeast cells biofilm formation at MIC concentration for ZnO nanoparticle in comparison with control groups without treatment (P = 0.006).
4.3. The Effect of ZnO NPs on Hwp1 Gene Expression of C. albicans
The effect of NPs on CandidaHwp1 gene expression was assessed by q-real-time PCR before and after treatment of C. albicans at 32 μg/mL and 128 μg/mL concentration of NPs. Total RNA was extracted from isolates, cDNA was synthetized, and q-real-time PCR was performed using a specific primer of Hwp1 and ACT1 genes as a housekeeping control. Results of paired t-test showed that exposure of Candida to NPs significantly decreased mRNA levels of Hwp1 gene in the standard strain and clinical isolate of Candida (P = 0.001) (Table 2).
Comparison of the Levels of ΔCt of the Hwp1 Before and After Exposure with ZnO NPs
5. Discussion
It has been established that biofilm formation in Candida species is required for adhesion, which leads to persistence of infection and invasion to host cells, especially in immunocompromised and/or hospitalized patients with underlying disease. There is a cluster of genes that contribute to biofilm formation in Candida species (20-22). Hyphae cell wall proteins are the most well-known C. albicans surface protein and link to cell wall glucan through a remnant of its GPI anchor. The critical role of Hwp1 in biofilm formation at the in vitro and in vivo levels has been shown (23, 24). Biofilms cause clinical complications with inherent resistance to antifungal treatments (25). Nowadays, exploration for new approaches with antifungal activity has become an urgent necessity, however, the mechanism of biofilm resistance is not entirely recognized. Previously published data indicated that ZnO NPs has inhibitory activity against fungi and bacteria (2, 8, 10). It has been shown that chitosan (CS) has wide application in biomedical and pharmacology because of its non-toxicity and unique biological and physiochemical properties as well as antimicrobial activity. Indeed, linoleic acid (LA) comprised of Trans-11 and Cis-9 is one of the appropriate acids that inhibits fungal cell growth (26, 27).
Thus, in this study new nanoparticles were designed, known as ZnO NPs, and their efficacy on inhibition of C. albicans biofilm formation and the expression level of Hwp1 gene and ROS generation by mice macrophages was examined. Previous findings showed that ZnO NPs successfully inhibited C. albicans growth in a respectable concentration compared to fluconazole, a conventional antifungal drug (1). In the present study, the researchers found that ZnO NPs significantly decreased Hwp1 expression in C. albicans cells treated with ZnO nanoparticle. It may be concluded that this nanoparticle may act a critical prevention of biofilm formation via influence on Hwp1 gene and contribute to limitation of infection spreading. Some studies confirm the current findings. In a prior study performed by Monteiro et al., the effect of different concentrations of silver nanoparticles (SN) on matrix composition and structure of Candida biofilms was evaluated (28).
The results showed that SN changed the biofilm structure, compared to the control group without NP treatment, also SN nanoparticle induced damage on cell wall of the Candida. In a recent experiment, chitosan-zinc oxide/polyaniline (CS-ZnO/PANI) composite was examined against C. albicans and relatively greater activity was observed than the known antibiotics and CS-ZnO alone. In addition, the antimicrobial activity of CS-ZnO/PANI composite against established biofilms was also tested and showed more than 95% inhibition of biofilm formation (29). In another study, Oilin et al. revealed that the novel gold nanoparticles (AuNPs) powerfully inhibited pathogenic biofilm formation and invasion to dental pulp stem cells (DPSCs). More examinations denoted that its mechanism was strongly related to binding AuNPs to the pathogen cells, which probably accomplished their inhibitory activity on biofilm formation and invasion (30). Wady et al. firstly assessed the effect of a silver nanoparticle (AgNPs) solution against C. albicans and indicated AgNPs solution had antifungal activity. In contrast of the current results, it was not shown on C. albicans adherence and biofilm formation after its incorporation into a denture base resin (31). Interestingly, consistent with the results, Jothiprakasam et al. in a recent study, showed that synthetized ZnO had proper antifungal activity against fluconazole-resistant strain C. tropicalis and could prevent Candida biofilm formation in medical devices (32).
Reactive oxygen spices test findings exhibited that ZnO NPs increased production of reactive O2 species by macrophages in comparison with the control group (non-tread cells). This evidence has improved the hypothesis that ZnO NPs induced antimicrobial activity mediated by macrophage, yet in a dose-dependent manner and subsequently with increasing the ZnO NPs concentration, ROS production was elevated. Parallel with the current findings, Lipovsky et al. reported that ZnO NPs in aqueous suspensions induced active oxygen species and caused an inhibition of over 95% in the growth of C. albicans. Also, they speculated that the antifungal activity of ZnO on Candida may be mediated through ROS (33, 34). Analysis of cytotoxicity effect of ZnO NPs on HepG2 cells represented limited cytotoxicity activity compared to the control group. It can be concluded that this nanoparticle may be a safe agent in clinical application, yet further in vitro and in vivo evaluation will be necessity. To the best of the author’s knowledge, this study was the first report about the effect of ZnO NPs on Hwp1 expression in C. albicans. The results suggested that the new synthetized nanoparticle may be a suitable candidate for preventing biofilm dispersion and control of Candida infection. Nevertheless, further studies are desired for support of its effect in vitro and in vivo.
5.1. Conclusions
Taken together, the current findings shed novel insight on the application of ZnO NPs in fighting against C. albicans biofilm by decreasing the Hwp1 gene expression, as the main gene in transition of blastopore to hypha concerning development of the biofilm and suggests that the traditional antifungal drug, because of undesirable side effects, ineffectiveness and limitation in number may be substituted by novel nanocomponent for proper control of Candida infection.