1. Background
Reproductive tract infections (RTIs) are a serious global health problem both directly and through their potentiating effect on HIV transmission (1). Their consequences are more prevalent among women than among men, particularly in low-income countries among women aged 15 - 49 years. An estimated 340 million new cases of RTIs, including Sexually Transmitted Infections (STIs), emerge each year (2). Women are also biologically more susceptible than men to certain chronic and disabling diseases like rheumatoid arthritis. It is a chronic, systemic inflammatory disorder of unknown etiology with an estimated global prevalence of 1% (3). It has the potential to present during the child-bearing years of women’s life. Outcomes are variable, ranging from a remitting disease (rare) to a severe disease bringing disability and even premature death (4).
Several factors, including disease process and drug therapy, allegedly predispose to infections in rheumatoid arthritis. Infectious agents, including those that can enter the host, have a major role in many etiologies of rheumatoid arthritis. Human studies have shown the association of periodontopathic bacteria with rheumatoid arthritis. Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans are the most common periodontopathic bacteria associated with rheumatoid arthritis (5, 6). Another common infection associated with rheumatoid arthritis is caused by Proteus, as Proteus mirabilis can cause urinary tract infection. Rheumatoid arthritis patients show a significantly high incidence of urinary tract infection and symptomatic/asymptomatic bacteriuria compared to non-RA people. Gastrointestinal or genitourinary infections with Salmonella, Shigella, Campylobacter, Yersinia, and Chlamydia trachomatis may cause inflammatory oligoarticular or polyarticular sterile arthritis (5). In summary, infection is a risk factor for the development of rheumatoid arthritis.
Socioeconomic constraints on study settings impose unique impediments. Both RTIs and rheumatoid arthritis are prevalent among women at the reproductive age. However, data on RTIs in rheumatoid arthritis women are woefully lacking. Although rheumatoid arthritis is predominantly female disease, there remain many unanswered (or unasked) scientific questions about reproductive health among rheumatoid arthritis women. Some studies show the improvement of rheumatoid arthritis during pregnancy. Conversely, postpartum, and miscarriage are associated with accelerated joint destruction (7, 8).
There are sparse studies on rheumatoid arthritis and sexuality that indicate the high levels of pain, physical disability, and depression interfering with sexual pleasure (9, 10). However, there is no study to assess if rheumatoid arthritis as a long life disability with an immunosuppressive nature, and many complications has any effect on the prevalence of RTIs. An understanding of the relationship between RTIs and rheumatoid arthritis can provide valuable information for policymakers and health professionals who are concerned with improving the quality of life of women, especially women with chronic disease. This research was conducted to determine the prevalence and risk factors of RTIs among reproductive-aged women suffering from rheumatoid arthritis.
2. Objectives
This study investigated the prevalence and risk factors of RTIs among reproductive-aged women with rheumatoid arthritis in Pune, India.
3. Methods
A clinical-based, cross-sectional study was performed on 400 women of reproductive age suffering from rheumatoid arthritis. The sample size of 400 subjects was calculated based on the RTI prevalence of ~40% (Government of India Family Health Survey III 2005 - 06) (11). The inclusion criteria included married women aged 15 - 49 years with a history of at least three months’ rheumatoid arthritis, referring to the Center for Rheumatic Diseases in Pune, India, from June 2013 to May 2015. They were selected by a systematic sampling method. The exclusion criteria included women who had received antibiotics or antifungal agents within the past week or and those who had vaginal douching methods and/or intercourse in the last 24 hours. Also, we excluded women who were pregnant or had vaginal bleeding or a history of delivery in the previous six weeks, as well as women with missed menstruation. In this study, vaginal speculum insertion and bimanual examination were part of data collection; thus, for cultural and ethical reasons, it was not felt appropriate to include unmarried women or girls in this research.
For a holistic approach to the issue under study, three basic tools were used for the collection of data. These tools included a previously validated questionnaire, gynecological examination, and laboratory tests to clinically and microbiologically identify RTIs. The questionnaire included sociodemographic characteristics, obstetric-gynecological and medical-surgical history, and information about their rheumatoid arthritis history, medicines, complications, and rheumatoid arthritis risk factors. Then, a gynecological examination was done by vaginal speculum insertion and bimanual exam at the time of the interview, while clinical examination privacy and confidentiality were maintained.
After speculum insertion, two specimens were obtained from the posterior vaginal fornix and cervical canal. Subsequently, two wet mounts were prepared by mixing one of the specimens with one drop of normal saline to diagnose trichomoniasis and bacterial vaginosis. The other specimen was mixed with one drop of 10% KOH to assess Candida albicans. Wet mount microscopy is the direct microscopic examination of vaginal discharge for the diagnosis of trichomoniasis, candidiasis, and bacterial vaginosis (12, 13). In this study, the diagnosis of bacterial vaginosis, candidiasis, and trichomoniasis was based on the patients’ medical history, clinical examination with the measurement of vaginal pH, whiff/KOH test, and evaluation of wet mount slides. Also, the presence of vaginal discharge and the appearance of the cervix were noted. After removing the speculum, a bimanual examination was done to evaluate the internal genital organs.
A venous blood sample was collected from each study participant for syphilis serology. All tests in this study were free of charge. The laboratory diagnosis was designed at the Laboratory of the Center for Rheumatic Diseases for the etiological diagnosis of C. albicans, bacterial vaginosis, trichomoniasis, and syphilis. Candida was diagnosed by the visualization of budding yeasts on pseudohyphae, Trichomonas by the visualization of motile Trichomonas, and bacterial vaginosis by the presence of clue cells on microscopy of the vaginal wet mount. Syphilis was screened by the rapid plasma regain test on the blood drawn from the sample population.
3.1. Statistical Analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS, V.16). Descriptive statistics (mean, standard deviation, frequency) were used to summarize the data. The frequency distribution and the measures of central tendency and variances were assessed for the relevant continuous variables. Demographic variables were examined for the relationship between the independent variable (age group) and the dependent variable (RTIs). The chi-square test (χ2) was used to analyze the categorical data. The Odds Ratio (OR) and logistic regression analysis were performed to obtain the independent determinants of RTIs. Differences were considered significant at P < 0.05.
4. Results
We enrolled 400 rheumatoid arthritis women in the age group of 15 - 49 years. Demographic data demonstrated that the majority of the respondents (46.5%) were within 30 - 49 years of age, and 11.3% were in the age group of 15 - 30 years (mean age = 39 years, range: 23 - 49 years). Besides, 96.5% were married (mean ± SD: 19.9 ± 3.3; range: 13 - 38 years), 2.8% were widowed, 0.8% were divorced, and only 2.3% of the rheumatoid arthritis women had more than one marriage. The menarche age of above 13 years was observed in 54% of the sample population (mean ± SD: 13.8 ± 1.3; range: 11 - 18 years). Among 400 rheumatoid arthritis women, 10.3% were illiterate (inability to read or write), 12.5% were educated in primary schooling, and 50.7% completed secondary schooling, and 20.3% had university education. While 29.8% of the rheumatoid arthritis women were living in rural areas, 70.3% of them were from urban areas. In this study, 83.0% of the sample population was Hindu, 12.3% Muslim, and 4.8% other religions (Jain, Sikh, Buddhist, and Zoroastrian).
Data on socioeconomic characteristics revealed that 11.5% of the sample population lived in rented houses. Since the majority of the rheumatoid arthritis women in this study were living in urban areas, the piped water, bathrooms, and toilets were available for them. Moreover, 5.3% of the rheumatoid arthritis women were using public/shared bathrooms, 6.8% public toilets (flush/pit), and 5.8% used open fields as toilets. 16.5% did not have water in their toilets. 50.3% were living in houses with 1 - 2 rooms, and 32.5% were with joint family. 87.5% of the rheumatoid arthritis women were housewives. Data on personal hygiene showed that 43.3% of the rheumatoid arthritis women did not practice washing the genital area after coitus.
While 54% of the rheumatoid arthritis women applied cloth/cotton during menstruation, 83% washed them with piped water, and among these women, 79.5% dried them in the sunshine. Only 4.8% had intercourse during the menstruation period, and 95.2% of the rheumatoid arthritis women did not have coitus during menstruation. In this study, 28.8% of rheumatoid arthritis women had pregnancy twice, 4.5% did not have any pregnancy, and 0.8% of them had experienced pregnancy seven times. The majority of rheumatoid arthritis women (48.3%) had female sterilization, and 7.5% of rheumatoid arthritis women had hysterectomy history. None of the rheumatoid arthritis patients reported the use of vaginal douche or having extramarital sex.
Clinical features of rheumatoid arthritis showed that 38% of the study subjects had early rheumatoid arthritis (≤ 2 years) and 62% late rheumatoid arthritis (> 2 years). Risk factors, including urinary tract infection and diabetes, were present in 8% and 1.5% of the subjects, respectively. The history of jaundice and tuberculosis was reported in 0.8% each. Comorbid conditions such as hypertension, hypothyroid, hyperthyroid, and kidney stone were seen in 2.0%, 2.0%, 0.5%, and 0.3%, respectively. The history of chikungunya was noted in 0.8% of the study subjects. In addition, 4.8% of the rheumatoid arthritis women had limitations in lower limbs, 4% in upper limbs, and 68.3% in both upper and lower limbs.
A global assessment of disease activity by the rheumatologist was done on a five-point scale (asymptomatic, mild, moderate, severe, and very severe). The assessment showed that 9.8% of the rheumatoid arthritis women were asymptomatic, while 55.8% had mild rheumatoid arthritis, 33% moderate, and 1.5% had severe rheumatoid arthritis. The majority of the rheumatoid arthritis women (87.8%) were on methotrexate, 46.3% steroid, 32.8% chloroquine, 22.5% sulphasalazine, 6.3% lefumide, 1.3% azathioprine, and 33.5% anti-anxiety medicines.
In this study, vaginal discharge (28.3%) was the most common symptom of RTIs, followed by itching (25.8%) and low back pain (20.5%) (Table 1). No cases of genital ulcers or genital warts were reported. During the clinical examination, no signs of abnormality in external genitalia, vaginal wall, adnexal, urethra, or Bartholin’s gland were observed.
| RTI Symptoms | Values |
|---|---|
| Vaginal discharge | 113 (28.3) |
| Itching | 103 (25.8) |
| Bad odor | 66 (16.5) |
| Severe lower abdominal pain | 58 (14.5) |
| Low back pain | 82 (20.5) |
| Vaginal yeast | 13 (3.3) |
| UTI | 26 (6.5) |
| Dyspareunia | 69 (17.9) |
| Menstrual irregularity | 24 (6.5) |
The Frequency of RTI Symptoms Among Rheumatoid Arthritis Womena
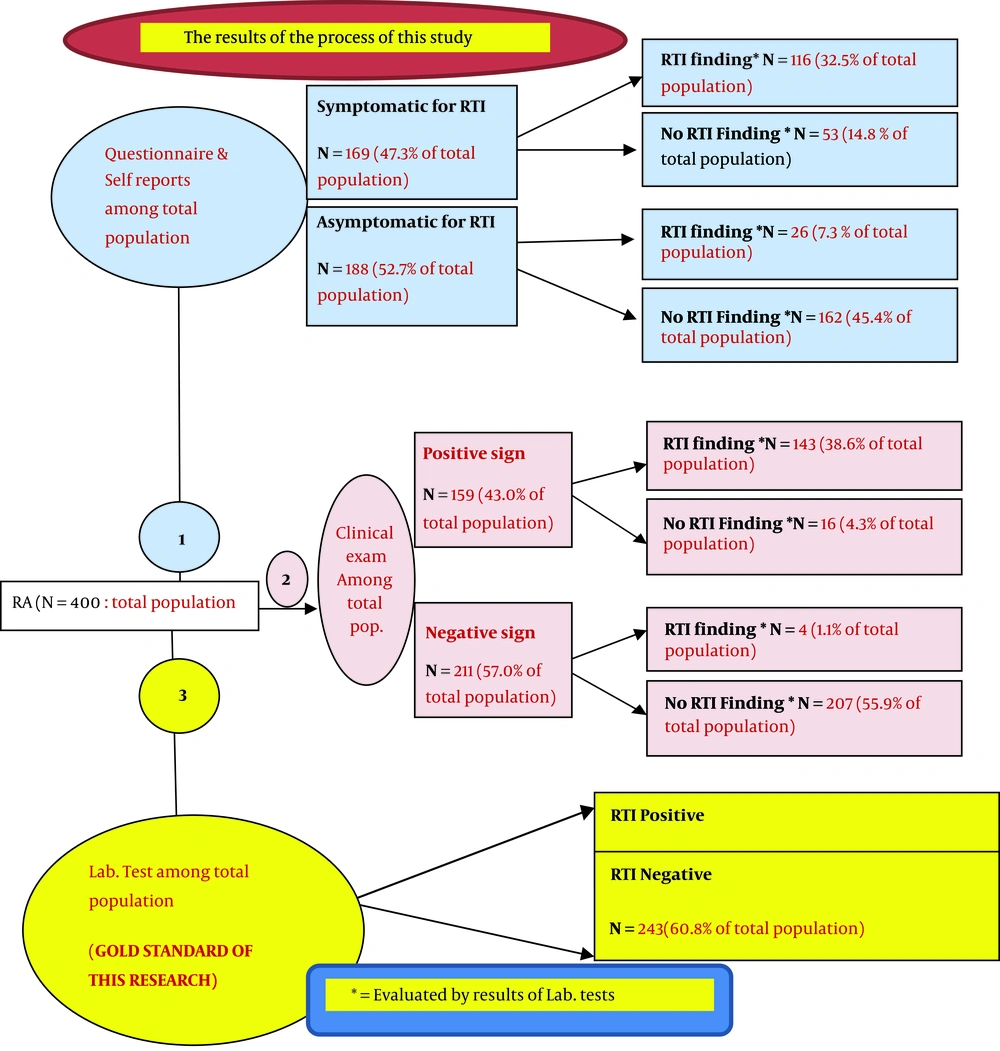
Based on the self-reported symptoms and clinical examination, 47.3% and 43% of the rheumatoid arthritis women were suffering from RTIs, respectively. Moreover, RTIs with signs and/or symptoms were observed in 39.4% of the subjects. Based on positive laboratory methods, 39.3% of the rheumatoid arthritis women had RTIs; 32% had bacterial vaginosis, 6.5% C. albicans, and only 0.8% had Trichomonas vaginalis. Besides, 7.3% of the rheumatoid arthritis women had RTIs derived from laboratory tests but did not report any symptoms (asymptomatic cases). Syphilis was not observed in the target population (Tables 2-4).
| RTIs (Laboratory-Based) | Total | ||
|---|---|---|---|
| Present (%) | Absent (%) | ||
| Symptoms of RTIs; (n = 357a) | |||
| Symptomatic RTIs; (% of total population) | 116 (68.6%); 32.5% | 53 (31.4%); 14.8% | 169; 47.3% |
| Asymptomatic RTIs; (% of total population) | 26 (13.8%); 7.3% | 162 (86.2%); 45.4% | 188; 52.7% |
| Clinical examination; (n = 370b) | |||
| Positive signs; (% of total population) | 143 (89.9%); 38.6% | 16 (10.1%); 4.3% | 159; 43.0% |
| Negative signs; (% of total population) | 4 (1.9%); 1.1% | 207 (98.1%); 55.9% | 211; 57.0% |
| Symptoms and/or signs for RTIs (n = 371c) | |||
| Present; (% of total population) | 146 (69.2%); 39.4% | 65 (30.8%); 17.5% | 211; 56.9% |
| Absent; (% of total population) | 2 (1.3%); 0.5% | 158 (98.7%); 42.6% | 160; 43.1% |
Frequency of Symptomatic and Asymptomatic RTIs Among Rheumatoid Arthritis Women
According to our results, several independent risk factors were identified for RTIs including age under 30 years, living in one-room houses, using public toilets, intercourse during menstruation, no washing-up of the genital area after intercourse, using unsanitary napkin for menstruation, and taking chloroquine for rheumatoid arthritis. Adjusting for confounding factors in logistic regression showed that only four factors remained significant, including age under 30 years (AOR: 2.4, 95% CI: 1.2 - 4.9), small residence (AOR: 2.5, 95% CI: 1.2 - 5.1), improper linen for menstruation bleeding (AOR: 1.9, 95% CI: 1.1 - 3.3), and oral disease-modifying anti-rheumatic drugs (AOR: 3.96, 95% CI: 1.9 - 7.9) (Table 5). Figure 1 shows the process of the study and the results.
| Parameters | Adjusted Odds Ratio (95% CI) | P Valuea |
|---|---|---|
| Age group, y | ||
| < 30 | 2.4 (1.2, 4.9) | 0.018 |
| 30 - 40 | 1.5 (0.9, 2.4) | 0.082 |
| +40 | 1.0 | - |
| Number of rooms | ||
| 1 room | 2.5 (1.2, 5.1) | 0.015 |
| 2 rooms | 1.9 (1.1, 3.6) | 0.034 |
| 3 rooms | 1.3 (0.7, 2.5) | 0.349 |
| > 3 rooms | 1.0 | - |
| Type of tampon used in menses | ||
| Sanitary napkin | 1.0 | - |
| Cloth | 1.9 (1.1, 3.3) | 0.015 |
| Chloroquine treatment | 3.96 (1.9, 7.9) | 0.0001 |
| Limited moderate activities in QOL questionnaire | 1.4 (1.1 - 2.6) | 0.010 |
Logistic Regression Analysis
5. Discussion
Reproductive tract infections are a silent worldwide pandemic in women of the age group of 15 - 49 years. Finding the prevalence rates of RTIs among different groups of women, especially women with chronic diseases, can be a vital indicator of reproductive health among them. Rheumatoid arthritis is a long life disability that is more prevalent among women. To our knowledge, there have been no studies on the prevalence of RTIs among rheumatoid arthritis women. We aimed to find the prevalence of RTIs among rheumatoid arthritis women in Pune City, India. The results of our study can be discussed as follow. The total sample size was 400 married rheumatoid arthritis women aged 15 - 49 years. The majority of the sample population was in the age group of 41 - 49 years. The COPCORD Bhigwan (Pune, India) data revealed a surprisingly high prevalence of rheumatoid arthritis in young women, which has not been reported in other population-based studies from the rest of the world. The prevalence of rheumatoid arthritis per 100,000 population was 1,639 among women aged 30 - 44 years and 1,775 among women aged 45 - 59 years in Bhigwa (14, 15).
In this study, 54% of rheumatoid arthritis women had a menarche age above 13 years. According to a study of the menarche age among Indian (Maharashtraian) girls, 63.30% had a menarche age of 12 - 13 years and 11.74% above 14 years (16). Rheumatoid arthritis is associated with delayed menarche age (17); our study is in agreement with this result. The statistics regarding the magnitude of RTIs are different because of the varying source of information, methodologies, and technologies of measurement. In this study, for a holistic approach to this problem, three basic tools were used for data collection: self-reported symptoms, clinical examination, and laboratory methods. Based on the laboratory methods, 39.3% of the sample population had RTIs, while 39.4% of the subjects had RTI based on signs and/or symptoms (Table 2). The similarity of the figures (39.4% vs. 39.3%) shows that where a facility for laboratory investigations may not be available, diagnosing RTIs with signs and/or symptoms is as good as diagnosing RTIs with laboratory investigations. No previous studies reported about RTIs among rheumatoid arthritis women, so we could not compare the results of this study with other studies on the prevalence of RTIs.
The knowledge of RTIs is poor among rheumatoid arthritis women. In this study, most rheumatoid arthritis women with RTIs were under 30 years. This is in line with other findings showing than young married women had high risks of RTIs (16, 18, 19). Besides, 46.8% of rheumatoid arthritis women with RTIs were living in houses with 1 - 2 rooms. It shows that low socioeconomic status (poor housing) can affect women’s health status. The high incidence of RTIs in this group of women can be because the limited number of rooms can deprive a privacy environment for partners, and subsequently, they cannot do hygienic practices regarding intercourse. In our study, the association between the occupation of rheumatoid arthritis women and RTIs was seen to be not significant. A cross-sectional, community-based study of RTIs in 1996 - 97 among married women aged 16 - 22 years in a rural community of Tamil-Nadu, India, revealed that women who worked as agricultural laborers had more likelihood of having STIs than those who worked solely at home (20).
In the current study, using public toilets and no washing-up of the genital area after intercourse were the risk factors of RTIs. In line with our findings, two studies from Malawi and Nigeria showed that the lack of proper toilet is one of the significant factors in contracting RTIs (21, 22). Lack of adequate sanitation in toilets could potentially facilitate infection transmission through genital fluids. This transmission can occur by sharing bath towels and toilet seats (22). The absence of water for genital area washing after toilet use or intercourse is also associated with urinary tract infection and genital infection. The presence of piped water provides a better situation and access to water for washing the genital area after coitus or urination.
According to our results, 54% of the rheumatoid arthritis women did not use commercially available sanitary materials during menstruation. This finding is in line with a study conducted in Shimla city in 2006 (23), which showed that unhygienic practices during menstruation such as using improper and unsanitary material to absorb menstrual blood can be associated with a high prevalence of RTIs. It can be justified that the open neck of the uterus (cervix) creates a pathway to allow blood to pass out of the body and bacteria to travel back into the uterus and pelvic cavity. In addition, the pH of the vagina is less acidic at this time, which makes yeast infections such as thrush (candidiasis) occur more likely (24). Thus, using sanitary pads during menstruation can decrease the frequency of RTIs. The majority of the rheumatoid arthritis women who did not wash the genital area after vaginal sexual intercourse had RTIs. Also, RTIs were more prevalent among rheumatoid arthritis women who had a history of intercourse during the menstrual bleeding period. In line with our results, a study from China in 2003 (25) showed the importance of reproductive health behaviors for the prevention of RTIs, which included washing practices before and after sexual intercourse, taking a shower daily, and washing the genital area during menstruation.
In the present study, the majority of the rheumatoid arthritis women with RTIs were on chloroquine. The high prevalence of RTIs among chloroquine users may be justified according to one article in the monthly index of medical specialties that stated chloroquine in considerable amounts is deposited in tissues like the liver, spleen, kidney, and lung (26). By deposition in the genital tissue, it may cause some problems, including RTIs. Randomized controlled trials are certainly needed to prove this hypothesis. Chloroquine has also an affinity for melanin and it gets concentrated in pigmented structures, which may explain its toxic effects on the eyes (keratopathy and retinopathy) and the skin when used over a prolonged period for treating rheumatoid arthritis and other connective tissue disorders (27). Another study demonstrated palate hyperpigmentation caused by the prolonged use of chloroquine due to the deposition of drug metabolites in the mucosa (28). Also, a study found that chloroquine enhances viral replication in mice (29, 30). It may suggest a possible connection between the increased spread of AIDS in malaria-endemic areas and the wide use of chloroquine in those areas for the chemotherapy of malaria.
As reported by Davidson et al. (31), overuse of chloroquine can lead to the development of a specific strain of Escherichia coli that is now resistant to the powerful antibiotic ciprofloxacin. Escherichia coli, which lives normally in the rectum, can be transferred to the vaginal wall to cause bacterial vaginosis. Bacterial vaginosis was the most prevalent RTIs in this study. There are no studies on the side effects of chloroquine leading to RTIs (32). Chloroquine diffuses rapidly across the cell membranes to acidic cytoplasmic vesicles like endosomes, lysosomes, or Golgi vesicles and increase their pH (33).
The deposition of chloroquine metabolites in the vaginal mucosa probably leads to changes in vaginal pH (33). Another possibility is the relationship of chloroquine with the development of a specific strain of E. coli that can be responsible for the elevated bacterial vaginosis among the sample population. No previous studies have reported the risk factors of RTIs among rheumatoid arthritis women. This study was cross-sectional, so the researchers could infer any causal association between RTIs and rheumatoid arthritis. Indeed, the main limitation of this study is that causality cannot be inferred. Despite the above limitation, it should be noted that the current clinical-based cross-sectional study is the first study on this issue. Although rheumatoid arthritis is known with a high risk of infection (34), none of the previous studies have been conducted on the possible effects of rheumatoid arthritis on the infection of the reproductive tract.
5.1. Conclusions
Rheumatoid arthritis patients experience poorer life expectancy than general healthy people. The risks of infections, cardiovascular disease, and other comorbid conditions are also high. The results of this study showed that almost two-fifth of young rheumatoid arthritis women suffered from RTIs. This study can be a beginning for research among rheumatoid arthritis women to find whether RTIs can be a comorbid disease with rheumatoid arthritis. In this study, taking chloroquine was introduced as one of the risk factors for RTIs among rheumatoid arthritis women. More longitudinal, comparative, or interventional studies in different settings among rheumatoid arthritis women are needed to determine whether rheumatoid arthritis can cause RTIs among women due to taking chloroquine.