1. Background
Migraine is one of the most common hereditary disease. The way to prevent and control of migraine attacks is always demanded by patients with recurrent migraine attacks. Some of the most important prophylactic drugs for migraine relief include tricyclic antidepressants, beta-blockers, and anticonvulsants (1). Studies reported a high prevalence of migraine together with extrapyramidal signs such as restless legs syndrome (RLS) (2). RLS leads to unpleasant feelings or paresthesia in the legs, occurring usually at night and during the early stages of sleep. RLS symptoms are quickly relieved by moving the legs (3). According to the results of the study by Fernandez, patients with RLS had higher lifetime prevalence of migraine than non-RLS controls (53.2% vs. 25.5%) (4). The reason for this concurrence is not explained clearly using a single mechanism. Some studies attributed this concurrence to impaired dopamine synthesis in both diseases (5). Other studies also proposed the hypothesis of impaired central metabolism of iron in both diseases (2). Simultaneous manifestation and treatment of both diseases with a common drug is of great importance. This is due to the fact that insomnia caused by RLS can increase the risk of migraine attacks and treatment of common mood disorders associated with migraine may, on the other hand, exacerbate RLS symptoms (6).
2. Objectives
The present study aimed at investigating the effect of pramipexole (a dopamine agonist effective in RLS) on the frequency and severity of migraine attacks and disability of patients who simultaneously have migraine and RLS in the activities of daily living.
3. Methods
The present randomized, double-blind study protocol was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (ethical code: 1394.391). The participants of the study included 30 patients with migraine with three or more attacks per month referred to Golestan Hospital, Ahvaz, Khuzestan Province, Iran from May 2015 to September 2016. The migraine was diagnosed in the subjects based on their detailed history and use of the International Headache Society (IHS) criteria (7). The patients were then questioned about their RLS symptoms by a neurologist. The diagnosis of RLS was based on the following criteria, established by the International Restless Legs Syndrome Study Group (IRLSSG):
A strong urge to move your legs, usually accompanied by uncomfortable sensations typically described as crawling, creeping, cramping, tingling or pulling.
Symptoms begin or become worse when resting or inactive, such as when lying down or sitting.
Symptom get better when move, such when walk or stretch, at least as long as the activity continues.
Symptoms are not solely accounted for by another condition such as leg cramp, leg swelling or arthritis (8).
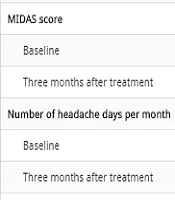
The patients were also examined for secondary causes of RLS such as uremia and iron deficiency anemia. They were included in the study if the secondary causes of RLS were rejected. In the current study, due to taking propranolol, the patients with heart diseases such as heart block and bradycardia were not included in the study. The participants of the study were randomly divided into two groups using the four block method. Both groups received propranolol (20 mg) twice a day. The case group received pramipexole 0.18 mg and the control group received placebo one hour before sleep for three months. The MIDAS and IRLSSG questionnaires were filled out for patients before and three months after the treatment. The migraine disability assessment score (MIDAS) questionnaire (supplementary file Appendix 1) is quite a useful tool in clinical trials. There were five questions that asked patients regarding their disability associated with migraine headache during the last three months. The MIDAS scores interpretation reflects the degree of disability in patients; the scores 0 - 5 (days) show little or no disability, 6 - 10 indicate mild disability, 11 - 20 moderate disability, and ≥ 21, severe disability. Furthermore, there are two questions that indicate the number of headache days and headache intensity during the last three months. The patients scored their headache’s severity from 0 to 10 where score 10 showed the maximum intensity headache (9). Moreover, patients were questioned about the side effects of drugs such as orthostatic hypotension and bradycardia at each visit, and they were excluded from the study if any side effects were observed. The data were expressed as mean ± standard deviation. For each group, changes in the MIDAS score, frequency, and intensity of headache were compared by paired-samples t-test between the beginning and the end of the study.
4. Results
Table 1 shows the information of the study population. One patient from the case group and two patients from the control group were excluded from the study due to lost to follow-up. No significant difference was observed between the two groups in MIDAS score and frequency and severity of migraine at baseline. After three months of treatment, the mean MIDAS score in case group reduced from 41.27 to 19.533 and in the control group reduced from 42.733 to 27.46 (52.67% vs. 35.74%). Compared to the placebo group, the changes in the MIDAS score, in the case group was significant, at the end of the study (P = 0.001) (Table 2). After three months of intervention, the mean frequency of migraine attacks in the case group reduced from 7.266 to 2.733 and in control group reduced from 6.87 to 4.13 per month, respectively (62.38% vs. 39.85%). Compared with the placebo group, this reduction was significant in the case group (P = 0.001). Although severity of migraine reduced in both groups after the treatment, this reduction was not significant in the control group, compared with that of the case group (52.13% vs. 47.56%).
| Variable | Treatment Group | Control Group | P Value |
|---|---|---|---|
| Age, y | 0.50 | ||
| Mean ± SD | 29.21 ± 4.36 | 30.06 ± 2.26 | |
| Range | 15 - 50 | 15 - 50 | |
| Gender | 0.456 | ||
| Male | 6 | 4 | |
| Female | 9 | 11 |
| Variable | Treatment Group | Control Group | P Value |
|---|---|---|---|
| MIDAS score | |||
| Baseline | 41.27 | 42.733 | 0.094 |
| Three months after treatment | 19.533 | 27.46 | 0.001 |
| Number of headache days per month | |||
| Baseline | 7.266 | 6.87 | 0.558 |
| Three months after treatment | 2.733 | 4.13 | 0.001 |
| Headache severity | |||
| Baseline | 7.1333 | 7.5333 | 0.295 |
| Three months after treatment | 4.23 | 4.6667 | 0.095 |
aValues are expressed as mean ± SD.
5. Discussion
The results obtained from the current study showed that compared with the control group, the MIDAS score and frequency of migraine attacks reduced in the case group. In a previous clinical trial, the effect of pramipexole (0.7 - 0.18 mg) on 10 patients with migraine and RLS was investigated. Frequency and severity of migraine attacks significantly improved in 50% of the patients, of whom 80% also had morning headaches before treatment (10). These findings were consistent with those of the present study in terms of reduced frequency of migraine attacks. Recently, concurrence of migraine and RLS is frequently reported. The reason for this relationship is not explained thus far directly using a single mechanism. Pramipexole (a dopamine agonist) reduces the frequency and severity of migraine attacks and disability of patients with migraine in the activities of daily living, which suggests impairment in dopamine synthesis among such patients. Functional magnetic resonance imaging (MRI) findings, which shows the role of basal ganglia in pain processing in patients with migraine, support this hypothesis (2). Insomnia is a known trigger for migraine. On the other hand, studies show that treatments for RLS such as pramipexole relive symptoms of RLS by improving sleep (11). With this mechanism, pramipexole can play a significant role in reducing the frequency and severity of migraine attacks, especially morning migraines. According to the results of the present study, pramipexole may be effective in reducing migraine attacks and disability of patients with migraine in the activities of daily living.
5.1. Limitations of the Study
Since patients with migraine with more than three attacks per month should receive prophylactic treatment, lack of using antimigraine drugs and relying on placebo or pramipexole, which their effects on migraine attacks are not proved yet, was attributed to the ethical considerations. Therefore, both groups in the current study received propranolol as a standard treatment for migraine. Because of the small sample size, these findings need to be confirmed in a large-scale randomized, controlled trial.