1. Background
Adolescence is a developmental life stage and a transition period from childhood to adulthood, which is associated with various physical, cognitive, socio-emotional, and environmental changes (1). Adolescence is characterized by increased thinking ability, start of puberty, changes in interactions with the family, friends, and the community, striving to acquire new emotional and social patterns, and creating new directions for the future as independent and productive adults (2). These factors affect the decision-making of adolescents regarding education, employment, and wellbeing, especially in the individual and social spheres (3).
Obesity is a global health issue, which has become an epidemic with the potential to affect all age groups (4). According to statistics, 170 million children aged less than 18 years had obesity in 2008, and it is predicted that this number will reach 30% of all children across the world by 2030 (5). Furthermore, statistical data are suggestive of the high prevalence of obesity and overweightness among Iranian children and adolescents. For instance, the study by Kelishadi et al. (6) on 13,486 students aged 6 - 18 years in 30 provinces of Iran indicated the prevalence of obesity and overweightness in Iranian children and adolescents to 9.7% and 11.9%, respectively, which was relatively higher compared to the previous finding. Considering the high probability of weight gain in adolescence, this period is an essential predictive of overweightness in adulthood (7) and substantially affects the daily activity and other dimensions of life in adolescents (8). Consequently, obesity in children and adolescents has become a global issue (9).
Several studies have been focused on the underlying and biological factors of obesity, while data is scarce regarding the psychological factors and consequences, particularly in children and adolescents. This is mainly because weight gain is considered to be a normal change in children and could be resolved with increased height. However, some cases not only have showed no signs of improvement, but they have also experienced unfavorable psychological and social effects on their future life (10, 11).
Depression is a psychological consequence of obesity, which has attracted the attention of researchers in terms of the biological mechanisms and new therapeutic interventions (12). Depression is associated with the lack of energy and disinterest in life, sense of guilt, difficulty concentrating, low appetite, suicidal thoughts, decreased activity, impaired cognitive abilities, sleep disorders, and other biological complications (13). Although several studies have examined the correlation between depression and obesity, it remains unclear whether depression leads to obesity or vice versa (14). Evidence suggests that obesity is a comorbidity of depression, and the prevalence of depression is higher in overweight individuals (15). Furthermore, it is suggested that obese individuals gradually become depressed due to their negative body image, low quality of life, and other physical consequences (16, 17). In this regard, Brewis and Han (18) proposed some logical findings, arguing that obesity and its concerns influence depressive symptoms in individuals.
Self-esteem has been shown to have a negative correlation with obesity (19). Due to the negative valuation of the society regarding obesity, obese individuals tend to suffer from low self-esteem (20). The adverse effects of obesity in adolescence potentially lead to long-term consequences until adulthood (19). Low self-esteem is also associated with behavioral disorders, cynical and depressive moods, and negative and uncontrollable emotions (21).
In a study by Coco et al., interpersonal problems were associated with overeating and low self-esteem in obese individuals. Moreover, Dunkleany and Grilo (22) investigated 236 obese patients, discovering that low self-esteem and depressive symptoms were elaborated with obsessive body image evaluation, body weight, and other anxiety disorders. According to some studies, improved body image, self-esteem, and depression have been achieved in the obese individuals receiving psychotherapy (3).
Psychological wellbeing is another psychological variable associated with weight gain. Wellbeing or life satisfaction is considered to be one of the primary psychological qualities of a healthy individual (23). Psychological wellbeing could be defined as feeling healthy, living in a productive environment, being valuable, and enjoying life (24). According to Vallis (25), there is a complex association between obesity and psychological wellbeing, which encompasses physical, social, and psychological factors. This is considered to be a reciprocal correlation as obesity could lower the quality of life and increase the risk of mental and emotional disorders. On the other hand, the patients with treated obesity as a health issue or those attempting treatment by medications or food as a counter measurement solution may gain weight. Many obese individuals experience self-blame, low self-esteem, and a negative attitude toward themselves and their circumstances throughout life (25). In this regard, Anderson et al. assessed the health-related quality of life and psychological wellbeing of children and adolescents with obesity, reporting low levels of psychological wellbeing and emphasizing on the necessity of psychotherapeutic interventions for the improvement of their psychological wellbeing (26).
As mentioned earlier, several studies evaluate various aspects of obesity each year across the world, aiming to obtain beneficial results for the prevention and treatment of weight gain, particularly in childhood and adolescence. Nevertheless, there are inadequate psychological studies regarding the impact of obesity on the psychological and social consequences of weight gain in adulthood. Therefore, the recognition of the psychological factors of this phenomenon could help reduce the adverse psychological consequences of obesity in children and adolescents.
The current research had two main objectives. Many studies have been focused on the causes of obesity, while only a few have investigated the psychological variables associated with phenomenon. The secondary objective of the study was the evaluation of obese adolescent girls and their comparison with their normal peers.
2. Objectives
The present study aimed to assess the psychological consequences of obesity in adolescent girls.
3. Methods
This descriptive study was performed using the causal-comparative method on a sample population consisting of 150 female students in the first and second year of high schools in Shahrekord (district 1), Iran in 2019. In total, 360 students (each cluster with 180 subjects) were selected using the Cochran formula (
The questionnaires for the normal students were completed after each high school provided the researcher with the names of 10 selected classes, excluded the obese students from sampling, and prepared the final list of 10 classes. Following that, 18 individuals were randomly selected from each list, and after coordination with the principal and teacher, the names of the students were read out in each class. The selected students were informed of the research objectives, completion of the questionnaires, and confidentiality of their information. Upon their consent, the questionnaires were provided to the participants. After examining the questionnaires, the researchers eliminated seven participants who did not reply to most of the questions and conducted the data assessment of the normal group (173 subjects).
The obese students were selected via purposive sampling. To this end, the researchers prepared a list of the individuals with obesity based on their healthcare records and body mass index (BMI) from five random high schools. The questionnaires of the obese students were implemented individually, and the necessary explanations were provided on the ethical principles, objectives of the study, data confidentiality, and freedom to withdraw from the assessment. After obtaining the informed consent of these subjects for participation, they were asked to complete the questionnaires. In total, 180 obese students participated in the study. Notably, the researchers excluded four of these participants who did not reply to most of the questions, and three other individuals were also excluded to maintain equality between the two sample groups; finally, the data assessment of the obese group was performed with 173 subjects.
The inclusion criteria of the study were as follows: (1) female gender; (2) willingness to participate; (3) BMI of 85 - 95 percentiles for obesity and weight gain of more than 95 percentile; (4) age range of 12 - 16 years; and (5) absence of significant physical problems (e.g., blindness). The exclusion criteria were incomplete research questionnaires and pre-existing medical conditions (e.g., cardiovascular diseases, asthma).
The mean BMI of the obese students was 26.88 kg/m2, which was converted into the percentile of obesity and weight gain.
3.1. The Center for Epidemiological Studies Depression Scale for Children
This scale was formulated by Weissman et al. in 1980 for the screening of depressive symptoms and assessment of symptom improvement in children and adolescents aged 6 - 17 years. All the 20 items of the Center for Epidemiological Studies Depression Scale for Children (CES-DC) are rated based on a four-point scale (zero = not at all, 3 = a lot). To control the response bias, four items (items 4, 8, 12, and 18) are scored in a reversed manner and summed up, and the youths who obtain the scores of ≥ 15 are speculated to have significant depressive symptoms.
The results of the validity assessment of the CES-DC have indicated a significant correlation with the Beck depression inventory (BDI). In the study by Barkmann et al. (27), the internal consistency of the CES-DC was evaluated using the Cronbach’s alpha and estimated at 0.71 - 00.91. In Iran, the validity and reliability of the CES-DC have been estimated by Ebadi and Habibpour in adolescents aged 11 - 17 years, and the obtained results indicated a significant correlation with the BDI of 0.73 and Cronbach’s alpha of 0.82, confirming the validity and reliability of the CES-DC for the Iranian population. In the present study, the Cronbach’s alpha of the scale was calculated to be 0.76.
3.2. The Rosenberg Self-Esteem Scale (RSES)
This scale was developed by the sociologist Morris Rosenberg in 1956 and consists of 10 items that positively express the overall feelings of self-acceptance. Each item is assigned with a score within the range of 1 - 4 (strongly disagree = 1, strongly agree = 4). The total score is determined by summing up the scores of the questionnaire items, with the minimum and maximum score of 10 and 40, respectively and the higher scores signifying better self-esteem. The Cronbach’s alpha coefficients of the RSES have been reported to be within the range of 0.72 - 0.88 in the previous studies (28). In Iran, the study by Rajabi and Bohlol (29) estimated the Cronbach’s alpha coefficient of 0.84-0.90 for the freshmen students of Shahid Chamran University. In the present study, the Cronbach’s alpha of the scale was estimated at 0.86.
3.3. Ryff’s Psychological Wellbeing Scales
This 18-item scale was designed by Ryff in 1989 and measures six factors of wellbeing, including autonomy, environmental mastery, personal growth, life purpose, positive relations with others, and self-acceptance. Each statement is scored within the range of 1 - 6, with score one indicating strong disagreement and score six indicating strong agreement. The total score of Ryff’s Psychological Wellbeing scales (PWB) is obtained by summing up the score of the six factors of the test. Notably, 10 items of this scale are scored directly, and eight items are scored in a reverse manner, with the higher scores indicating better psychological wellbeing.
Ryff and Keyes (30) reported the Cronbach’s alpha of 0.86 - 0.93 for the six factors. In Iran, the study by Khanjani et al. (31) evaluated the PWB in standardized undergraduate students and estimated the Cronbach’s alpha coefficient of 0.71 for the total sample population. In the present study, the Cronbach’s alpha of the scale was estimated at 0.75.
The study protocol was approved by the Ethics Committee of Shahrekord University of Medical Sciences (code: IR.SKU.REC.1398.006).
4. Results
4.1. Demographic Characteristics
Approximately 46.8% of the overweight participants were within the age range of 12 - 14 years, and 53.2% were aged 16 - 15 years. The parental education level of the students ranged from illiteracy to postgraduate studies. Paternal occupation status covered the range of unemployed, employee, and self-employed with the percentile of 3.5, 38.7, and 57.8, respectively. In the normal group, 57.2% of the participants were within the age range of 12 - 14 years, and 42.8% were aged 15 - 16 years. The parental education level ranged from illiteracy to doctorate studies. Paternal occupation status covered the range of unemployed, employee, and self-employed with the percentile of 1.8, 33, and 65.2, respectively.
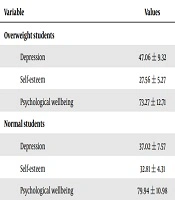
According to the information in Table 1, the normal group scored higher in terms of self-esteem and psychological wellbeing, while the overweight group had higher scores of depression.
| Variable | Values |
|---|---|
| Overweight students | |
| Depression | 47.06 ± 9.32 |
| Self-esteem | 27.56 ± 5.27 |
| Psychological wellbeing | 73.27 ± 12.71 |
| Normal students | |
| Depression | 37.02 ± 7.57 |
| Self-esteem | 32.81 ± 4.31 |
| Psychological wellbeing | 79.94 ± 10.98 |
aValues are expressed as mean ± SD.
The equality of the distribution was ensured using the Kolmogorov-Smirnov test. The null hypothesis indicated the normal distribution of the scores of all the research variables in both groups, which was confirmed. Furthermore, the Levene’s test was used for the equivalence of the variances (P > 0.05), and the use of parametric tests was also possible. The analysis of covariance (ANCOVA) was applied for data analysis since the researchers aimed to control the role of the demographic variables in parental education.
According to the information in Table 2, the F value of 59.775 and Wilks' lambda of 0.344 at the P value of less than 0.000 were statistically significant. Therefore, the grouping impact factor was of importance, and it could be concluded that there was a significant difference between the normal and obese female students in at least one of the test variables.
| Effect | Test | Value | F | df Hypothesis | df Error | Sig. |
|---|---|---|---|---|---|---|
| Grouping | Wilks’ lambda | 0.344 | 59.775 | 3.000 | 342.000 | 0.000 |
| Lawley-Hotelling test | 0.656 | 59.775 | 3.000 | 342.000 | 0.000 | |
| Largest root | 0.524 | 59.775 | 3.000 | 342.000 | 0.000 | |
| Roy’s criterion | 0.524 | 59.775 | 3.000 | 342.000 | 0.000 |
Before performing the ANCOVA, we had to ensure that there was no interactions between the independent variable and the covariate (parental education level) with the variables of depression, self-esteem, and psychological wellbeing using the regression slope.
According to the information in Table 3, no significant difference was observed between the levels of the dependent variables, and the ANCOVA was carried out using the parallel slope regression model.
| Sources of Change | Dependent Variables | Type III Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|---|
| Parental Education Level | Depression | 19.032 | 1 | 19.032 | 0.264 | 0.608 |
| Self-esteem | 70.308 | 1 | 70.308 | 3.085 | 0.080 | |
| Psychological wellbeing | 195.443 | 1 | 195.443 | 1.382 | 0.241 |
According to the information in Table 4, the F value of the variables of depression, self-esteem, and psychological wellbeing was equal to 122.200, 104.955, and 27.362, respectively, which were considered significant at 0.000. As a result, significant differences were observed in the variables of depression, self-esteem, and psychological wellbeing between the normal and obese students.
| Sources of Change | Dependent Variables | Type III Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|---|
| Parental Education Level | Depression | 8780.170 | 1 | 8780.170 | 122.200 | 0.000 |
| Self-esteem | 2406.485 | 1 | 2406.485 | 104.955 | 0.000 | |
| Psychological Wellbeing | 48571.621 | 1 | 48571.621 | 27.362 | 0.000 |
5. Discussion
The current research aimed to examine the psychological consequences of obesity in adolescent girls, and the results demonstrated the higher score of depression and lower scores of self-esteem and psychological wellbeing in the obese group, showing a significant difference in this regard.
According to the present study, depression was more prevalent in the obese adolescents compared to the normal individuals, and the difference in this regard was considered significant. This is consistent with the results of three previous studies (15, 17, 18), which indicated a strong association between obese individuals and depressive disorders (32). The study by Moshirian Farahi et al. (33) showed positive, significant correlations between BMI, depression, and age in 390 individuals referring to the health center in Norabad Delfan City (Iran). In another research, Anderson et al. (34) examined the association of depression and anxiety disorders with weight changes in a prospective community-based study of the children who were followed-up into adulthood, and the obtained results indicated the higher prevalence of depression in the overweight group compared to the control group. In addition, the research by Dixon et al. confirmed the high probability of depression in female adolescents with obesity, which is consistent with the results of the present study considering the significant difference in depression between the two groups (32). Therefore, it could be concluded that young girls are highly concerned and sensitive about their body image. The growing popularity of social media networks and their imposing standards of ideal body image (e.g., thin body figures) lead to dissatisfaction and negativity in overweight adolescents (35). The adolescent regards obesity as a social disgrace and gradually isolates themselves from most social activities, which in turn lowers their self-esteem and make them more susceptible to depression. This leads to the adaptation of inappropriate behaviors and lifestyles, reduced physical activity, and development of inappropriate eating habits, which is plays a key role in depression. Furthermore, overweight adolescents are subject to bullying, harassment, and derision by their peers, which also increase the risk of depression (10).
According to the findings of the current research, the overweight group had lower self-esteem scores compared to the normal group, which is consistent with the results of the previous studies in this regard (19, 20, 22, 36). Low self-esteem is a significant factor in obesity as reflected in the results of several studies denoting the correlation of low self-esteem and adverse consequences such as behavioral disorders, negative/depressive moods, and other emotional issues. Compared to normal individuals, overweight individuals are more displeased with themselves, mentally occupied, and likely to avoid social interactions. Consequently, their self-esteem is lower than normal individuals.
Individuals suffering from obesity may have been the subject of derision from their peers, friends, and classmates and also continuously blamed for their eating habits by their parents. A failed weight loss diet plan is often followed by feelings of worthlessness and low self-esteem, as well as the development of a negative body image. In a study by Harter and Whitesell (21), the adverse consequences of low self-esteem were reported to be depression, anxiety, negative moods, and other emotional issues. Obese adolescents are prone to various mental disorders, including depression (21). The current research also indicated the higher level of depression and lower self-esteem in the obese individuals compared to the normal group. The results of another study indicated that interpersonal problems were associated with overeating and low self-esteem in the overweight group (6). In a cross-sectional study performed by Xue-Yan et al. (37), it was suggested that obese female adolescents had low self-esteem, while the individuals with severe obesity were at the higher risk of low self-esteem (37).
With this background, the two variables of depression and low self-esteem in obese individuals must be further considered as any negligence causes a negative impact on their lives, annihilating their motivation to start something or finish what they have already started. While ordinary students do homework at school, participate in social, cultural, and sports activities, and provide a daily report of their work, overweight students do not attend school activities and are often rejected by their classmates, have lower self-esteem, and gradually become isolated and depressed. The majority of these cases consider obesity as the cause of their exclusion. Teenage girls usually seek the attention of others, and being rejected and ridiculed by their peers gradually leads to the loss of their self-esteem and self-confidence and avoidance of social presence. They may even be forced to abandon their work, adhere to a diet, and continuously blame themselves. Consequently, obesity plays a key role in their lives and may even lead to other issue due to low self-esteem, such as depression, anxiety, and suicide.
The results of the present study suggested the significantly lower score of psychological wellbeing in the overweight students compared to the normal students. Therefore, it could be concluded that obesity is a severe issue with severe outcomes in terms of physical health, mental wellbeing, and quality of life (38). It has suggested that obesity may cause adverse consequences when it comes to mental wellbeing, manifesting in the form of depressive symptoms, anxiety, low quality of life, and damaged physical and interpersonal relationships (39). In this regard, Anderson et al. asserted that due to the low psychological wellbeing in overweight adolescents, psychotherapeutic interventions are required to improve this aspect of their life.
Overweight students may be criticized by their family for their eating habits and are forced to follow different diets, humiliated by their friends and peers and unable to participate in games and sports. They have insufficient social interactions, a negative body image, and low self-esteem and tend to experience depression and anxiety, which in turn lead to inferior psychological wellbeing and low quality of life. It has been confirmed that overweight adolescents are less likely to marry or have a well-paid job and tend to become the subject of social stigma and mockery, which jeopardize their mental wellbeing in the long run.
In general, the increased prevalence of obesity is associated with numerous negative psychological and social consequences in adolescent girls who will take on different roles in the future, such as motherhood and the upbringing of future generations. Therefore, emphasis should be placed on the consequences of weight gain in order to improve the quality of life of these individuals in the community. The findings of the current research could be used by the psychologists, psychiatrists, nutritionists, and general practitioners who focus on depression, self-esteem, and psychological wellbeing for the development of preventive and treatment interventions. Our findings could also inform educational officials to devise weight gain support programs for adolescent girls as a preventive measure against adverse psychological consequences.
One of the limitations of the current research was the restriction of the sample population to the female students of Shahrekord in Chaharmahal and Bakhtiari Province, and the generalization of the results should be with caution. Another limitation was the exclusiveness of the study to female students, and it remains unclear whether the results will be identical in overweight and normal male students or in comparison with other female group.
Since overweight individuals are at the risk of several psychological consequences, it is recommended that further investigations be performed regarding other psychological variables in both male and female overweight and normal adolescents simultaneously, which could benefit universal healthcare policies.