Dear Editor,
A highly contagious coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1). Since the first patient was hospitalized in Wuhan, Hubei, China, on December 12th, 2019 (1), more than 5 million cases and 300,000 deaths have been recorded worldwide up to May 18th, 2020 (2). The virus affects the respiratory system of the person, and the patient has the symptoms of fever, cough, fatigue commonly, and having pneumonia with abnormal findings on chest CT (3). Sometimes, sputum discharge, dyspnea, headache, hemoptysis, and in some cases, diarrhea have been reported (3). The first officially confirmed case of COVID-19 was recorded in Sulaymanyaih City, Kurdistan Region, Iraq, on March 1st, 2020 (4). Since then, 397 confirmed COVID-19 cases, five deaths, and 377 recoveries had been reported (5). In addition, all the five recorded deaths had underlying health conditions and only two of them were hospitalized COVID-19 patient, the rest were confirmed to have died of COVID-19 base on post-mortem examination of the corpses (6).
We believe the disease was started as early as the time of the outbreak in Wuhan, Hubei, China. It is known to the resident of the Kurdistan Region of Iraq that we have a severe form of flu during last fall, 2019 (6). Our hypothesis is based on re-examination of the CT scan data of two male patients admitted to the Faruk Medical City (FMC) in Sulaymaniyah city with "flu-like illness", which both had lymphopenia in 19 and 23, December 2019. Although real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) kits are commonly used to diagnose COVID-19, many developing countries do not have access to enough kits rRT-PCR can frequently have false positive. Therefore, CT scans are a golden standard that provides quick diagnosis for the suspected infected people, and the presence of ground-glass opacity (GGO) pattern is generally considered as a characteristic feature of the COVID-19's infection (7).
Chest CT in patients with COVID-19 most commonly demonstrates ground-glass opacification with or without consolidative abnormalities, consistent with viral pneumonia. Case series have suggested that chest CT abnormalities are more likely to be bilateral, have a peripheral distribution, and involve the lower lobes. Less common findings include pleural thickening, pleural effusion, and lymphadenopathy (8, 9). Common laboratory findings among hospitalized patients with COVID-19 include lymphopenia, elevated aminotransaminase levels, elevated lactate dehydrogenase levels, and elevated inflammatory markers (eg, ferritin, C-reactive protein, and erythrocyte sedimentation rate) (10).
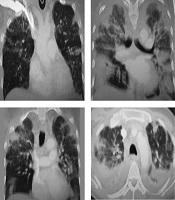
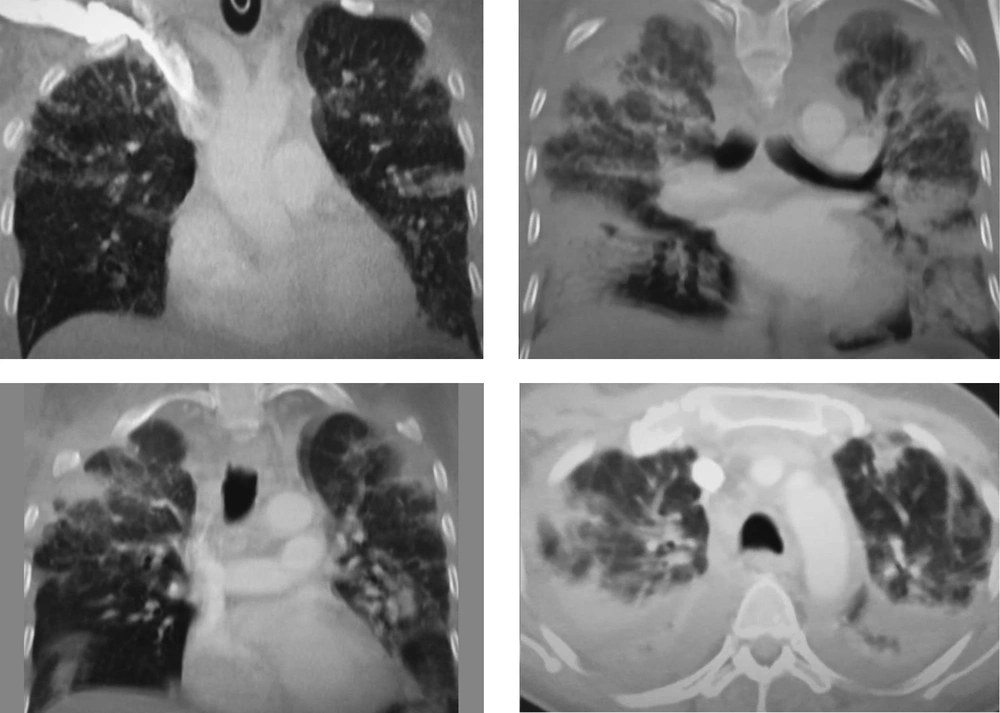
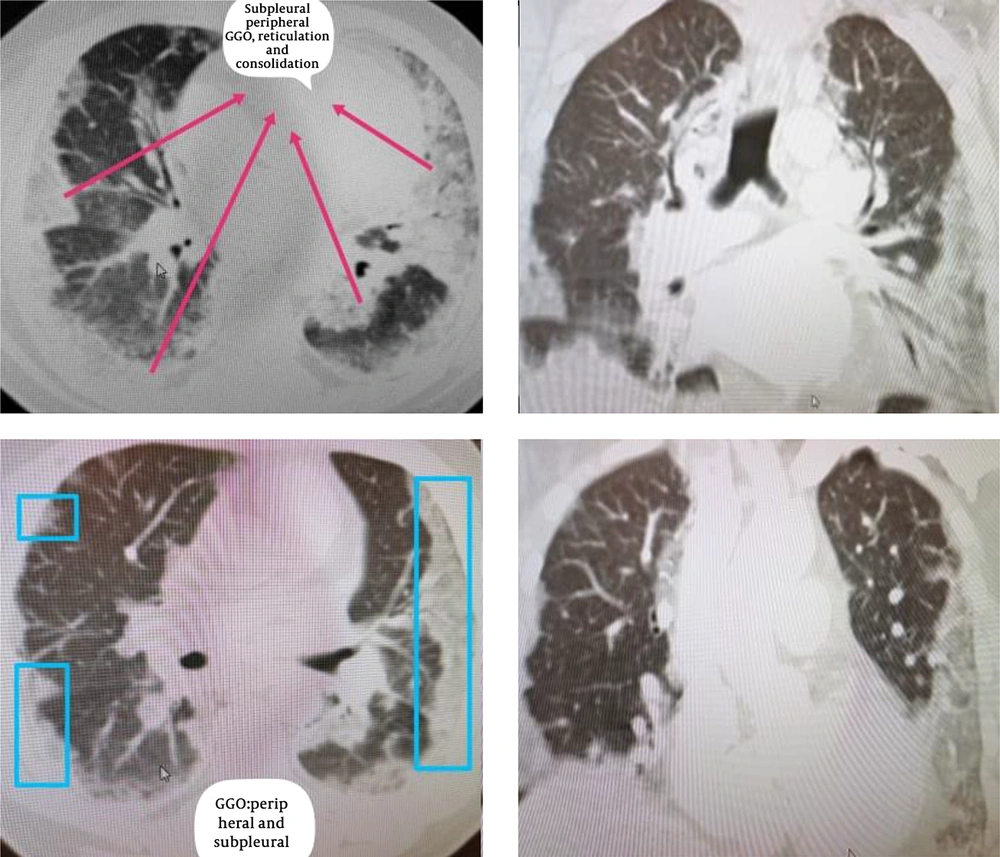
A 51 year-old-male patient with flu-like illness, he rapidly deteriorated and intubated; after 1 month, he died (Figure 1). A 49-year-old male had no significant past medical history, nonsmoker presented with flu-like illness, cough and fever, not responded to supportive medications, after 1 week he developed, chest pain, severe dyspnea and resistant hypoxia associated with many bouts of loose bowel motions. Spo2 = 77% on air and 10 - 15 L of O2 on nonrebreather mask still did not reach 90%. Ct chest (Figure 2) showed bilateral mainly peripheral subpleural lower lobe predominant Ground glass opacities, reticulations, and patchy consolidations with air bronchogram no pleural effusion, no lymphadenopathy. CTPA excluded pulmonary embolism, high ESR, CRP, liver function test. Normal heart assessment, Clostridium difficile, anti-toxin A + B was negative. The patient did not respond to the broad-spectrum antibiotics, tamiflu, methylprefnisolone. After two weeks he gradually improved and now survived with no any complication.
An axial CT image obtained without intravenous contrast in a 49-year-old male in the “late” time 23 December 2019 (10 days from symptom onset to this CT) shows bilateral reticulations and patchy consolidations opacities, with a striking subpleural peripheral distribution, subpleural lower lobe predominant Ground glass opacities.
To conclude, we believe the herd immunity is a key protection of the Kurdistan Region's residence against the disease. Such immunity was acquired from the early spread of SARS-CoV-2 in the region back to December 2019. Further studies are required to investigate these factors and confirm the reason for less severity of the COVID-19 disease in the Kurdistan Region of Iraq compared to the other country.