1. Background
Klebsiella pneumoniae is an important opportunistic pathogen that causes a wide range of clinical diseases, including hospital acquired pneumonia, urinary tract, digestive, and blood infections, skin and soft tissue infections, and septicemia in immunocompromised patients (1-3). K. pneumoniae is a Gram-negative, rod-shaped, aerobic, non-motile bacillus with a large polysaccharide capsule. It is one of the most important enteric bacteria accountable for up to 10% of nosocomial infections associated with high morbidity and mortality rates (4).
Antimicrobial resistance (AMR) is a major health concern worldwide (5, 6), as well as a major cause of treatment failure in infectious diseases, which is associated with increased morbidity, mortality, and financial burden on the healthcare system (7). It is estimated that approximately 700,000 deaths occur each year due to AMR. Furthermore, it is predicted that if appropriate control and prevention measures are not taken, AMR could become a leading cause of mortality in hospitalized and non-hospitalized patients in developing and developed countries (8).
The emergence of multidrug-resistant K. pneumoniae is considered to be a global public health issue (9). The carriage of K. pneumoniae and development of multidrug-resistant bacteria have increased due to the frequent use of broad-spectrum antibiotics for hospitalized patients (10). In several countries, K. pneumoniae has developed resistance to the most common antibiotics and even the higher classes of antibiotics, such as third-generation cephalosporins (11). In addition, K. pneumoniae has been reported to be the most common pathogenic bacteria to develop resistance to broad-spectrum beta-lactam antibiotics via extended-spectrum beta-lactamase (ESBL) (5).
Previous studies in Duhok City, Iraq have denoted the alarming rates of antibiotic resistance to several bacteria (12-15). While the continuous monitoring of antibiotic sensitivity patterns is essential to the treatment of various infections, the current data is scarce on K. pneumoniae in Duhok City.
2. Objectives
The present study aimed to determine the antimicrobial susceptibility pattern of K. pneumoniae isolated from various clinical specimens in Duhok City, located in the Kurdistan Region of Iraq.
3. Methods
3.1. Sample Collection and Processing
This cross-sectional study was conducted at a private clinical health center in Duhok City during January 2017-February 2019 on 130 isolates that were obtained from various clinical specimens, including 86 urine specimens, 16 blood specimens, nine sputum specimens, 13 wound swabs, three central venous (CV) lines, and three oral swabs. The patients were within the age range of 10 - 65 years from both genders (31 males and 99 females). All the patients were clinically positive for K. pneumoniae and examined in accordance with the standard operation procedure.
Clean-catch midstream urine specimens were collected using sterile disposable glass containers (5 mL) from the patients in order to avoid contamination. Blood samples were obtained from the patients aseptically in blood culture tubes, and sputum was collected from each patient using sputum containers with screw caps. In addition, the clinical wound and oral samples were collected using sterile cotton swabs.
The inclusion criteria of the study were as follows: (1) both male and female patients; (2) age of more than 10 years; (3) positive microbiological evidence of K. pneumoniae and (4) consent to participate in the study. The patients who did not consent to participate were excluded.
3.2. Identification and Antimicrobial Sensitivity
The clinical isolates of K. pneumoniae were identified based on the morphological characteristics on the MacConkey agar media. The large mucoid colonies obtained from the MacConkey agar plate were classified based on the gram stain according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI). In the gram staining, all the isolates were confirmed as gram-negative and rod-shaped. The identification of K. pneumoniae and antimicrobial susceptibility testing were performed using the VITEK-2 compact bacterial identification and monitoring system (bioMerieux, US) in accordance with the instructions of the manufacturer.
3.3. Ethical Considerations
The study protocol was approved by the Ethics committee of the College of Medicine at the University of Zakho in Kurdistan Region, Iraq. Informed consent was obtained from all the patients prior to participation.
4. Results
In total, 130 positive K. pneumoniae cultures of various clinical samples were evaluated. The highest number of the K. pneumoniae isolates was obtained from the urine samples (n = 86; 66.2%), followed by the blood samples (n = 16; 12.3%), and wound swabs (n = 13; 10%) (Table 1). In terms of gender, the female patients were more affected by K. pneumoniae (n = 99; 76.2%) compared to the males (n = 31; 23.8%) (Table 1). Moreover, the distribution of K. pneumoniae was higher in the females compared to the males in the urine, blood, wound, and oral samples. However, the distribution of the isolates was higher in the males compared to the females in the CV line and sputum samples (Table 1).
| Source of Isolation | Gender | Total | |
|---|---|---|---|
| Male | Female | ||
| Urine | 14 (16.3) | 72 (83.7) | 86 (66.2) |
| Blood | 2 (12.5) | 14 (87.5) | 16 (12.3) |
| Wound Swab | 4 (30.8)) | 9 (69.23) | 13 (10) |
| Sputum | 8 (88.9) | 1 (11.1) | 9 (6.9) |
| CV Line | 2 (66.7) | 1 (33.3) | 3 (2.3) |
| Oral Swab | 1 (33.3) | 2 (66.7) | 3 (2.3) |
| Total | 31 (23.8) | 99 (76.2) | 130 (100 |
Distribution of K. pneumoniae Isolated From Various Clinical Specimens in Terms of Gendera
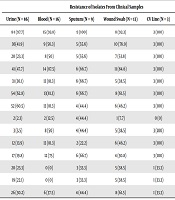
Table 2 shows the resistance rate of the isolated K. pneumoniae from various clinical samples to common antibiotics. In the urine samples, K. pneumoniae was observed to be highly resistant to ampicillin (97.7%), ceftriaxone (62.8%), and cefepime (60.5%), while also highly sensitive to ertapenem (97.7%) and imipenem (96.5%). K. pneumoniae isolated from the blood samples was extremely effective against ciprofloxacin (100%) and levofloxacin (100%), while the K. pneumoniae isolates were resistant to ampicillin (93.8%) and cefazolin (87.5%), and approximately 81% were resistant to cefoxitin, ceftriaxone, cefepime, and gentamicin (Table 2).
| Resistance of Isolates From Clinical Samples | ||||||
|---|---|---|---|---|---|---|
| Antibiotic | Urine (N = 86) | Blood (N = 16) | Sputum (N = 9) | Wound Swab (N = 13) | CV Line (N = 3) | Oral Swab (N = 3) |
| Ampicillin | 84 (97.7) | 15 (93.8) | 9 (100) | 8 (92.3) | 3 (100) | 3 (100) |
| Amoxicillin/clavulanic acid | 36(41.9) | 9 (56.3) | 5 (55.6) | 10 (76.9) | 3 (100) | 1 (33.3) |
| Piperacillin/tazobactam | 20 (23.3) | 8 (50) | 5 (55.6) | 7 (53.8) | 3 (100) | 0 (0) |
| Cefazolin | 41 (47.7) | 14 (87.5) | 6 (66.7) | 11 (84.6) | 3 (100) | 2 (66.7) |
| Cefoxitin | 31 (36.1) | 13 (81.3) | 6 (66.7) | 5 (38.5) | 3 (100) | 0 (0) |
| Ceftriaxone | 54 (62.8) | 13(81.3) | 6 (66.7) | 8 (61.5) | 3 (100) | 1 (33.3) |
| Cefepime | 52 (60.5) | 13 (81.3) | 4 (44.4) | 6 (46.2) | 3 (100) | 1 (33.3) |
| Ertapenem | 2 (2.3) | 2 (12.5) | 4 (44.4) | 1 (7.7) | 0 (0) | 0 (0) |
| Imipenem | 3 (3.5) | 8 (50) | 4 (44.4) | 5 (38.5) | 3 (100) | 0 (0) |
| Gentamicin | 12 (13.9) | 13 (81.3) | 2 (22.2) | 6 (46.2) | 3 (100) | 0 (0) |
| Tobramycin | 17 (19.8) | 12 (75) | 6 (66.7) | 4 (30.8) | 3 (100) | 0 (0) |
| Ciprofloxacin | 20 (23.3) | 0 (0) | 3 (33.3) | 5 (38.5) | 1 (33.3) | 0 (0) |
| Levofloxacin | 19 (22.1) | 0 (0) | 3 (33.3) | 5 (38.5) | 1 (33.3) | 0 (0) |
| Nitrofurantoin | 26 (30.2) | 6 (37.5) | 4 (44.4) | 8 (61.5) | 1 (33.3) | 2 (66.7) |
Antibiotic Resistance Pattern of K. pneumoniae Strains Isolated From Clinical Samplesa
According to the findings, 100% of the isolated K. pneumoniae from the sputum samples were resistant to ampicillin, and 77.8% were sensitive to gentamicin (Table 2). The sensitivity of the K. pneumoniae isolated from the wound swabs to ertapenem was estimated at 92.3%, while these isolates were highly resistant to ampicillin (92.3%). The strains isolated from the CV line exhibited the highest resistance rates against all the antibiotics, with the exception of ertapenem (Table 2). In addition, 100% of the isolated K. pneumoniae from the oral swabs were highly sensitive to all the common antibiotics, with the exception of ampicillin (Table 3).
| Antibiotic | Susceptibility Patterns (N = 130) | |
|---|---|---|
| Resistance | Sensitivity | |
| Ampicillin | 126 (96.9) | 4 (3.1) |
| Amoxicillin/clavulanic acid | 63 (48.5) | 67 (51.5) |
| Piperacillin/tazobactam | 43 (33.1) | 87 (66.9) |
| Cefazolin | 77 (59.2) | 53 (40.8) |
| Cefoxitin | 58 (44.6) | 72 (55.4) |
| Ceftriaxone | 85 (65.4) | 45 (34.6) |
| Cefepime | 79 (60.8) | 51 (39.2) |
| Ertapenem | 8 (6.2) | 122 (93.8) |
| Imipenem | 23 (17.7) | 107 (82.3) |
| Gentamicin | 34 (26.2) | 96 (73.8) |
| Tobramycin | 40 (30.8) | 90 (69.2) |
| Ciprofloxacin | 29 (22.3) | 101 (77.7) |
| Levofloxacin | 29 (22.3) | 101 (77.7) |
| Nitrofurantoin | 40 (30.8) | 90 (69.2) |
Overall Antimicrobial Susceptibility Pattern of K. pneumoniae Isolated From Various Clinical Specimensa
Table 3 shows the overall susceptibility profile of the K. pneumoniae isolates from various clinical specimens. Accordingly, 96.9%, 65.8%, and 60.8% of the isolated K. pneumoniae strains were resistant to ampicillin, ceftriaxone, and cefepime, respectively. However, the highest sensitivity rate was observed against ertapenem (93.8%) and imipenem (82.3%) (Table 3).
5. Discussion
K. pneumoniae is an important causative agent of several clinical diseases, including urinary tract infection, pneumonia, skin and soft tissue infections, and bacteremia septicemia, which are associated with high morbidity and mortality (2, 3). Currently, drug resistance to human pathogenic bacteria such as K. pneumoniae is frequently reported worldwide (9). This is considered to be an alarming issue in both developing and developed countries due to the wide usage of the antibiotics used in medical practice (5). To investigate the potential difference in drug resistance, we analyzed the K. pneumoniae isolated from various clinical specimens in Duhok City (Iraq) in the present study.
In the present study, 130 K. pneumoniae isolates were collected from various clinical sample sources. Among the patients, K. pneumoniae infection was the predominant organism recovered from the urine samples (66.2%), followed by the blood samples (12.3%) and wound swabs (10%). Several studies in Iraq have reported that urine is a most common source of urinary tract infection (14, 16, 17). For instance, Riaz et al. (3) and Akter et al. (6) reported that urine is the principle source of Klebsiella species.
Regarding gender, the findings of the current research indicated that the frequency of the K. pneumoniae isolated from various clinical samples was higher in the female patients (76.2%) compared to the males (23.8%). In the case of the urine, blood, wound, and oral samples, the female patients were observed to be more affected by K. pneumoniae compared to the males, while in the case of the CV line and sputum samples, the frequency of the isolates was higher in the males compared to the females. This is consistent with the studies reporting that K. pneumoniae was the more predominant pathogen isolated from female patients compared to male patients (8), while in contrast to a study conducted in Bangladesh, the results of which indicated that male patients were more susceptible to Klebsiella infection isolated from urine and wound samples compared to females (6). This discrepancy is rather difficult to explain and could be due to the variations in the sample collection, study design, sample population, inclusion criteria of patients, environmental factors, and personal hygiene.
K. pneumoniae was observed to be the most prevalent causative agent isolated from the female patients with urinary tract infection in the present study, which could be due to several factors, such as the shortness of the urethra and its proximity to the anus in women as a major cause of urinary tract infection. In addition, sexual activities could also increase the inoculation of the pathogen into the bladder in women (18). In a study conducted in Iran, K. pneumoniae was reported to be the most prevalent infection in female patients to cause urinary tract infection (4). The other studies conducted in Iran have also denoted that women tend to be affected more frequently by K. pneumoniae and experience urinary tract infection more commonly than men (2).
The effectiveness of currently available antibiotics is declining due to the increasing number of the resistant strains that cause infections (11). The available therapeutic options for antibiotic-resistant pathogens are severely limited as these pathogens frequently exhibit a multidrug-resistant phenotype (19, 20). In the present study, K. pneumoniae isolated from various clinical samples demonstrated variable degrees of sensitivity to the common antibiotics. In addition, K. pneumoniae isolated from the urine samples was highly resistant to ampicillin (97.7%), while highly effective against ertapenem (97.7%) and imipenem (96.5%).
According to a research performed in Iraq, 100% of isolated Klebsiella strains were resistant to meropenem and amikacin (17), which is in line with the results of another study in Bangladesh, showing that all Klebsiella isolates were highly resistant to ampicillin (100%) (10). In the same study, Klebsiella was reported to be moderately sensitive to ceftriaxone, ciprofloxacin, and gentamicin (10). However, another study in Pakistan indicated that Klebsiella isolates from urine samples were sensitive against gentamicin (21). The discrepancy between our findings and the aforementioned studies regarding the higher sensitivity against gentamicin may be due to selective pressure in various regions.
According to the current research, K. pneumoniae isolated from the blood samples was highly sensitive to levofloxacin (100%) and ciprofloxacin (100%). However, the K. pneumoniae isolates showed maximum resistance to ampicillin (93.8%) and cefazolin (87.5%), approximately 81% of which were also resistant to cefoxitin, ceftriaxone, cefepime, and gentamicin. This finding is comparable with the studies conducted in developing countries, reporting that Klebsiella isolates showed 100% resistance to ampicillin (22, 23), which could be due to the widespread use of this antibiotic owing to the low cost and easy administration.
In the present study, 100% of the isolated K. pneumoniae from the sputum samples were resistant to ampicillin, and approximately 78% of the isolates were sensitive to gentamicin. This is in line with the results of a study conducted in India, which indicated that 92% of the Klebsiella isolates from sputum showed resistance to ampicillin (8). However, this is inconsistent with the other studies that indicated that the majority of the strains isolated from sputum were sensitive to amikacin (24). In the current research, the sensitivity of the K. pneumoniae isolated from the wound swabs to ertapenem and levofloxacin was estimated at 87.5% and 75%, respectively, while 100% resistance was recorded to ampicillin. In addition, ertapenem (100%) was observed to be the most potential drug against the K. pneumoniae isolated from the digestive system, followed by imipenem, gentamicin, and tobramycin, while it was highly resistant to ampicillin, amoxicillin/clavulanic acid, cefazolin and ceftriaxone. In a study conducted in Iraq, the K. pneumoniae bacterium was mostly sensitive to amikacin and imipenem, while mostly resistant to ceftriaxone and tetracycline (24).
Unfortunately, the strains isolated from the CV line in the present study showed high resistance rates to all the common antibiotics, with the exception of ertapenem, which could be dispensed without prescription. Therefore, patients and general public education are crucially required in this regard. Widespread, excessive dispensing and irresponsible use of antibiotics have led to the development of multi-resistant strains. On the other hand, 100% of the isolated K. pneumoniae strains from the oral swabs in the current research were highly sensitive to all the common antibiotics, with the exception of ampicillin. These antibiotics should be the preferred drugs for the treatment of the K. pneumoniae infections isolated from oral swabs. Penicillin resistance is due to the ability of K. pneumoniae to carry the plasmid-producing beta-lactamase variants (21), and beta-lactamase production is considered to be the most common mechanism of gram-negative pathogens (22).
In terms of the overall susceptibility pattern of the K. pneumoniae isolates of various clinical specimens, it was observed that the K. pneumoniae isolates were highly resistant to ampicillin, ceftriaxone, and cefepime, while the highest susceptibility rate was observed against ertapenem and imipenem. These antibiotics have been proposed as alternatives for the treatment of K. pneumoniae infections in the studied region, which is in contrast to another study conducted in Iraq, the results of which indicated that amikacin, ciprofloxacin, and gentamicin were the most effective antimicrobial agents against K. pneumoniae (23). According to another research, K. pneumoniae isolates obtained from clinical samples exhibited good sensitivity to amikacin and meropenem, while they were only moderately sensitive to levofloxacin, ceftazidime, and ciprofloxacin. Therefore, it could be inferred that the resistance rate of the isolates from various sample sources in the current research have numerous differences in comparison with the aforementioned studies in all the antibiotics, which could be due to the significant differences in the sample size, sampling methods, and geographical/environment variations. In addition, the high resistance rate to ampicillin, ceftriaxone, and cefepime antibiotics in the present study compared to other countries is rather alarming in terms of the spread of antibiotic resistance among the clinical isolates in our region. This shows the limited possibility of using these antibiotics in the empirical treatment of the patients with K. pneumoniae infections. Therefore, an urgent measure is required to control the threatening development of such resistance in the country.
The main limitation of the present study was the small sample size (n = 130). In addition, the study was mainly conducted in Duhok City, and the patients aged less than 10 years were not evaluated. Therefore, further investigations are required in this regard using advanced molecular tools to diagnose and evaluate the sensitivity of bacteria in order to overcome these limitations and obtained more accurate results.
5.1. Conclusions
According to the results, K. pneumoniae infection was the predominant bacteria isolated from the urine samples in the female patients. Ertapenem and imipenem were observed to be the most effective antibiotics against the K. pneumoniae isolates from various clinical samples. However, the isolates were extremely resistant to ampicillin, ceftriaxone, and cefepime. The emergence of resistant bacteria to various antibiotics has urged the periodic assessment of empirical, first-line antibiotic treatments at a regional level. Our findings could help physicians and clinicians to select appropriate antimicrobial therapies in this regard.