1. Introduction
Acute pancreatitis may lead to severe complications and even significant mortality if it is not diagnosed and treated in a timely manner. Timely diagnostic and therapeutic measures could prevent the complications of the disease in numerous cases. The most common signs and symptoms of acute pancreatitis include abdominal pain, nausea and vomiting, diarrhea, fever, tachycardia, and dyspnea (1). Various diagnostic methods are applied for acute pancreatitis, including laboratory tests, abdominal radiographs, abdominal ultrasound, endoscopic ultrasonography, and CT-scan (2). Increased serum levels of amylase and lipase enzymes are considered to be significant indicators of acute pancreatitis.
In this case study, we described the history of the disease in contrast to the common cases (i.e., normal enzymes) with different radiological evidence supporting acute pancreatitis.
2. Case Presentation
Our patient was a 31-year-old man presenting with abdominal pain and two periods of biliary vomiting and food intolerance. The patient’s pain was predominantly perceived in the right half of the abdomen and epigastrium. The patient also had a fever and chills and no history of melena, hematemesis, and any specific diseases. However, he had a history of opium and alcohol use.
Baseline vital signs included the blood pressure of 115.65, pulse rate of 120, respiratory rate of 30, and temperature of 38°C. Initially, the patient was fully conscious and oriented despite appearing restless on physical examination. He also had normal heart sounds without heart murmur, and the lungs had normal hearing as well. There was tenderness on the right abdomen and epigastrium and no organomegaly on the abdominal palpation. Neurological examinations were normal.
2.1. Laboratory Results
White blood cell count was 10,800, hemoglobin was 19.6, platelet count was 104, blood sugar was 222, sodium level was 132, potassium level was 4.4, calcium level was 16.5, liver enzymes were measured to be 58 and 38, creatinine level was 0.5, sedimentation was estimated at 97, C-reactive protein was 48, total bilirubin was 0.8, lipase was 88.99, and amylase level was estimated at 74.
2.2. Chest X-Ray
No specific pathological findings were observed in the lung scan of the patient.
2.3. Abdominal and Pelvic CT-Scan
Edema and stranding of pancreatic tissue and peripancreatic showing pancreatitis. A focus of non enhancement seen in trunk of pancreas with volume of < 30%, suggesting necrosis; evidence of acute necrosis seen in spaces of peripancreatic masses and with spread to paracolic gutters on both sides; evidence suggesting necrotizing pancreatitis) (Figure 1).
Edema and stranding of pancreatic tissue and peripancreatic showing pancreatitis. A focus of non enhancement seen in trunk of pancreas with volume of < 30%, suggesting necrosis; evidence of acute necrosis seen in spaces of peripancreatic masses and with spread to paracolic gutters on both sides; evidence suggesting necrotizing pancreatitis).
2.4. Ultrasound
Ultrasound was performed for the free fluid in the splenorenal space and Morrison’s pouch, and the pancreas was observed to be heterogeneous and larger than normal. Furthermore, there was evidence of perivascular inflammation and inflammatory changes around the pancreas, extending to the right anterior parenchyma with the less involvement of the left anterior parenchyma caused by acute pancreatitis. The liver had normal dimensions and echo, the gallbladder was without stones and slug of intrahepatic bile ducts, and common bile duct was normal as well.
2.5. Subsequent Tests
As mentioned earlier, triglycerides were measured, and the level was estimated at 1,415 (normal < 150).
2.6. Patient Procedures and Treatment
Due to respiratory distress and seizures, the patient was intubated in the emergency section upon admission to the ICU. After eight days, the patient was extubated and transferred to the ward. Notably, the patient had an early admission to the dialysis ward due to aneuria and hypercalcemia, and endocrine counseling was provided for the high triglycerides; no apheresis was required. After stabilization, the patient underwent an endoscopic ultrasound, and after several days of antibiotic treatment, he was discharged in good overall condition and advised to refer to an outpatient clinic after one week.
3. Discussion
Laboratory tests are reliable diagnostic approaches for acute pancreatitis. Furthermore, the serum levels of amylase and lipase are significantly elevated in patients with acute pancreatitis, often reaching three times the normal level as observed in the previous studies in this regard (3). Amylase levels in patients with acute pancreatitis may be normal or extremely low due to hypertriglyceridemia or alcohol consumption (4). Previous findings have indicated that normal amylase levels in acute pancreatitis are secondary to hypertriglyceridemia, performing serial amylase test can reduce thetrigyceride interference (5-8).
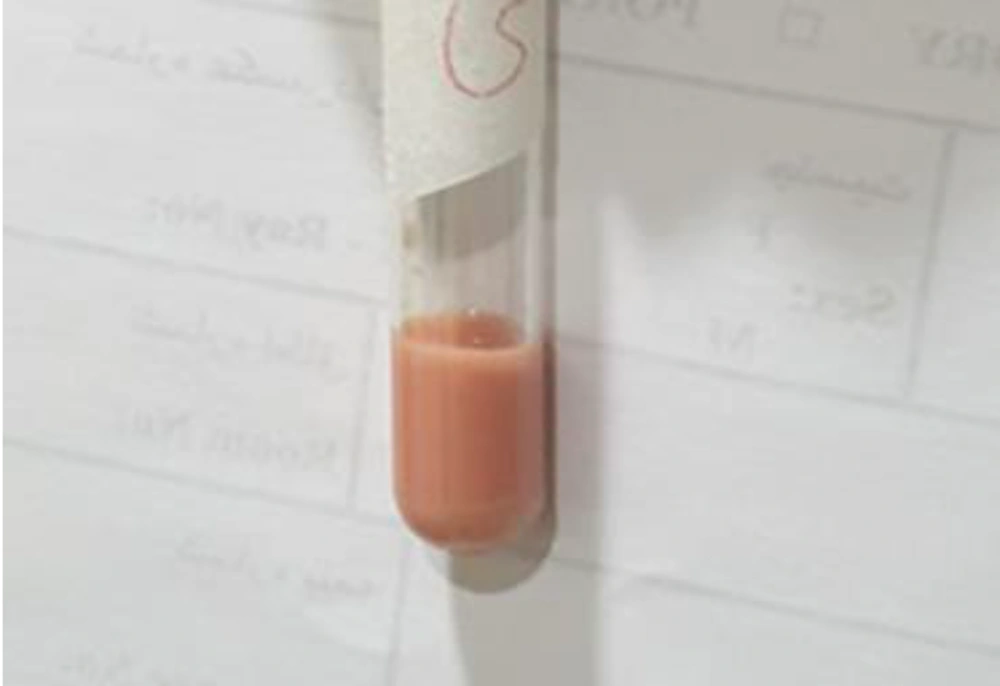
According to our findings in this case report, the use of other diagnostic methods seems essential to imaging and ultrasound where there is strong clinical suspicion (Figure 2).