1. Background
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-COV-2), which emerged in Wuhan, China, in December 2019 (1). The most common clinical manifestations are fever (80%), cough (63%), fatigue (46%), and expectoration (42%) (2, 3).
The virus spread worldwide rapidly within the first few months of identification, persuading the World Health Organization (WHO) to declare COVID-19 a “public health emergency of international concern” as of February 1, 2020 (4). In Iran, the first case of coronavirus death was reported in the city of Qom which was indeed the first registered coronavirus death in the Middle East (5, 6). By March 5, 2020, all 31 provinces of the country had been involved. Following two deaths in Qom, Iranian officials announced the COVID-19 outbreak in the country (7). However, initially, Iran did not adopt any lockdown or traffic restriction policy, which led to the rapid expansion of COVID-19. As of February 29, 2020, all schools and universities, and as of March 7, 2020, almost all public places and shrines were closed. On March 26, 2020, the National Committee on COVID-19 placed more restrictions to be executed until April 4, 2020 (8).
These stress responses during a threatening event (such as the COVID-19 outbreak) are associated with adverse physical and mental health outcomes (9, 10). Consequently, unnecessary healthcare referrals of individuals who are worried about their health status due to the COVID-19 epidemic could increase the risk of contamination with SARS-CoV-2 (11). On the other hand, the COVID-19 pandemic reduced the referrals of patients with chronic diseases such as diabetes mellitus, cardiovascular, and neurological diseases, which is worrying (12).
During health crises, the public demand for and reliance on the media increased (13). However, timely updates from trusted sources such as WHO might have decreased fears, rumors, stress responses, and unreasonable demand for healthcare facilities. Regardless of the crucial role of media in informing the community of health threats, news coverage has the potential to contribute to an increase in healthcare facilities in emergency departments (14). Therefore, appropriate precautions must be taken to ensure that news coverage provides the community with urgent information, while simultaneously mitigating news exposures that can lead to traumatic stress responses.
2. Objectives
The present study aimed to investigate the trend of COVID-19 referrals to IKHC during the first peak and compare their features and present symptoms. The study also aimed to evaluate the role of media and health management planning in changing referral patterns. The results of this study can help health policy makers to prepare for future epidemics as well as the likely future peaks of the current pandemic.
3. Methods
This retrospective cohort study was conducted using the centralized electronic medical database of IKHC. The characteristics of individuals with COVID-19 symptoms referring to IKHC from February 20 to June 4, 2020, were extracted on June 7 from the hospital’s electronic medical database. Each individual’s birth date, sex, comorbidities, symptoms, referral sites, laboratory-confirmed cases, chief complaint, demographic characteristics, and underlying health conditions were registered. They were also divided into two groups, COVID-19 positive and negative.
This study was approved by the Research Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.VCR.REC.1399.051). The patients’ personal information and data were kept confidential and secure.
3.1. Participants
The patients included in this study had attended the respiratory emergency due to COVID-19 symptoms or simply because of the fear of infection. Besides, some patients were admitted from other wards with chief complaints other than COVID-19 and were then examined for COVID-19 infection according to their symptoms. The hospitalization criteria were in accordance with the health administration protocol (15) and are as the following:
Patients with an underlying health condition are divided into two groups:
(1) High-risk A who are defined as: (a) patients undergoing corticosteroids treatment (> 20 mg/dL prednisolone for more than two weeks or cumulative dose more than 600 mg equivalent to prednisolone), (b) patients undergoing chemotherapy, (c) patients with an organ transplant, and (d) patients with a known malignancy;
(2) High-risk B who are defined as: (a) patients with hypertension, (b) patients with uncontrolled diabetes (HbA1c > 7.6%), (c) patients with cardiovascular diseases, (d) patients with body mass index (BMI) > 40, (e) patients with an underlying respiratory disease, and (f) patients with CKD.
Every patient with dyspnea or oxygen saturation lower than 93% or respiratory rate above 30 was hospitalized and tested for COVID-19 infection. All patients with group A risks underwent a computed tomography scan (CT scan), but in group B risks, only febrile patients with an axillary temperature above 37.8°C underwent a CT scan. If the CT scan findings suggested COVID-19, polymerase chain reaction (PCR) test was performed. Individuals with positive PCR tests were identified as COVID-19 patients. Other individuals with suspected COVID-19 infection were advised to be quarantined and stay home until full recovery. They were also advised to refer to the hospital in case of exacerbation of their conditions.
3.2. Measures
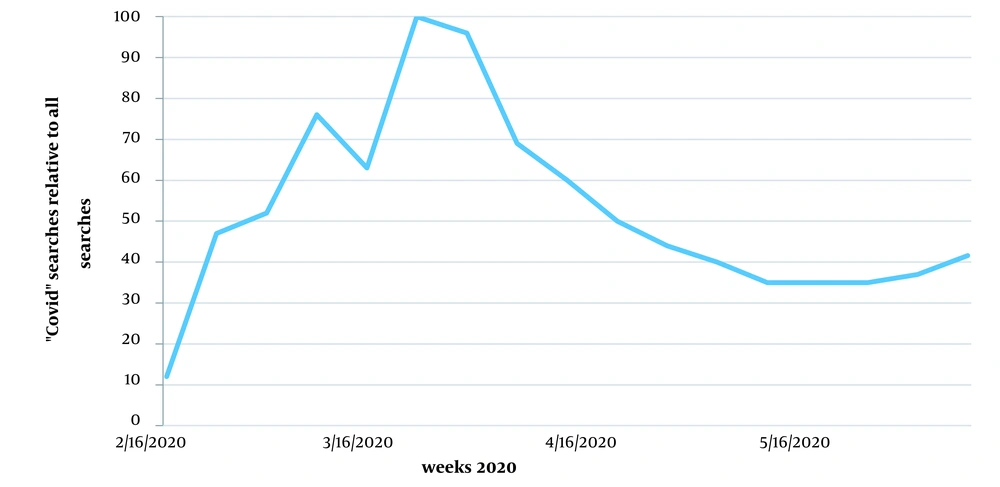
This study examined the referral pattern from February 20 to June 4, 2020, along with public concern and health management planning during that period. The Google Trends (https://trends.google.com/trends; Google Inc., Mountain View, CA) was used to examine the Google Internet search queries from the country using the search term “Coronavirus” during the mentioned period for analyzing public concern. Numbers represent search interests for the given region and time. A value of 100 denotes the peak of popularity of the term, a value of 50 indicates that the term is almost popular, and a score of 0 means a lack of enough data for this term (16).
Available policy documents, programs, action plans, reports, websites, and the official news related to COVID-19 in Iran (mostly the Iranian Ministry of Health and Medical Education [MoHME]) were used to examine government policy and health management planning (17).
3.3. Statistical Analysis
Continuous variables with normal distributions were expressed as means ± standard deviation (SD), and categorical variables were defined as proportions or ratios. Continuous variables with skewed distribution were expressed as medians and interquartile ranges. The data were analyzed using SPSS 25.0. (SPSS Inc., Chicago, USA).
4. Results
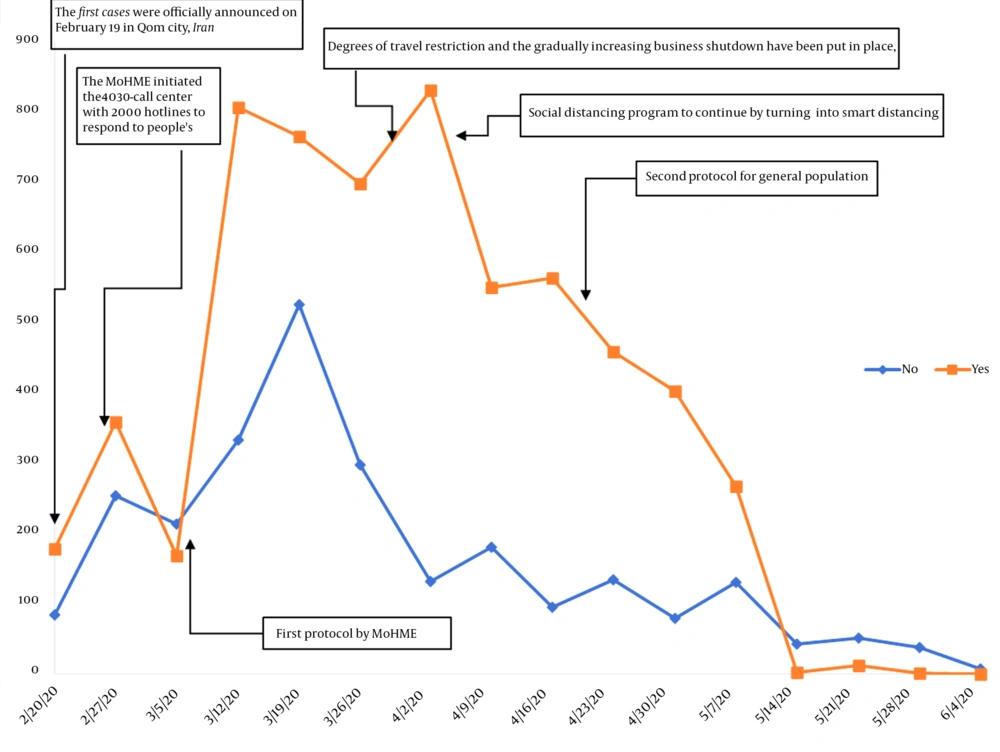
Data of 8647 individuals visiting IKHC due to COVID-19 from February 20 to June 4, 2020 were reviewed. Weekly hospital admissions during the study period are shown in Figure 1. There were large increases in hospital admissions in both COVID-19 negative and positive groups, with the most rapid increase during March 5 - 11, 2020. The largest difference in the admission rates of the two groups was observed during April 2 - 8, 2020. Rates of hospital admissions were the lowest in both COVID-19 negative and positive groups during May 14 - 20, 2020.
Table 1 shows the weekly referral numbers according to COVID-19 status. The total number of referrals had increased until the week of March 19 - 25 and peaked during this week and then decreased until June 4, 2020. The attendance of COVID-19 negative individuals peaked during March 19 - 25. The attendances of individuals with a positive COVID-19 test had increased until the week of March 12 - 18 and decreased slightly until the beginning of the week of April 2 - 8 and peaked during this week.
| Admission Week (the Year 2020) | Total | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2.20 | 2.27 | 3.05 | 3.12 | 3.19 | 3.26 | 4.02 | 4.09 | 4.16 | 4.23 | 4.30 | 5.07 | 5.14 | 5.21 | 5.28 | 6.04 | ||
| COVID-19 | |||||||||||||||||
| No | 84 (3.2) | 253 (9.8) | 213 (8.2) | 333 (12.8) | 525 (20.2) | 297 (11.5) | 131 (5.1) | 180 (6.9) | 95 (3.7) | 134 (5.2) | 79 (3) | 130 (5) | 43 (1.7) | 51 (2) | 38 (1.5) | 7 (0.3) | 2593 (100) |
| Yes | 178 (2.9) | 358 (5.9) | 168 (2.8) | 805 (13.3) | 764 (12.6) | 697 (11.5) | 829 (13.7) | 549 (9.1) | 563 (9.3) | 458 (7.6) | 402 (6.6) | 267 (4.4) | 3 (0) | 12 (0.2) | 1 (0) | 0 (0) | 6054 (100) |
| Total | 262 (3) | 611 (7.1) | 381 (4.4) | 1138 (13.2) | 1289 (14.9) | 994 (11.5) | 960 (11.1) | 729 (8.4) | 658 (7.6) | 592 (6.8) | 481 (5.6) | 397 (4.6) | 46 (0.5) | 63 (0.7) | 39 (0.5) | 7 (0.1) | 8647 (100) |
a Values are expressed as No. (%).
According to information announced by MoHME, the government policies in response to the pandemic were as follows (Table 2):
| Date | Measures and Policies in Response to COVID-19 Pandemic |
|---|---|
| 1/31/2020 | Preventing passengers coming from China from entering Iran due to the risk involved |
| 2/01/2020 | Calling for a temporary halt on round-trip flights from Iran to China and vice versa due to the spread of COVID-19 |
| 2/26/2020 | Setting up the 4030-call center with 2000 hotlines to respond to people’s queries |
| 3/08/2020 | Issuing the first protocol (by MoHME) |
| 3/11/2020 | Releasing the first protocol for hospital admission |
| 3/26/2020 | Discouraging and partially restricting travel and gradually increasing business shutdowns until March 26, 2020; Executing more restrictions until April 4, 2020 |
| 4/04/2020 | Carrying on the social distancing program by turning it into a smart social distancing |
| 4/05/2020 | Smart social distancing: Medium and low-risk businesses can start their activities from April 11 with strict observance of health protocols, but high-risk businesses will remain closed until April 19. Regarding the offices that are currently active, as of next week, April 11, their activities will continue with two-thirds of their personnel at work while one-third will be allowed to work from home. |
| 4/19/2020 | Releasing a new protocol for the community |
The first protocol was released by MoHME on March 8, 2020. Before this time, the country had not adopted a complete lockdown policy. Restrictions on the number of travels and a gradual increase in business shutdown had been imposed until March 26, 2020, when the National Committee for COVID-19 placed more restrictions to be executed until April 4, 2020. On April 4, 2020, MoHME (18) initiated the social distancing program followed by smart social distancing program which was defined as the following: “Medium and low-risk businesses in provinces all around the country can start their activities from April 11 with strict observance of health protocols, but high-risk businesses will remain closed until April 19. The Government will continue its activities with two-thirds of its personnel at work, and one-third will be allowed to work from home.”
Table 3 shows the participants’ characteristics and referral sites. The mean ± SD of their ages was 46.05 ± 16.5 years, and 56.9% were male. Of these patients, 259 (3.0%) died for different reasons including COVID-19, whereas 8171 (94.4%) recovered and were discharged. Most of the participants (8000 or 92.5%) attended the emergency department of the hospital. CKD, type 2 diabetes, cardiovascular diseases, and cancer were the most common underlying health conditions.
| Variables | Values |
|---|---|
| Age | 46.06 ± 16.5 (43) |
| Days of hospitalization | 2.29 ± 4.7 (0) |
| Sex | |
| Female | 3727 (43.1) |
| Male | 4920 (56.9) |
| Referral site | |
| Emergency department | 8000 (92.5) |
| Medical ward | 561 (6.4) |
| Intensive Care Unit | 73 (0.8) |
| Outcome | |
| Recovery and discharge | 8171 (94.4) |
| Death | 259 (3.0) |
| Transfer to other centers | 12 (0.1) |
| Withdrawal of admission | 119 (1.4) |
| Leave with personal consent | 86 (1.0) |
| Underlying health conditions | |
| Chronic kidney disease (CKD) | 239 (2.8) |
| Type 2 diabetes | 141 (1.6) |
| Cardiovascular disease | 117 (1.4) |
| Cancer | 88 (1.0) |
| Type 1 diabetes | 35 (0.4) |
| Chronic obstructive pulmonary disease | 27 (0.3) |
| Hypertension | 24 (0.3) |
| Liver disease | 15 (0.2) |
| Brain stroke | 9 (0.1) |
| Asthma and pulmonary disease | 1 (0) |
a Values are expressed as mean ± SD or No. (%).
The participants’ chief complaints and accompanying symptoms at the time of admission are listed in Table 4. The most common accompanying symptoms were dyspnea, fever, cough, and myalgia.
| Clinical Symptoms and Signs | No. (%) |
|---|---|
| Dyspnea | 870 (10.1) |
| Fever | 613 (7.1) |
| Cough | 574 (6.6) |
| Myalgia | 415 (4.8) |
| Malaise and fatigue | 197 (2.3) |
| Acute respiratory distress syndrome (ARDS) | 91 (1.1) |
| Headache | 74 (0.9) |
| Gastroenteritis and colitis | 66 (0.8) |
| Septic shock | 50 (0.6) |
| Pharyngitis | 49 (0.6) |
| Nausea/vomiting | 45 (0.5) |
| Chest pain | 43 (0.5) |
| Pleural effusion | 39 (0.5) |
| Coma | 30 (0.3) |
| Chills | 24 (0.3) |
| Hemoptysis | 23 (0.3) |
| Dizziness | 14 (0.2) |
As shown in Figure 2, Google Internet searches for the term “COVID” peaked across the country from March 22 to April 5, 2020. Data from the Internet searches represent a normalized value for searching this term compared to all other Google searches all over the country.
5. Discussion
The present study aimed to show the pattern of referrals to IKHC due to concerns and symptoms of COVID- 19 from February 20 to June 4, 2020.
Due to the increasing number of COVID-19 cases and concerns about its spread throughout the country and the general public concern in this regard, the need to establish a 24-hour call center to answer questions and provide information in order to reduce concerns as well as prevent and combat the virus is inevitable. Undoubtedly, in this situation, the call center has a very prominent role in providing counseling and education, reducing the anxiety of coronavirus, resolving ambiguities, and quashing rumors by providing correct and scientific answers to people’s questions. As the results of the present study revealed, MoHME’s 4030 call centers (19) reduced the total number of referrals.
The second peak during March 12 - 18 indicated that the Government policies and media were not effective in informing people, and more restrictive policies were required. Accordingly, more restrictions on travel along with a gradual increase in business shutdowns were imposed, until March 26, 2020, when the National Committee for COVID-19 placed more restrictions to be executed until April 4, 2020.
Also, during this period, there was a surge in Google searches for the term COVID-19 in the week of March 22-28, 2020. There was a dramatic reduction in the referral of the COVID-19 negative group from March 19 to March 25 suggesting that the Government was successful in reducing unreasonable attendances by informing the community. On March 28, an increase was documented in the testing capacity as well as the number of authorized laboratories to conduct COVID-19 testing across the country (20). In general, 90 labs in the 31 provinces of the country were capable of conducting specific diagnostic tests every day, and therefore the referrals for performing diagnostic tests at IKHC decreased, the reason behind a reduction in both COVID-19 negative and positive groups in our study.
On April 4, 2020, the social distancing program was introduced by MoHME followed by smart social distancing resulting in a dramatic reduction in COVID-19 cases. The government announced that in the framework of the smart social distancing program, medium- and low-risk businesses across the country can start their activities from April 11 with strict observation of health protocols, but high-risk businesses would remain closed until April 19. In this framework, the elderly, as well as people with severe illnesses, were given priority and more attention. Government offices carried on their activities with two-thirds of their personnel at work in person.
In the present study, the number of men referring to IKHC was more than that of women, similar to a study conducted in Baqiyatallah Hospital in Tehran, Iran (21). Also, during the MERS-CoV and SARS-CoV epidemics, more men were affected than women (22, 23). This finding can be explained by the X chromosome and its role in the innate and adaptive immune system and the role of female sex hormones to make them less susceptible to infection (24).
There was a difference in the prevalence of underlying health conditions in patients of this study and the other study mentioned in the following paragraph. In the present study, CKD, diabetes (types 1 and 2), cardiovascular diseases, and cancers were more common, whereas in the study conducted by Nikpouraghdam et al. (21), diabetes, chronic respiratory diseases, hypertension, and cardiovascular diseases were more common.
Raoofi et al. (7) conducted a study and compared the policies and strategies of Iran with the experiences and recommendations of China and WHO to combat COVID-19. They concluded that effective control of COVID-19 depends on the extent of applying a whole-of-government and a whole-of-society approach in the formulation, implementation, and evaluation of the policies involved. Tabari et al. (18) reviewed the public health responses to the COVID-19 epidemic in some countries including China, Italy, Iran, Spain, South Korea, Germany, France, United States, Australia, Canada, Japan, and Singapore. They concluded that quarantine, social isolation, and flight suspensions can be useful and effective techniques to control and confront the present pandemic.
Pan et al. (25) conducted a study and examined the association of public health interventions with the epidemiological features of the COVID-19 outbreak in Wuhan, China. In contrast to our results, they found that, compared with males, females had a higher rate of confirmed cases. Moreover, they concluded that mitigation measures, such as traffic restriction, cancellation of social gatherings, and home quarantine were associated with a reduction in the degree of transmission.
Based on the findings, the increase in respiratory emergency referral could be attributed primarily to older individuals. The results of this study showed that those referring to the hospital due to COVID-19 were middle-aged and had chronic conditions such as CKD, diabetes, and cardiovascular disease. The reason behind the referral of these groups to the hospital and emergency departments may be a reflection of the age of the first cases reported to have died of COVID-19 in Wuhan, China (26). In a similar vein, McDonnell et al. (27) conducted a study to examine the effect of H1N1 influenza on referring to an emergency department. They found more referrals to emergency departments among young children, which may be attributed to the age of the first patient (a 22-month-old) reported to have died of H1N1 in the United States.
There was a great concern among people due to the lack of information and also lack of reliable sources. During the first weeks of the pandemic, there were no reliable sources of news, and many people followed the news from Google or social media such as Instagram, Twitter, and Telegram, which are presumptively impregnated with rumors and fake news, confusing the community and thus increasing the fear.
There is no doubt that providing reliable news media has a crucial role in informing the community of potential health threats. However, news coverage may have the potential to harm public health and welfare, when such coverage, independent of actual disease prevalence, overcrowds the emergency departments. Therefore, news media and the government, in general, should be aware of this potential impact and take appropriate precautions to ensure that their coverage of public health issues establishes an authentic and credible authority without harming public health. In this situation, health policymakers should develop effective educational programs with careful and timely planning to help people gain the necessary knowledge of the situation and behave rationally and appropriately to maintain their health in an effective yet non-threatening manner. Garfin et al. (9) carried out a review and suggested that repeated media exposure to a crisis such as COVID-19 can result in increased anxiety, heightened stress responses, can have downstream effects on health, and increase inappropriate health-protective and help-seeking behaviors, which is in agreement with the results of this study.
Our study examined the trend of IKHC referrals and the Iranian government’s policies during the first peak (from February 20 to June 4). Yet, the referral patterns, government policies, and public behaviors were different in other peaks which were not examined in this study. Also, the present study used the hospital’s electronic database and the accuracy could have been higher if the data had been extracted directly from each patient’s file. Additionally, we had to include limited variables in our study since the data available to us in the database were not comprehensive. It was not possible for the researchers to obtain written informed consent from all the participants because the data had already been recorded, and it was a retrospective cohort study. However, a deliberate effort was made throughout the study to ensure that all aspects of medical ethics, including the confidentiality of individuals’ names, were observed, and no harm was done to the patients.
5.1. Conclusions
Public fears of COVID-19 were associated with increased referrals to hospitals, which were mostly unreasonable. This pattern was mostly associated with old age and chronic conditions, which can be a reflection of the impact of the first cases of death due to COVID-19. The referral pattern during the outbreak emphasized the role and influence of news media and government policies on public health threats. The findings showed that restrictions, quarantine, people’s cooperation, and informing and educating the public were of considerable importance in decreasing the number of people referring to hospitals and healthcare centers in both negative and positive COVID-19 cases. Therefore, to achieve the best results, the government and media should cooperate to take appropriate precautions, and at the same time, effective policies should be adopted so that people can gain the necessary and trustworthy knowledge of the situation.