1. Backgound
The prevalence of food allergies has increased in recent decades. Since many factors, including patients’ age and genetics, environmental conditions, and dietary exposure may affect the prevalence of food allergy, accurate determination varies among nations. Due to the lack of understanding of food allergy by patients, it is quite difficult to estimate its prevalence. However, World Allergy Organization has estimated that food allergy affects 2.5% of the general population (1). In addition, using standard tests, Cianferoni estimated that food allergy is common in 8% of young children and 4% of adults (2). Food allergy is used when a causal relationship occurs between a specific immunological mechanism and a specific food consumed, falling into three broad categories of immune reactions, including IgE-mediated, non-IgE-mediated and mixed. Other reactions without an immunologic basis are defined as food intolerances. IgE-mediated food allergies are usually rapid-onset in different organs, including skin (urticaria, angioedema, pruritus), gastrointestinal tract (nausea, abdominal cramp, vomiting, and diarrhea), respiratory tract (rhinoconjunctivitis, asthma), and oral allergy syndrome, and anaphylaxis. As a result, IgE-mediated food allergies can sometimes result in death. A pathophysiological mechanism explains the whole process of the disease in IgE-mediated food allergies (3). In contrast, non-IgE-mediated and mixed types of food allergies are linked to manifestations of delayed hypersensitivity reactions, including gastrointestinal (eosinophilic esophagitis, eosinophilic gastroenteritis, food protein-induced enteropathy, and food protein-induced allergic proctocolitis), pulmonary (asthma, Heiner’s syndrome), and cutaneous manifestations (eczema). Although these disorders may not cause mortality, they can lead to significant morbidity (3).
2. Objectives
This study aimed to compare the various types of food allergies in children and discuss the basis of their different presentations.
3. Methods
3.1. Study Design
3.1.1. Patient Selection
This study was conducted on children aged 2 - 12 years old with signs or symptoms of food allergy in the allergy clinics of Azad University Hospitals, Tehran, Iran, from January 2019 to January 2020. Food allergy was evaluated in these patients by careful history, physical exam, as well as skin prick and atopy patch tests.
3.1.2. Definitions
Food allergy: Reproducible and adverse health reactions after exposure to a specific food mediated by immunologic mechanisms (4).
Skin prick test (SPT): A reliable and widely used method to demonstrate IgE-mediated allergic reactions.
Atopy patch test (APT): Epicutaneous application of intact protein allergens in a diagnostic patch test setting along with evaluating the induced skin lesions after 48 and 72 hours (5).
IgE-mediated food allergy major presentations: Rash, urticaria/angioedema, pruritus, sneezing, coughing, wheezing, hoarseness, cardiovascular/neurological manifestations, loss of bladder control.
Non-IgE-mediated food allergy major presentations: Emesis, diarrhea, bloody stools, edema, shock, failure to thrive, lethargy, and pallor (6).
3.1.3. Inclusion and Exclusion Criteria
The inclusion criteria were children from 2 to 12 years old with signs or symptoms suggestive of food allergy. The exclusion criteria were those younger than 2, older than 12, or unwilling to participate in this study.
3.2. Initial Assessment
The children were categorized into two distinct groups according to their food allergy manifestations, IgE-mediated as the first group and non-IgE mediated as the second. Then, the subjects were evaluated using the SPT (Greer Company, USA) and APT for common food allergens mainly based on their cardinal manifestations. Atopy patch and skin prick tests were performed by the same nurse according to standard protocols at least five days after discontinuing all antihistamine-containing medications.
3.3. Statistical Analysis
The data were analyzed using SPSS Software Version 26 (IBM Corp. Armonk, NY). Quantitative parameters were described according to mean ± standard deviations, and qualitative data were obtained by the chi-square test and Fisher’s exact test. Other statistical tests used in this study were the Mann-Whitney U test, Pearson, and Spearman correlation test. A P value of less than 0.05 was considered significant.
3.4. Ethics
The present study was carried out under the recommendations of the Ethics Committee of the Islamic Azad University of Medical Sciences, Tehran, Iran. Informed written consent was taken from all patients’ caregivers. The study protocol was approved by the Ethics Committee of Islamic Azad University of Medical Sciences, Tehran, Iran, with the reference code of IR. IAU.TMU.REC.1399.367.
4. Results
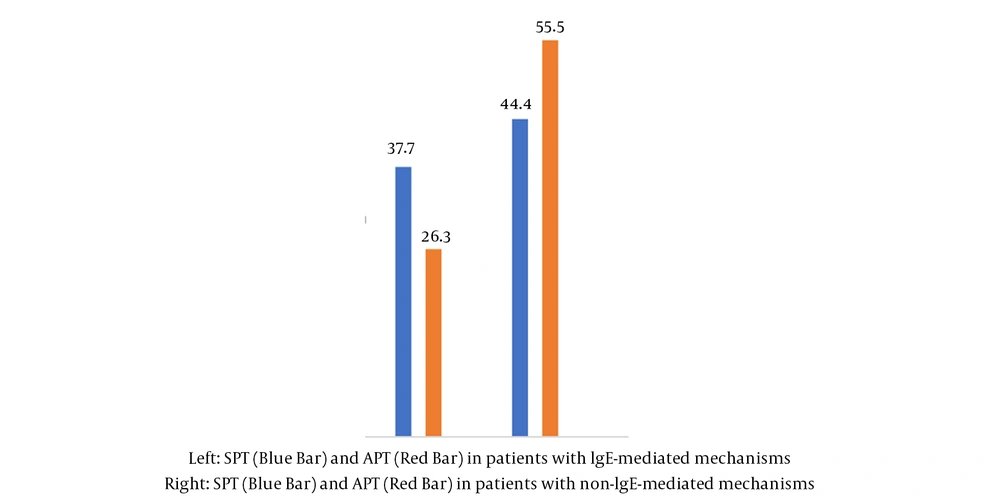
A total of 131 children between the ages of 2 and 12 with signs or symptoms of food allergy who were referred to Azad University Hospitals' allergy clinics were analyzed between January 2019 and January 2020. The mean age of the patients was 3.17 years, with a standard deviation of 3.45. The study included 78 (59.5%) female patients and 53 (40.5%) male patients. A positive family history of atopy existed in their first-degree relatives in 82 patients (63%). All the children were exclusively breastfed at the beginning. A total of 61 patients had positive skin prick tests, while 70 patients had negative results. In addition, 68 patients had positive atopy patch tests, and 63 had negative results. Figure 1 presents the results of the skin prick and atopy patch tests in the two groups of patients with IgE-mediated and those with non-IgE reactions or mixed types.
Table 1 compares the mean age of the patients with positive SPT and APT test results.
| Skin Prick Test | Atopy Patch Test | |
|---|---|---|
| Patients | 61 | 68 |
| Mean age | 4.21 | 2.24 |
| Standard deviation | 4.34 | 2.1 |
| P value | 0.001 | 0.001 |
There was a significant correlation between a positive atopy patch test and proctocolitis (P value = 0.001) in the studied children. A significant correlation (P value = 0.001) was also observed between the positive skin prick test and anaphylaxis, rash, pruritus, and hives. No significant correlation was detected among the SPT and APT test results with atopic dermatitis, gastroesophageal reflux disorder, or other gastrointestinal manifestations.
Table 2 compares SPT and APT test results in different food allergens consumed by the studied children.
| Food Allergen | Skin Prick Test Positive | Atopy Patch Test Positive |
|---|---|---|
| Cow’s milk | 26 (34.2) | 49 (64.5) |
| Egg | 35 (46.1) | 41 (53.9) |
| Wheat | 8 (88.9) | 2 (22.2) |
| Nuts (walnut, almond) | 11 (64.7) | 7 (41.1) |
| Soy | 2 (100) | 1 (50) |
| Sesame | 6 (66.7) | 3 (33.3) |
| Rice | 1 (100) | 0 (0) |
| Beef | 8 (100) | 0 (0) |
| Seafood (fish, shrimp) | 5 (62.5) | 3 (37.5) |
a Values are expressed as No. (%).
A significant correlation was detected between positive atopy patch test results and hypersensitivity reactions to cow’s milk (P value = 0.001), beef (0.002), and tomato (0.04) among food allergens. The analysis also showed the same significant correlation between positive skin prick test results, allergens, and wheat (P value = 0.01).
5. Discussion
Food allergy reactions are mediated by IgE- or non-IgE-mediated mechanisms (4) with an increasingly recognized spectrum of disorders because of their diverse and heterogeneous manifestations in different organs and their potential for significant morbidity (3). The most challenging food allergies to diagnose are non-IgE-mediated allergies, which are commonly misdiagnosed. The lack of a clear cause-effect relationship and appropriate non-invasive tests is another limitation that physicians face regarding non-IgE-mediated food allergies. Food allergies with non-IgE mediated symptoms are diagnosed clinically based on symptoms that improve after removing the culprit food (7). This study evaluated the children whose different organs, such as the skin or gastrointestinal tract, were adversely affected by food allergies. The patients were classified into IgE- and non-IgE-mediated food allergies according to the pathophysiologic mechanism of their specific food hypersensitivity.
Clinical manifestations of IgE-mediated food allergy in organ system include skin (rash, urticaria/angioedema, pruritus, oral allergy syndrome), upper airway (sneezing, itching), lower airway (wheezing, periods of airway clearing, cough, persistent throat tightness), gastrointestinal tract (nausea, vomiting, abdominal pain), cardiovascular/neurological (weakness, dizziness, tachycardia, drop in blood pressure, anxiety, confusion, unconsciousness), and others (loss of bladder control, pelvic pain) (8). As a result of the lack of accessible blood or skin tests, it is more difficult to confirm the relationship between the culprit food and the symptoms in non-IgE-mediated food allergies. Food protein-induced enterocolitis syndrome (a combination of emesis, diarrhea, poor growth, and lethargy), food protein-induced allergic proctocolitis (bloody stools in well-appearing infants), and contact dermatitis are some of the complications (1). Eosinophilic gastrointestinal disorders and atopic dermatitis may be characterized concurrently by both mechanisms. The patients were categorized according to their manifestations into two groups of patients with IgE-mediated and non-IgE-mediated manifestations, and then evaluated both by skin prick and atopy patch tests. Oral food challenge is the gold standard for diagnosis of IgE- and non-IgE-mediated food allergies (9), which was not performed due to the time required and the risk of severe reactions and relied on non-invasive procedures. All patients underwent both skin prick and atopy patch tests due to the overlap in symptoms between IgE- and non-IgE-mediated food allergies. The atopy patch test results were predominantly positive in non-IgE- mediated conditions, while the skin prick test results were significantly positive in those with IgE-mediated food allergies. Previously, the atopy patch test was shown as a reliable diagnostic tool in food allergy-related skin symptoms in young children (10). Atopy patch test with a specificity of 95% is considered a proper confirming tool in diagnostic work-up of food allergy, particularly in patients without positive specific IgE results and delayed reactions (11). A skin prick test with a negative predictive value of more than 90% and high sensitivity (12) helps confirm IgE-mediated food allergies, particularly in acute allergic events and aids in ruling out IgE-mediated food allergies when the skin prick test is negative.
Patients with positive atopy patch test results were younger than those with positive skin prick test results. Atopic sensitization, is defined as positive allergen-specific IgE, which is diagnosed either by skin prick test or in the patients’ sera and changes dynamically through childhood and increases with age (13). Allergic sensitization in infants initially occurs with food allergens and increase with age. Allergen sensitization tends to increase with aeroallergens after age 2 as well (14). The higher age of these patients can be explained with positive SPT results with this fact.
Aging would be associated with lower levels of sensitization after the age of 20 years, which might reflect immunosenescence (15).
Although breastfeeding has a protective role against food allergies, all patients participating in this study were exclusively breastfed without formula supplementation at the onset of their symptoms. Breast milk antigens may cause clinical reactions in previously-sensitized infants, including IgE-mediated and non-IgE-mediated food allergies (6).
Genetic predispositions to food allergies are another risk factor associated with the disorder. Evidence from two low-quality reviews shows that atopic disease or food allergy in parents or siblings may act as risk factors for developing food allergy in the next child (16).
Age and diet are the two major factors affecting allergic response to different food allergens (17). Most food reactions in children are caused by eight food types, including milk, eggs, peanuts, tree nuts, fish, shellfish, soy, and wheat. The primary culprit foods in this study were cow’s milk, egg, nuts, and wheat detected by SPT and APT tests. According to several studies published from 2002 to 2014, cow's milk and egg are the most common food allergens across the country (18, 19).
Based on the limitations of this study, no oral food challenges or elimination diets were performed to confirm the diagnosis of food allergy.
5.1. Conclusions
According to the results, food allergy is an increasingly primary health concern worldwide with cow’s milk and egg as the most common food allergens. Non-IgE-mediated and mixed food allergies arise through immunological mechanisms, which are not well understood yet. The SPT and APT tests may assist in identifying the culprit foods, but diagnosis relies on a compatible history and the resolution of symptoms after elimination diets are implemented. However, oral food challenges are still the mainstay of the diagnosis. Therefore, Atopy patch test results may be helpful but not convincing in all cases.