1. Background
The sphenoid bone (SB) is an essential bone of the skull base, which contains the sphenoid sinus (SS) and is closely related to the vital neurovascular structure (1). Sphenoid bone shape and size show significant individual variability, and SS may extend into the foramen magnum depending on the type of pneumatization. There is an extensive diversity in SS variants, which occur often (2). Sphenoid sinus pneumatization is significant when designing surgical approaches to intrasellar and extrasellar diseases because of its inherent relationship to the nasal cavity (3). The optic nerve (ON), cavernous sinus, internal carotid artery (ICA), and maxillary and cranial nerves III, IV, and VI are all near the sphenoid sinus's contents when it is overly pneumatized (4).
The middle cranial fossa contains the posterior clinoid process (PCP) and dorsum sella (DS), which produce light bony prominences with different degrees of pneumatization on the upper surface of the SB (5). Surgical access to diseases within the clivus or interpeduncular cisterna is linked to PCP and DS pneumatization. In addition, DS and PCP may obscure deeper anatomical structures, such as the basilar artery apex, creating a barrier (5, 6). Congdon initially characterized the pneumatization of the SS in 1920, referring to the sella tursica. In the sagittal plane, pneumatization was thus divided into three categories: Conchal, presellar, and sellar (7). Later, Hardy added a postsellar type to include more developed cases of pneumatization (8). The sellar type has been categorized into six fundamental forms (sphenoid body, lateral, clival, tiny wing, anterior, and combination) by Wang et al. in previous. This classification defines the postsellar type as clival as a subtype of the sellar type (9).
Computed tomography (CT) is a crucial diagnostic tool for anatomical differences when making therapeutic decisions on surgical treatments. Computed tomography scanning of the paranasal sinuses reveals significant findings about proper pneumatization processes within the sinus and neighboring bone marrow cavities (10). The significance of the paranasal sinus anatomy, particularly the SS, is growing due to advancements in imaging technology and the advent of functional endoscopic sinus surgery (FESS) (11).
In addition to using the pneumatized structures of the SB, surgeons can also explore areas such as the anterior cranial floor, the pericellular areas, the clivus and petroclival regions, and the cavernous sinuses with this approach (11, 12). In addition, new technological developments such as computer-assisted surgery (CAS) have provided significant advantages in guiding the endoscopic probe in FESS through automated robotic assist procedures (13). This technological advancement requires the preoperative definition of essential parameters in endoscope guidance. The intricate anatomical variations of the sphenoid sinuses may make navigation and orientation during endoscopic surgery more difficult (13, 14).
Examining the studies in the literature reveals that the prior classifications lacked several sections and that there is no consensus (7-9). Nonetheless, the Hardy technique is the most often utilized for DS and PCP pneumatization examination (8). There is little indication of a possible relationship between anatomical variants, especially for those involved in pneumatization structures other than the body (pterygoid processes, anterior clinoid processes, dorsum sellae) of the SB (10, 15-17). In addition, few articles have been published on SS pneumatization and its types in different populations (10, 18-22).
The detailed indication of SS and lateral-type pneumatization in the radiological evaluation before transsphenoidal surgery may change the operation plan (15).
2. Objectives
This study aims to classify pneumatizations of the SS and lateral types in detail with the most significant number of instances and use these classifications to ideally determine the incidence of pneumatization types in the Turkish population.
3. Methods
3.1. Participants and Study Design
The institutional ethics committee approved this retrospective study (IRB: 514/167/7). Computed tomography images obtained for the paranasal sinuses were evaluated retrospectively from March 2020 to February 2022. Informed consent was acquired from patients whose CT images were taken, and all pertinent principles of the Helsinki Declaration were followed. The exclusion criteria were cases with SS disease, intracranial tumors, craniofacial bone disorders, craniofacial syndromes/anomalies, cleft lip or palate, history of orthognathic surgery, images with > 2 mm section thickness, and cases with age < 18.
The investigation contained CT illustrations showing the sphenoid sinus's entire borders. Paranasal sinus CT scans of 509 patients compatible with the current criteria were determined and included in the study.
3.2. Imaging Acquisition
The same CT scanner (SOMATOM Definition Flash, Siemens Healthcare, Forchheim, Germany) captured all exam images. The acquisition parameters were reconstruction thickness: 0.625 mm, collimation: 40 × 0.5 mm, tube rotation: 1 s, and kV: 130. Axial scans were taken from the maxillary sinus floor to the frontal sinus roof level in a plane parallel to the hard palate. Different window widths and levels were examined at the workplace. SS was assessed in the coronal, sagittal, and axial planes for every patient.
3.3. Classifications of the Sphenoid Sinus
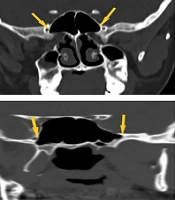
Pneumatizations have been separated into posteroanterior (PA) and lateral directions. Four subtypes of PA pneumatization were identified (Figure 1):
- Conchal type: The sinus is absent or very slightly extended.
- Presellar type: The anterior wall of the sella turcica is in advance of the posterior border of the SS.
- Sellar type: The sinus is situated between the sella's anterior and posterior walls.
- Postsellar: The sinus's rear wall extends past the sella's posterior border.
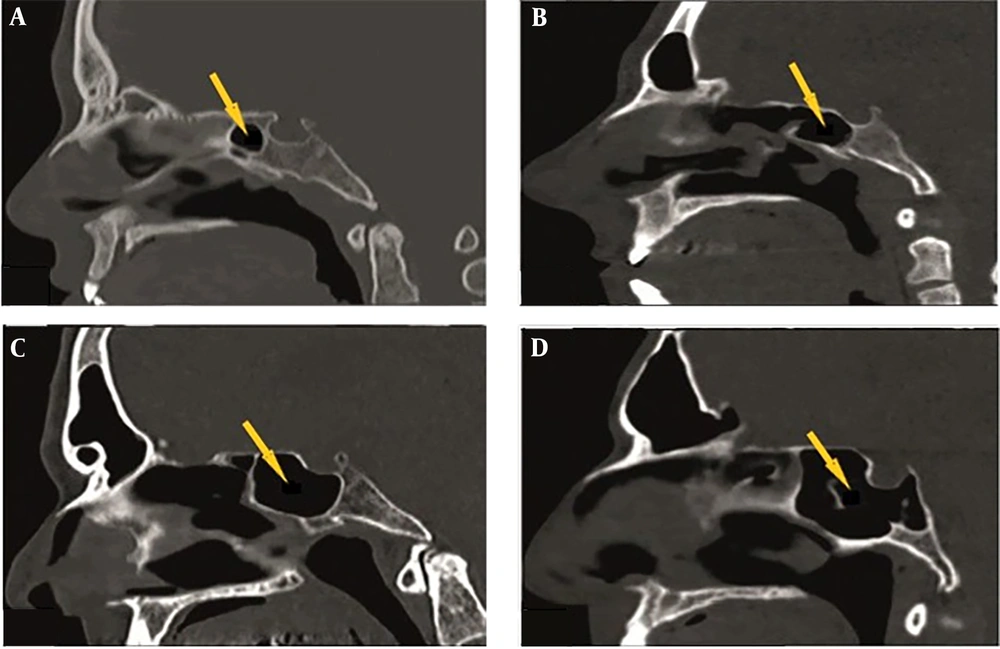
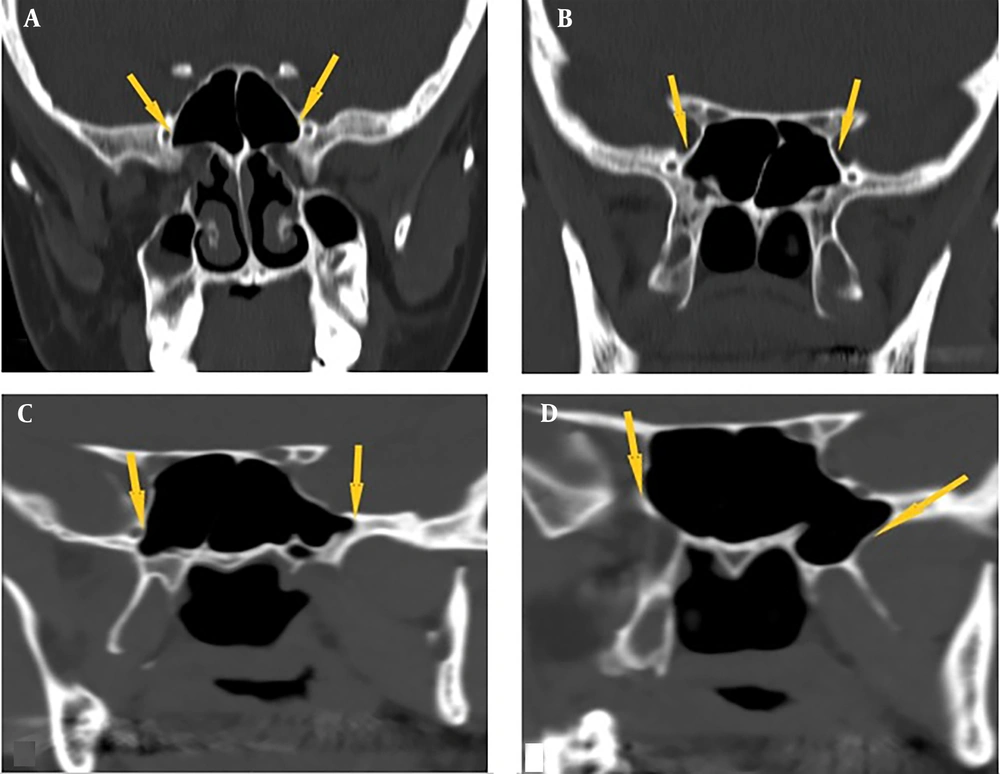
Four subtypes of the SS were assessed for lateral pneumatization: Body, lesser wing, inferior, and combined (lesser wing-inferior). As mentioned in the literature, the optic canal and the virtual reality (VR) line connecting the foramen rotundum and the vidian canal were also used as guides for these pneumatizations (4, 9). Lesser wing-type pneumatization was defined as that which went from the optic canal to the anterior clinoid process. In contrast, inferior-type pneumatization was defined as beyond the VR line. Pneumatization inside guide regions was categorized as lateral body type, and pneumatization outside both guide areas was classified as combined type (Figure 2).
SPSS software version 18 was used for statistical analysis (Chicago, IL, US). Central tendency was expressed using descriptive statistical techniques [median, mean, frequency, standard deviation (SD), minimum, and maximum]. The distribution of the quantitative data was examined for normality using the Kolmogorov-Smirnov test. The statistical difference between categorical data was assessed using Pearson's chi-square test. Mann-Whitney U test was utilized to compare the laterality and sex differences. A 95% confidence level was considered for all analyses, and a P-value < 0.05 was deemed statistically significant.
4. Results
The study comprised 509 patients; 255 (or 50.1%) male and 254 (or 49.9%) female. Both cases were male, with the youngest being 18 and the oldest being 89. The oldest female instance was 81 years old, and the youngest was 19. The mean age ± SD was 48.02 ± 17.34, and the median was 47 (Table 1).
| Variables | n | Mean ± SD | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| Female | 254 | 48.17 ± 16.8 | 48 | 19 | 81 |
| Male | 255 | 47.87 ± 17.9 | 47 | 18 | 89 |
| Total | 509 | 48.02 ± 17.34 | 47 | 18 | 89 |
Abbreviation: SD, standard deviation.
When the PA pneumatization of 509 patients was evaluated, 0.6% conchal, 16.7% presellar, 66.4% sellar, and 16.3% postsellar pneumatization were detected. The conchal type was the least common, with three female cases (Table 2). There was no significant correlation (P = 0.354) between the SS type and gender when the relationship was examined.
| Types | Male | Female | Total |
|---|---|---|---|
| Conchal | 0 (0) | 3 (0.6) | 3 (0.6) |
| Presellar | 46 (9) | 39 (7.7) | 85 (16.7) |
| Sellar | 163 (32.1) | 175 (34.3) | 338 (66.4) |
| Postsellar | 46 (9) | 37 (7.3) | 83 (16.3) |
| Total | 255 (50.1) | 254 (49.9) | 509 (100) |
a Values are expressed as No. (%).
The most prevalent lateral direction pneumatizations were left lateral body (32.2%) and right lateral body (39.9%). Lesser wing was the least common lateral type (3.9%) (Table 3). No statistical significance was found between sphenoid lateral type pneumatization and gender (P = 0.388). In addition, the relationship between age-sex, age-sphenoid sinus type, and age-lateral type pneumatization was compared, and (P = 0.905, P = 0.247, and P = 0.434) no statistically significant difference was noticed.
| Types | No. (%) |
|---|---|
| Right lateral body | 203 (39.9) |
| Left lateral body | 164 (32.2) |
| Lesser wing | 20 (3.9) |
| Inferior | 41 (8.1) |
| Combined | 81 (15.9) |
| Total | 509 (100) |
5. Discussion
The SS varied considerably based on its extensions outside the body of the SB (14). Aside from being close to several surrounding structures, such as the internal carotid arteries, the cavernous sinuses, the optic, vidian, maxillary, oculomotor, and trochlear nerves, this is an essential factor to know in pituitary surgery (9).
Accidental cerebrospinal fluid leakage can occur from damage to the sphenoid sinus's lateral, posterior, or superior walls (23, 24). Sphenoid sinus began to form from the nasal capsule of the embryonic nose in the fourth month of fetal development, and its pneumatization progressed with age and took its final form during puberty (3, 25).
Treatment for intrasellar lesions typically involves transsphenoidal surgery. Research has demonstrated that the transsphenoidal method reduces morbidity and mortality rates when juxtaposed with the transcranial method (9, 26). The SS creates a pathway for the endoscope to reach intrasellar pathologies because of the anatomical connection between the SS and the nasal cavity. Additionally, SS pneumatization can access additional areas of the skull base (23). The type and degree of pneumatization of the SS play a crucial role in surgical planning. There should be a comprehensive understanding of the anatomical variations of the SS to prevent iatrogenic injury and comprehend the illnesses that arise in this area (16).
In Gibelli et al., sellar-type SS pneumatization was observed most frequently, at 74%. Sphenoid sinus volume was also measured, and men had higher mean SS volume than women. As a result of evaluating the SS types, the presellar type had the lowest volume, while the retrosellar type had the highest (16). Movahhedian et al. encountered the most common postsellar and sellar types in 500 patients. Onodi cell frequency and the relationship between ICA and ON of the SS were also evaluated. As the pneumatization of the SS increased, ON and ICA caused an increase in the frequency of protrusion and dehiscence. ON dehiscence and the existence of Onodi cells were significantly correlated with a 38.8% prevalence of Onodi cells (27).
Degaga et al. evaluated SS pneumatization in 200 patients in the Ethiopian population. The sellar type was, therefore, the most prevalent (50%), and the reseller type was the second (25.5%). There were four categories for SS septation: Single complete, single incomplete, double septa, and absence of septa. The most common septation was single complete, occurring in 77.5% of cases. Sellar pneumatization was the most clinically significant anatomical variation among the Ethiopian participants in the study, and 90% showed single septation on CT (10). In another study by Elkammash et al., the most common sellar type (85.7%) SS pneumatization was observed. Sellar septums have been reclassified within themselves, with inter-sphenoid septums being the most common and multiple sphenoid septums being the least common (24).
Ilkow et al. assessed the pneumatization of 100 patients' PCP, DS, and SS using CT. The Hardy classification divided the post-sellar type into IVA and IVB based on the pneumatization of the dorsum sella and posterior clinoid process. Three sagittal planes were used for the analyses: The midline plane (MP), the sagittal posterior left clinoid plane (SPCP-L), and the sagittal posterior right clinoid plane (SPCP-R). Sellar-type pneumatization was most common in MP and SPCP-R (41% and 38%, respectively), and type IVA pneumatization was most common in SPCP-L (41%). Type IVB was detected in 12% of SPCP-R visuals, 10% of SPCP-L images, and 12% of MP images (17). Bilgir and Bayrakdar evaluated SS pneumatization with CT in 128 patients. According to the PA classification, postsellar (57.8%) and sellar type (35.9%) SS pneumatizations were the most common types. Sphenoid sinus pneumatization was also evaluated in the lateral direction with a new classification. Subtypes were lateral body, lesser wing, inferior, and combined (lesser wing-inferior). The evaluation of pneumatizations in the lateral direction revealed that the lateral body type was most prevalent on the left (42.5%) and right (44.1%) sides (15).
Similar to the present study, the sellar type is the most common in a few studies, but its percentages (50% - 85.7%) are higher (10, 24). The number of cases in Degaga et al. was relatively small at 200, and that they were from a different race may have caused this result (10). In the other study, it was thought that the percentage of the sellar type was probably much higher because the postsellar type was not specified and was only divided into three subtypes: Conchal, presellar, and sellar (24). In the study of Movahhedian et al., the postsellar type (52%) was more common than the sellar type (35.5%), although the number of cases was similar to ours. The fact that there was a different population and the number of female cases (297) was much higher may have caused this difference (27). In the previous two studies in which the lateral parts of the SS were evaluated in addition to PA pneumatization, the insufficient number of cases (100 - 128 cases) may have probably caused the postsellar type, which was relatively more frequent (15, 17).
This study has some remarkable advantages compared to other studies. This study has the most significant cases (509) obtained using CT for SS pneumatization (10, 15-17, 27). Similarly, the Turkish population study has the most significant case reported in the literature on SS pneumatization. It is also the second CT study using lateral direction classification (15). Thus, as much data as possible was evaluated.
5.1. Limitations
There were a few limitations in the present study. Firstly, there were few CT studies with which we can compare PA pneumatization (10, 15-17, 20, 24, 26, 27). Secondly, there was only one CT study in the literature for the lateral direction (15). Finally, this study's lack of volumetric measurement for SS could be another limitation (16).
5.2. Conclusions
At the base of the skull, the sphenoid bone holds the greatest significance, and SS pneumatization shows considerable individual variability. A clear evaluation of PA pneumatization with CT is useful and instructive before transsphenoidal intervention. Lateral direction evaluation for SS is still new, and CT studies with many cases are needed.