1. Background
Coronary heart disease (CHD) is more prevalent among cardiovascular diseases (1) worldwide, especially in the Iranian population. In addition, CHD has been one of the first significant causes of death in recent years (2).
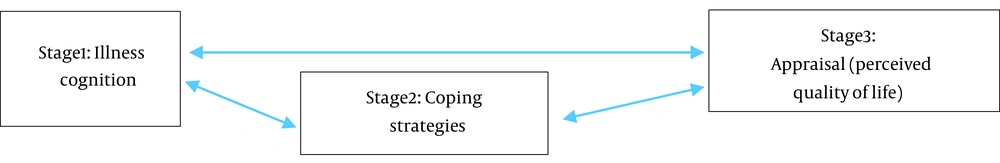
Psychological factors, including coping strategies, behaviors, quality of life, adherence, and illness beliefs, can affect illness onset, adaptation, and outcome in patients with CHD (3). When individuals consider healthiness a normal state, the onset of diseases like CHD will be regarded as a problem. Thus, individuals deal with their illnesses like other problems. Based on problem-solving approaches, the self-regulation model (SRM) of illness behavior (Figure 1) was developed to evaluate the coping (4). According to SRM, when people become sick, they experience anxiety, depression, and fear in addition to trying to understand their illness. The belief that a patient implicitly holds about their illness is called illness cognition. These beliefs help the patient generate a concept to understand and cope with diseases such as CHD. Illness cognition includes five dimensions: Identity (the label of the disease and the symptoms experienced), perceived causes (psychosocial or biological), timeline (perceived duration of the disease such as chronic or acute), consequences (psychosocial implications of the disease on the quality of personal and family life), curability and controllability (a patient’s beliefs about treatability or controllability of their disease) (5).
Leventhal’s self-regulation model (SRM) (3)
Researchers have suggested that from patients’ point of view, the most crucial factor leading to CHD is behavioral risk factors. They also stated that the psychological, biological, and environmental factors mentioned are the other important risk factors (6), and those concepts have been related to the current mood of the patient and their report of stressful lives (7). Both the interpretation of the disease and the illness cognition naturally lead to some emotional feelings in patients. Then, the excitement caused by the illness causes them to react to the disease. According to Leventhal's SRM, understanding the illness cognitions predict people’s coping strategies, and coping strategies can help determine the disease’s outcome (5). Coronary patients perceive their illness as chronic, with more symptoms, low levels of disease information, and serious negative consequences (8). Beliefs and perceptions of the patients about their chronic disease can impact adherence to medical recommendations through mediating role of coping strategies and emotional response (9). A systematic meta-analysis revealed that self-regulation mechanisms like cognitive bias, frequency of self-monitoring, and self-efficacy could alter health behaviors (10) so that self-monitoring provides improved diet, healthful physical activity, hypertension control, and medication adherence (11). Patients with CHD perceive all these factors as essential to their quality of life. Perceived quality of life is one of the most critical health concepts that assess the overall effect of a disease on a patient's life (12). Studies indicated that CHD significantly negatively impacts the quality of a patient’s life (13). Therefore, it is necessary to assess the relationship between quality of life with illness cognition and coping strategies to evaluate the impact of coping strategies on the patient's life.
2. Objectives
This study aimed to investigate the evaluation of Leventhal's self-regulation model in the quality of life of people with CHD. The central hypothesis of this study is to evaluate the relationship between illness perception, coping strategies, and perceived quality of life.
3. Methods
3.1. Participants
In total, 300 individuals with coronary heart disease were selected (14) using the convenience method.
3.2. Procedures and Data Collection
This cross-sectional correlational study was performed in Sari, Mazandaran, Iran, in 2018. The data were collected from the specialized heart clinics affiliated with Mazandaran University of Medical Sciences.
3.3. Data Analysis
Statistical analysis was performed using descriptive and inferential statistics using LISREL's structural equation modeling (path analysis), with parameters estimated using maximum likelihood estimation (MLE) (P < 0.05, P < 0.01).
3.4. Instruments
The study was conducted using four self-report questionnaires: (1) a demographic questionnaire, (2) the brief illness perception questionnaire (B-IPQ), (3) the coping schemas inventory (CSI), and (4) a researcher-designed perceived quality of life questionnaire.
Demographic questionnaire: Includes data about age, sex, job, educational background, and marital status.
The brief illness perception questionnaire (B-IPQ) was designed by Broadbent et al.. The questionnaire assesses the five cognitive illness dimensions in such a way that the first five items assess identity, timeline, personal control, treatment control, and consequences. The following two items assess concern and emotions, and a final article discusses the comprehensibility of illness. A nine-item scale is used based on a response rate on a scale from 0 (never feel threatened) to 10 (always or severely feel threatened) for items 1, 2, 5, 6, and 8 and add them to the reversed score for items 3, 4, and 7. The ninth item is an open-ended question about the perceived causes of CHD. Cronbach's alpha (0.90) for the total score indicated excellent internal consistency reliability, and the construct validity (0.52), concurrent validity (0.33), test–retest reliability (ICC: 0.90), appropriate predictive validity (0.44) (15, 16) were acceptable.
The coping schemas inventory (CSI): It was designed by Wong et al. to record different types of coping in the participants’ responses (17). This questionnaire has 78 items and eight sub-scales (8 items in each subscale). The choices ranged in a four-point Likert from strongly agree (5) to never agree (1) (18). The coping schemas inventory is explained by only six sub-scales in the Iranian population: Situational schemes, social support, religious beliefs, and emotional passivity. The Cronbach’s alpha value was calculated between 0.72 and 0.98, and the Cronbach's alpha of the total number of questions was 0.85, indicating high levels of internal consistency for its sub-scales (19). The test–retest reliability value was 0.69 to 0.94.
A researcher-designed quality of life Scale (The perceived Quality of life Scale) includes three items used to record the quality of life in three areas based on the World Health Organization Questionnaire (1993): Physical, mental, and general. The score of the items is based on the Likert range from strongly agree (5) to never to agree (1).
The study was conducted on 300 individuals who filled out the main questionnaires with CHD to determine psychometric indices. In B-IPQ, the distribution of the items was normal. Items 3 and 4 (related to control) were not accepted in single factor analysis. The six approved items could explain 34.12% of the variance in illness cognition. The questionnaire reliability was calculated at 0.69 by Cronbach’s alpha, which is acceptable. In the CSI-short form, the most critical factors, according to factor analysis in previous research (19), were selected because of the significant number of items in Iranian forms of coping schemas from each of the six sub-schema, which eventually reduced the number of items to 12 items. Data analysis indicated that items related to religious coping strategies had to be removed because of the lack of normal distribution, and items related to emotional passivity had to be removed due to a lack of factor loading. Overall, at this scale, one factor was extracted, and the remaining eight items could explain 26.50% of the variance. The reliability of the questionnaire using Cronbach's alpha was calculated at 0.73, which is acceptable. In the perceived quality of life Scale, the analysis of the item’s distribution revealed the normal distribution of all three questions. The internal reliability of the questionnaire using Cronbach's alpha was calculated at 0.78, which is acceptable. Test–retest reliability value was 0.80.
3.5. Ethical Considerations
Before data collection, the patients were informed about the study’s aims and process. There was no obligation for research participants, and they were also informed that they could leave the data collection process at any time.
4. Results
The study was performed on 300 patients aged between 30 to 65. The sample included 60.3% male and 39.7% female, and 91.3% of the participants were (91.3%) married. Further, 40.3% of research participants had secondary education. Each patient was asked about three perceived causes of CHD (Table 1).
| Perceived Causal | Behavioral | Psychological | Socioeconomical | Biological | Chance | Unknown |
|---|---|---|---|---|---|---|
| Frequency | 44 | 160 | 113 | 103 | 2 | 178 |
| Percentage | 7.3 | 26.7 | 12.5 | 17.2 | 0.3 | 29.7 |
From Table 1, most patients (29.7%) did not know the causes of CHD incidence, and only 7.3% of patients mentioned behavioral factors were the leading causes of their diseases.
The sufficiency index of sampling (KMO) was calculated at 0.795, which is acceptable. Bartlett's test of sphericity was rejected, and there was no missing data. The Kurtosis and skewness and Kolmogorov-Smirnov test had a normal distribution with no outlier.
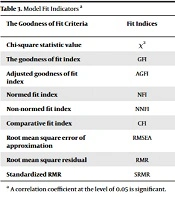
According to Table 2, coping strategies and illness cognition significantly correlate with perceived quality of life and have a significant relationship with illness perceptions. (Table 3)
| The Goodness of Fit Criteria | Fit Indices | The Goodness of Fit Values Obtained | Goodness of Fit | Fit Situations |
|---|---|---|---|---|
| Chi-square statistic value | χ2 | 4.80 | 0.00 ≤ χ2 ≤ 5.991 | Significant |
| The goodness of fit index | GFI | 0.97 | 0.95 ≤ GFI ≤ 1.00 | Good |
| Adjusted goodness of fit index | AGFI | 0.96 | 0.95 ≤ AGFI ≤ 1.00 | Good |
| Normed fit index | NFI | 0.91 | 0.95 ≤ NFI≤ 1.00 | Acceptable |
| Non-normed fit index | NNFI | 1 | 0.95 ≤ NNFI≤ 1.00 | Good |
| Comparative fit index | CFI | 1 | 0.95 ≤ CFI≤ 1.00 | Good |
| Root mean square error of approximation | RMSEA | 0 | 0.00 ≤ RMSEA ≤ 0.05 | Good |
| Root mean square residual | RMR | 0.043 | 0.00 ≤ RMSR ≤ 0.05 | Good |
| Standardized RMR | SRMR | 0.044 | 0.00 ≤ SRMR ≤ 0.05 | Good |
a A correlation coefficient at the level of 0.05 is significant.
According to Table 4, coping strategies directly affect the perceived quality of life (β = 0.12, P < 0.05). In addition, illness cognition has both direct effects on coping strategies (β = 0.10, P < 0.05) and indirect impacts on the perceived quality of life (β = 0.08, P < 0.05) through mediating role of managing processes. According to the results, the study's central hypothesis was significantly approved at P < 0.05. Therefore, SRMI can predict the perceived quality of life using illness cognition and adaptive coping strategies in patients with CHD.
| Paths | Path type | B | SE | Β | P | R2 |
|---|---|---|---|---|---|---|
| Coping strategies to quality of life | Direct | 0.22 | 0.04 | 0.12 | 0.01 | 0.10 |
| Illness cognition to coping strategies | Direct | 0.15 | 0.07 | 0.10 | 0.03 | - |
| Illness cognition to quality of life | Indirect | 0.12 | 0.20 | 0.08 | 0.02 | - |
| Illness cognition to quality of life | Total | 0.27 | 0.13 | 0.18 | 0.04 | 0.27 |
a A correlation coefficient at the level of 0.05 is significant.
5. Discussion
Perceived quality of life is mainly affected by various variables that significantly play direct roles in coping strategies. Adaptive coping systems have the most crucial role in predicting patients’ perceived quality of life with CHD. The coping strategies, including statements with situational coping strategies, coping by using social support, acceptance, and active emotional expression, were evaluated in this research. Individuals with a high score on these items have used more adaptive coping strategies. Adaptive coping strategies can predict the perceived quality of life. Predictably, people with more adaptive coping strategies have a higher perceived quality of life. According to scientific data, adaptive coping strategies reduce stress and anxiety (20). Researchers have indicated that patients with CHD mainly use emotional coping strategies (21). In addition, avoidance of coping strategies has been associated with an enhanced risk of mortality from CHD, and orientation coping strategies, such as actively dealing with stressful events, have been associated with a significant reduction in the incidence of stroke and cardiovascular mortality (22).
In this study, Illness cognition is another important variable for predicting the perceived quality of life in patients with CHD. Data are compatible with the Leventhal self-regulating model. Moreover, illness perception can impact adherence to a medical recommendation through coping behaviors and emotional responses (10). As a result, the self-regulation model of illness can be considered a critical mechanism for health-related behavior change that enhances the quality of life in patients. Based on the self-regulation model of Leventhal, when individuals realize the sick, they try to understand their disease, leading to "illness cognition" (4). Thus, many individuals experience signs or symptoms of the disease, believing their disease will take much time and have negative effects on their lives; they also thought their disease is not curable and controllable, which is why the illness cognition was able to predict adaptive coping strategies. A previous study revealed that CHD patients considered their illness chronic with more symptoms and severe negative consequences (8).
Most individuals claimed that controlling the disease was not their responsibility and was God's responsibility. The items related to coping by using religion were removed from the psychometric analysis of the scale of coping strategies because most of the patients in such items had acquired the top score. The high scores in items of this subscale confirmed the patients’ beliefs about the controllability of their disease. They believe everything is based on God’s control and willingness, and whatever God wants will happen.
Past research in other countries has mentioned that individuals with CHD believe that the leading causes of their disease are behavioral risk factors and psychological, biological, and environmental risk factors (6). Both women and men mentioned stress as the leading risk factor for CHD, and this attitude was related to the reports of their stressful life events and the current mood of the patients (7). The other study mentioned that spiritual experience and the cultural norms of some individuals with CHD, like beliefs about wellness or illness, are dramatically associated with God, which could impact their disease's controllability (8).
Based on the results, CHD patients had a primary need for information about their illness to adapt to their new situation (8). Patients should be informed about adaptive coping strategies, such as using situational coping strategies, social support, acceptance, and active emotional expression coping.