1. Introduction
Lateral luxation describes tooth displacement in any direction other than axial (1). The prognosis of luxated teeth depends on the emergency treatment and elapsed time (2). Intrusion is the most severe traumatic dental injury (TDI), corresponding to only 0.5 - 2% of all traumatic injuries in permanent teeth and 5 - 12% of dental luxation injuries (3). In addition, intrusion affects mainly the upper central incisors, followed by the upper lateral incisors, and rarely occurs in the mandible teeth (4).
The prognosis of intruded teeth is very low due to severe injury in the pulp and periodontal ligament. Lateral luxation is another TDI that causes damage to the root surfaces with a similar result in intrusion (5).
The intruded tooth is driven more axially into the socket, compressing the periodontal ligament, and commonly causes a crushing fracture of the alveolar socket (3).
The pulp and supporting structures of the tooth are severely damaged during intrusive dislocation because the tooth is dislocated into the alveolar process. Consequently, pulp necrosis, radicular inflammatory resorption, replacement root resorption, loss of marginal bone, and gingival retraction may occur (6).
The treatment type and prognosis change depending on the patient’s age, dentition type, tooth root development, time passed since the trauma, and severity. Three treatments are available: Waiting for spontaneous re-eruption, orthodontic repositioning, and surgical repositioning (7).
Lateral luxation injuries are diagnosed when a tooth is displaced in a position other than axial and is often associated with an alveolar bone fracture (8).
Epidemiological surveys indicate a high prevalence of traumatic dental injuries, especially during home accidents or sports activities. The frequency of lateral luxation injury is around 11% in traumatized permanent dentition (1).
Clinically, the crown of a laterally luxated tooth may be displaced and forced either labially or lingually. Displacing the apical portion of the tooth labially and fracturing the alveolar bone and root may get locked in this position, which may or may not show abnormal mobility. There may be a metallic sound on percussion with no tenderness to percussion and no positive response to sensibility testing. Lateral luxation injury may be managed by reduction of the fracture, splinting, clinical and radiographic observation of outcome, endodontic treatment, and extraction as per requirement (8).
2. Case Presentation
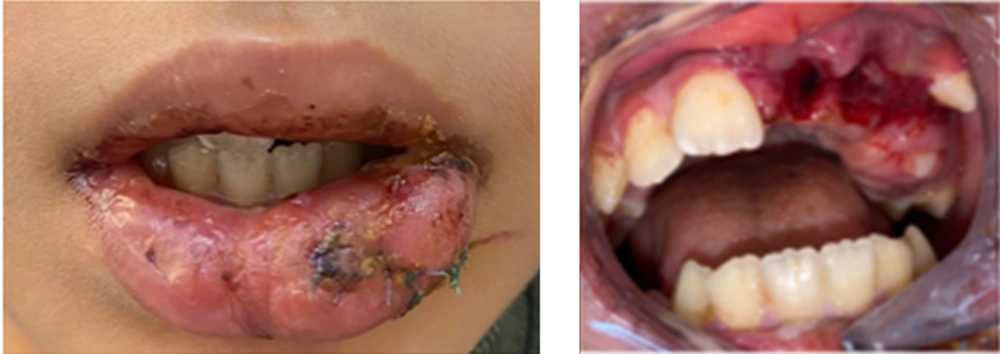
An 11-year-old boy was referred to the children’s ward of Hamadan dentistry faculty with an accidental hit to the window at home 24 hours ago. His lower lip was sutured in the hospital, and he was referred to the dentistry faculty to reposition his teeth. The patient’s extensive case history has been compiled. No relevant medical history was available. On extraoral view, there was no evidence of jaw fracture. The temporomandibular joint was evaluated for clinical and radiologic involvement and appeared unaffected. The lower lip appeared slightly swollen and edematous, and a sutured ulcer was present on the mucosal side, approximately 1cm in diameter. Intraoral examination showed tooth absence of left central and lateral incisors while the left canine was malposed in the maxilla (Figure 1).
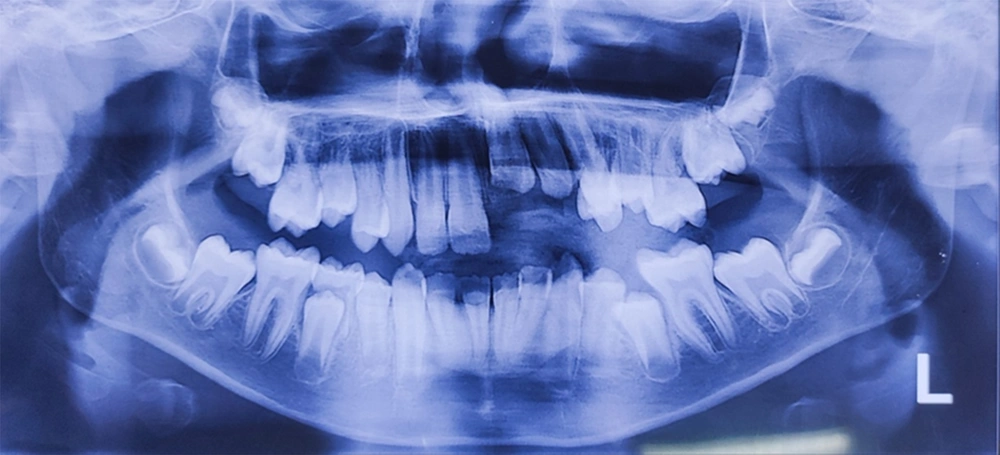
Patient compliance was low, so only panoramic radiography was ordered. Radiographic examination showed complete root formation and intrusion in the left central, lateral, and lateral luxation in the left canine (Figure 2).
Traumatized teeth were tested for pulpal sensitivity. The left central and lateral incisors were without response to cold and electric pulp tests, but the left canine had a normal response.
Informed consent was obtained from parents for treatment and publication of the treatment result.
An infiltration local anesthesia was administered, and intruded teeth were extracted with extraction forceps and repositioned to the correct position while very mobile. After consultation with an orthodontist, it was decided not to try repositioning the left canine to correct its position with fixed orthodontic treatment in the future.
Splinting was conducted with wire and composite splint from the right canine to the left lateral incisors on the labial surface with 0.7 mm stainless steel wire. In addition, an additional suture splint was applied due to the severe mobility of traumatized teeth (Figure 3).
The patient was apprised about using antibiotics (amoxicillin 500 mg, three times a day for five days), analgesics, mouth rinse (0.2% chlorhexidine gluconate two times a day for seven days), almost home care, and follow‑up visits. He was warned about the avoidance of biting his anterior teeth.
After ten days, when the mobility of teeth was reduced, the endodontic intervention was initiated on the left central and lateral incisors. The calcium hydroxide paste was applied to root canals to start the endodontic treatment.
Endodontic treatment was ended after four weeks, and teeth were obturated with gutta-percha. Access cavities were restored by amalgam filling, and the splint was removed (Figure 4).
Three follow-up sessions were scheduled, and the treatment was successful.
3. Discussion
Intrusive dislocations are among the most challenging injuries because opinions differ on the best treatment. The two main variables determining the treatment choice are the root development stage and the penetration severity. In Joshi et al. (9), the periodontal space between the tooth and the bone cannot be seen radiographically in intrusive cases.
Since immature permanent teeth tend to erupt and repair pulp/periodontal disease spontaneously, it is recommended to wait for re-eruption. When teeth are heavily intruded (> 7 mm) and root development is complete, surgical or orthodontic reduction is recommended with 2 - 3 weeks of splinting (9).
In Erverdi and Kargül’s (10) research, the age and degree of intrusion are identified: (1) re-eruption of teeth with the open or closed apex in patients aged 12 - 17 years with intrusion up to 7 mm due to their eruption potential; (2) immediate surgical repositioning with a fixation for teeth with closed tips and intrusions greater than 7 mm in patients between 12 and 17 years old and patients over 17 years old; (3) orthodontic extrusion is performed on teeth with a closed apex with an intrusion between 3 and 6 mm, remodeling of bone, and periodontal tissue on teeth with an open apex (5).
Hurley et al. recommended splinting the intruded tooth for four weeks in case of surgical reduction, which is flexible and allows physiological movement of the tooth to promote healing. This study reported that pulp necrosis occurs 100% of the time with a completely closed apex (7).
Kaushal et al. stated that fracture reduction, splinting, clinical and radiological observation of the outcome, endodontic treatment, and extraction as required to treat a lateral dislocation lesion (1). Still, in this case, repositioning the canine, which had a lateral luxation, was impossible due to the delay in visiting the doctor. As a result of cheek strength and improved position, this tooth can spontaneously correct during follow-up sessions. Clark and Levin reported that pulp necrosis (44.2%) was the most common complication in laterally dislocated mature teeth, but in the present case, the laterally dislocated tooth had no symptoms of pulp necrosis at follow-up sessions (8).
3.1. Conclusions
Rehabilitation of traumatically intruded teeth is challenging because the healing process is complex after intrusive luxation. The clinical and radiographic analysis showed that the incisors present satisfactory esthetic and functional demands in the present case. Surgical repositioning in the given case proved to be a viable treatment method for intrusive luxations without additional risk. Long-term clinical and radiographic follow-up is significant for the prognosis of the trauma. The tooth maintenance after traumatic episodes directly affected the patient’s quality of life and restored psychological and emotional states.