1. Background
Mortality and morbidity due to cardiac diseases rapidly increase worldwide, and their prevalence in developing, low, and middle-income countries. During the past 30 years, mortality from cardiovascular diseases has reached 32% of global mortality, indicating an increase in severe diseases’ prevalence, especially in less developing countries (1). Although the death rate due to coronary disease has decreased, it has been the most common cause in the United States during the past four decades and is responsible for 40% of all deaths annually. Nearly a quarter of those cases suddenly died (2) because the heart is one of the essential and sensitive parts of the human body, which affects the person’s mood and psychic (3). Lack of attention to stress and psychological reactance of the affected people causes disease development. Depression, anxiety, or excessive self-denial will postpone the disease improvement (4). Further, those who suffer from severe anxiety or depression are more likely to suffer from later problems, and the probability of their death is more likely than those with less stress. Therefore, heart patients’ essential problems are their mental and psychic problems (5). Therefore, their mental health and an attempt should be recognized to reduce complications because the patients’ lack of attention to stress and mental actions can cause the extent of their disease. According to the studies, one or two days after myocardial infarction, a short period of depression can be found, which is usually the peak of three or four days after MI (6). When the pain diminishes and the patient is assured of recovery, depression will die. However, a high percentage of the patients - long after myocardial infarction - remain depressed. Some patients suffer from these disorders in the intensive care unit. The severity of depression is not related to the severity of MI, as sometimes the depression of someone who has suffered a light infarction may be very deep. In contrast, another patient with a severe medical infarction will soon return to a normal position (7). Depression is the most common feeling that can involve patients after myocardial infarction. Depression should be reduced four weeks later after MI (8). Suppose the symptoms of depression are not lost after the end of this period. In that case, the family, physician, psychologist, and religious personality can help the patient care for immediate treatment. The symptoms of depression may be very mild. Someone who suffers from depression is often unaware of such a phenomenon (9). There have been over 100 studies of depression as a risk factor for incident cardiovascular disease. Many different self-report questionnaires and diagnostic interviews have been used to define depression in these studies (10). Some studies have focused on older adults, women or men only, or patients with cardiac risk factors such as hypertension (11). Despite the heterogeneity of the methods for assessing and defining depression and the populations examined, at least six meta-analyses have been performed. Five studies have found a 60 to 80% increased risk of incident cardiac disease associated with depression. One reported a more modest level of risk (30%), but all found that depression is a significant risk factor for developing cardiac disease (12). However, depression and anxiety disorders are associated with worse prognoses and quality of life in patients with cardiovascular diseases infrequently recognized or treated by cardiology providers. Many primary care physicians, cardiologists, and other specialists are now using a collaborative care model to assist in identifying and treating psychiatric disorders. In this model, treatment for depression or anxiety is managed by the primary care physician or specialist in consultation with a psychiatrist and another mental health professional, using a comprehensive surveillance plan based on evidence-based operational instructions. Social problem-solving skills training (SPSST) is one of the cognitive-behavioral therapy to reduce these disorders (13). Social problem-solving skills training is a way of therapy in which one learns to use practical cognitive skills to cope with troublesome social and interpersonal situations. The SPSST method can be considered an approach to deal with positional problems and their solutions. Also, problem-solving training is believed to increase self-efficacy and self-sufficiency (14). This method likely influences the types of emotions, social anxiety, and depression of the patients. Problem-solving is often described as independence, sufficiency, and self-confidence. First, the problem-solving model was proposed by D’Zurilla and Goldfried (15). The process of teaching social problem-solving consists of five steps that many theorists agree: General direction, definition, structuring problem, presentation of unique solutions, decision-making, and research and investigation (16-18).
2. Objectives
The prevalence of heart failure and depression, as well as its adverse effects in patients, need to perform a psychological intervention such as teaching social problem-solving skills, and this study was conducted for the lack of similar research.
3. Methods
3.1. Population
This study was conducted on male patients with heart failure with a systolic ejection fraction of lower than 45% and referred to the heart center of Imam Ali of Kermanshah, Iran, in 2022. Among 60 volunteers, 20 patients were selected based on inclusion criteria and randomly divided into control and intervention groups. The intervention group underwent ten sessions of one hour.
The inclusion criteria were: Age between 50 - 70 years, minimum secondary school education, maximum diploma degree, LVEF < 45%, Beck depression score > 7 and depression confirmed by psychology clinicians based on DSM-V, and absence of known psychological disorders. The exclusion criteria included voluntary exit and the lack of more than three sessions.
3.2. Ethical Considerations
Participants were explained the procedures for the study, the purpose and benefits, and that they were not at risk or in harm’s way before completing the informed consent form. Complete awareness of how to conduct the study, the authority to enter and volunteer, the exit of the study, the secrecy of the information, and the confidentiality of the administrators were considered.
3.3. Research Instruments
The data were collected using the Beck depression inventory (BDI-13). Beck’s depression inventory was introduced by Beck et al. in 1961 (19). Since the primary BDI only covered six criteria of nine criteria of depression, in 1996, it was revised to further coordinate with DSM-IV. The original version of this questionnaire had 21 items. A 13-item version was developed to use this questionnaire in the next few years. In this version, as in the 21-item version, each article contains four options from which the subject needs to choose. The validity and reliability of the questionnaire in several meta-analyses from 1961 to 1986 abroad were 0.81 and 0.86 (20), respectively. Based on scores, each individual can be placed in one of the categories of depression. In the Iranian version, the questionnaire was two sub-scales. Each question has 0 to 3 points, and the total score of the questionnaire is between 0 and 39. The assessment of depression is based on (21).
3.4. Data Collection Method
The patients were randomly divided into two groups of control and intervention groups. The Beck depression inventory was completed by patients. The intervention consisted of 10 one-hour sessions based on the instructions of the members of the faculty of the psychology department of the Kermanshah Branch of Islamic Azad University and previous authentic articles (22-24). This protocol was conducted for the intervention group by a psychologist with experience and license from the research group members in a training class for cardiac patients in Imam Ali Center (Table 1). Participants were re-called three months after the intervention, and the questionnaire was completed.
| Sessions | Descriptive |
|---|---|
| Session 1 | Introduction: Group rules, familiarity with self-awareness, and creating a combined atmosphere of trust and interaction with the goal of treatment |
| Session 2 | Determining the location and problem (depression mood), discussing the benefits of planning for the problem, identifying the current problem, selecting an appropriate approach to the problem, organizing and regulating the thoughts and feelings through dialogue, and paying attention to the relationship between an individual and the critical people in their lives. |
| Session 3 | Presenting the logic of treatment and emphasizing the importance of social problem-solving and making decisions in solving the problems and challenges of life and its effect on depression. Attention and importance of being in society, avoiding loneliness, and encouraging people to talk in groups and review thoughts that are alone. |
| Session 4 | Careful examination of different options and finding multiple solutions to a problem (depression): A lack of judgment at this stage with careful consideration of different options, brainstorming of different options, including the consequences of each option; resources and obstacles |
| Session 5 | Evaluation and prioritization of solutions step-by-step, implementation of social problem-solving methods |
| Session 6 | Reviewing the session before feedback from clients and check home assignments. Encouraging all clients to remember and plan their life challenges practice problem-solving methods for real problems, and propose different solutions. |
| Session 7 | Presenting home assignments and training emotional self-awareness and the diary of dysfunctional thoughts in the face of the problem. |
| Session 8 | Reviewing the session before client feedback, reviewing tasks, removing obstacles and problems, and encouraging all clients to plan their problems and express dysfunctional thoughts. Discussing the importance of dysfunctional thinking and its impact on depression |
| Session 9 | Evaluating and selecting the best option (final option) to solve the problem, expressing obvious and unambiguous problems, and encouraging the clients to become ambiguous problems as objective and transparent goals, stacking, and feedback of clients. |
| Session 10 | Emphasizes the importance and continuity of the skill of resolving conflicts in everyday life and the present situation, process reporting, and results of the social problem-solving techniques to solve the problem of a person and receive feedback. |
3.5. Statistical Analysis
The Shapiro-Wilk test was used to confirm the normal distribution of data. Paired t-test, independent t-test, and ANCOVA was used to compare the mean of variables. A P-value of less than 0.05 was considered significant in all the statistical analyses.
4. Results
The data were analyzed by SPSS software version 23, and descriptive and inferential statistics were used to analyze the data. All subjects were married and homogeneous in terms of education. The mean age of the subjects was 58.5 ± 3.2 in the control group and 57.6 ± 2.9 years in the intervention group (Table 2).
The Shapiro-Wilk test showed that the data had normal distribution, and Levene’s test revealed that all subjects were homogeneous variance in all groups (P > 0.05).
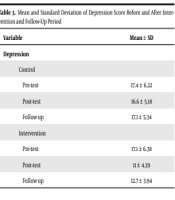
Table 3 reveals the mean values of the variable (depression) before, after, and during the follow-up period.
| Variable | Mean ± SD |
|---|---|
| Depression | |
| Control | |
| Pre-test | 17.4 ± 6.22 |
| Post-test | 16.6 ± 5.18 |
| Follow up | 17.1 ± 5.34 |
| Intervention | |
| Pre-test | 17.1 ± 6.38 |
| Post-test | 11 ± 4.39 |
| Follow up | 12.7 ± 3.94 |
Paired t-test was used to compare the mean scores of depression before and after intervention in each group. The independent t-test was used to compare the mean scores of depression in the control versus intervention group.
Table 4 indicated no significant difference between the different stages of study in the control group (P > 0.05). However, there was a significant difference between the pre-test and post-test in the intervention group (P = 0.000). In addition, there was a significant difference between the follow-up, and pre-test phases (P = 0.003), while no significant difference was denoted between the post-test and follow-up phases (P = 0.055) (Table 4).
| Comparison | Mean ± SD | 95% Confidence Interval of the Difference | t | df | P a | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Control | ||||||
| Pre/post | 0.8 ± 0.44 | -.2 | 1.8 | -1.809 | 9 | 0.104 |
| Pre/follow | 0.3 ± 0.39 | -0.59 | 1.1 | 0.75 | 9 | 0.468 |
| Post/follow | -0.5 ± 0.3 | -1.1 | 0.19 | 1.6 | 9 | 0.138 |
| Intervention | ||||||
| Pre/post | 6.1 ± 1.04 | 3.7 | 8.4 | 5.8 | 9 | 0.000 a |
| Pre/follow | 4.4 ± 1.06 | 1.98 | 6.81 | 4.1 | 9 | 0.003 a |
| Post/follow | -1.7 ± 0.73 | -3.3 | -0.4 | -2.3 | 9 | 0.055 |
a P-value < 0.05 is significant.
Table 4 shows that the comparison of the mean score of depression in the intervention group did not show a significant difference with the control group in the pre-test (P = 0.9). At the same time, there was a significant difference in the post-test between the intervention and the control groups (P = 0.018) (Table 5).
| Groups | Levene’s Test for Equality of Variances | t-Test for Equality of Means | |||||||
|---|---|---|---|---|---|---|---|---|---|
| F | P-Value | t | df | P-Value (2-tailed) | Mean Difference | Std. Error Difference | 95% Confidence Interval of the Difference | ||
| Lower | Lower | ||||||||
| Control vs. intervention (post) | 0.61 | 0.44 | 2.6 | 18 | 0.018 a | 5.6 | 2.15 | 1.08 | 10.11 |
| Control vs. intervention (pre) | 0.59 | 0.8 | 0.1 | 18 | 0.9 | 0.3 | 2.81 | -5.6 | 6.22 |
a P-value < 0.05 is significant.
In addition, the covariance analysis was used to compare the post-test and follow-up results with considering the covariate (pre-test result). As shown in Table 6, the results indicate a significant change in the intervention compared to the control group after the test and in the follow-up period (P = 0.000).
a P-value < 0.05 is significant.
5. Discussion
According to the results, training in SPSST in ten one-hour sessions effectively reduces depression scores in heart failure patients. This effect is significant even three months after training in the intervention group versus the control group. In previous studies, depressed patients have serious dysfunction in social problem-solving (24, 25). In addition, Noreen and Dritschel (26) found that people with high depression scores have social problem-solving dysfunction. Although numerous studies have been conducted to reduce depression in cardiac patients, the study of the effectiveness of SPSST on depression in cardiac patients has occurred in a few worldwide. Thoma et al. results were in line with the present research (24). The result of this study showed that social problem-solving skill training was influential in the treatment of major depression (27). Polat and Simsek showed that even a short period of skill training is effective in reducing depression and increasing the quality of life of heart inpatients (28). Omidi, et al. showed that this skill positively affects cardiac patients’ anxiety and sleep quality after CABG (29). In addition, Vollman et al. showed that heart patients who used problem-solving skills are less likely to have anxiety and depression symptoms than other patients and can control these factors well (30). Other studies have shown the effectiveness of social problem-solving skills training in reducing depression (31). Agren et al. (32) revealed that problem-solving skills could improve the control of mental problems in cardiac patients. According to Bayazi et al. (33) and Ghasemi et al. (34), short-term cognitive therapy had no significant effect on psychological disorders. This difference with the present study could be due to the short period of those studies. The mechanism of the effect of depression should be understood in heart patients to better understand how psychological disorders affect psychological interventions. Vaccarino et al. (35) showed that depression is effective in the outcome of heart failure patients through physiological mechanisms. Depression is associated with the activation of the sympathetic nervous system. An increase in norepinephrine has been recorded in depressed patients with norepinephrine and its metabolites in plasma and urine (36, 37). Charney et al. (38), and Golden et al. (39) found that therapy with anti-depressive drugs decreases plasma and urinary tract levels of norepinephrine and its metabolites. Du (40) revealed that heart failure is associated with the intense activation of the sympathetic nervous system. This factor plays a vital role in the progression of heart failure, and activation of the nervous and hormonal systems can worsen the heart rate and cause vascular spasms and sodium retention. In addition, increased activity of the sympathetic nervous system and the adrenal gland might predispose patients to ventricular arrhythmia and sudden cardiac death (41). Therefore, depression can be associated with increased levels of sympathetic activity in heart failure, which impairs and worsens heart failure, as well as depression by reducing heart rate and reducing heart rate variability (42, 43) as a risk factor for cardiac morbidity and mortality (44, 45). According to the above findings, several studies have been conducted regarding the impact of psychological interventions and the comparison of these interventions with drug interventions. Most of these studies have proved the positive effect of these interventions on neurohormonal factors in depression (46-50). Therefore, SPSST can be used as an effective method for reducing depression in heart failure patients, improving their quality of life, prognosis, and reducing mortality.
5.1. Conclusions
According to the results, cardiac patients who are depressed, other than using drugs, need to provide a solution to find the problem and find the best solution to solve it through social problem-solving skills is an effective method in treatment. Therefore, other health centers and chronic diseases involved in depression can use this solution.
5.2. Recommendation
It is recommended that a study be conducted to determine its efficacy in other chronic diseases as well.
The limitation of the study was participant’s absence in some meetings