1. Background
Many countries have recommended booster doses to ease the burden of rising death rates and severity caused by new strains of COVID-19 (1-4). Only 35.1% of Iranians and 34.6% of people worldwide received booster shots for COVID-19 (5). Only 346,000 (46.6%) of Kermanshah’s over-18 population (742,000 at the time of the research) received the third dose (6).
Factors affecting people’s reluctance to vaccinate against COVID-19 vary across countries and regions (7). Age, culture, government handling, and illness likelihood impact vaccine acceptance (8, 9). Perceived risks, uncertainty, and lack of information can lead to emotional, cognitive, and behavioral reactions, which influence public behavior.
COVID-19 challenges public health services’ communication ability with at-risk people and groups (10). Regular and active communication prevents misunderstandings and confusion. Health experts and authorities may differ on risk perceptions, while cultural values and beliefs heavily affect public perception (11). Community awareness should be increased for accurate, trustworthy, and accessible information for effective infection control (12). Community involvement in suggested behaviors is essential for effective infection control (13). Experts and researchers should understand the multifaceted nature of risk communication (RC) and willingness to receive COVID-19 booster doses (14).
Risk communication during epidemics is essential for sharing information about risks and facilitating good choices and preventive actions (13, 15). Risk communication involves sharing information about a risk’s nature, size, significance, or control among interested parties. As a result, informed choices and preventive measures can be taken to reduce the impact of crises (13). Risk communication raises awareness, improves knowledge, and influences behavior among stakeholders and public people. Effective risk communication minimizes damage in emergencies, as each person’s actions impact others (16).
Risk communication positively influences people’s willingness to receive booster doses by providing information about vaccine safety (17) and ensuring effectiveness (18). Vaccine hesitancy is also addressed, demographic messaging is tailored, and public health messages are promoted (19). Studies have indicated that booster shot uptake intent, institutional trust, and public risk information positively correlate, emphasizing risk communication (20).
Studies on the impact of risk communication on COVID-19 booster doses in Iran are limited. This study examined how risk communication affected people’s desire to get COVID-19 booster shots in Kermanshah, Iran, in 2022.
2. Objectives
This study evaluated the association between risk communication and willingness to receive booster doses of COVID-19 vaccinations in Kermanshah, Iran, in 2022. According to the study, the most important sources of information were the frequency of vaccine doses received, the degree of unwillingness, and the reasons for refusal.
3. Methods
3.1. Study Design
This cross-sectional descriptive-analytical study was conducted on 746 over 18 people in 2022 who completed the first and second doses of the COVID vaccine. More than six months were passed since the second dose, and they were willing to participate in the study.
3.2. Data Collection
The data were collected using an online questionnaire on an Iranian platform (https://survey.porsline.ir). The questionnaire was divided into four sections: demographic data (17 questions), information on the COVID-19 vaccine, and information about risk communication. The research construct (RC) was adapted by Heydari et al. into a valid and accurate questionnaire (16) based on four parts. (1) Exposure to news media was separated into two categories: traditional mass media and the internet, with two questions. The level of exposure was assessed on a 5-point scale ranging from 1 (often) to 5 (never); (2) Information-gathering ability with three questions; (3) Trust in the government with three questions, and (4) Trust in the news media with three questions were assessed. All questions were evaluated using a 5-point Likert scale ranging from 1 (total agreement) to 5 (full disagreement). The final score was calculated using the average.
The willingness to get a COVID vaccination booster dosage (3 questions), adapted by S. Vellappally (21). The willingness was measured on a 4-point scale ranging from 1 (agree) to 4 (disagree). The respondents who selected the “I agree” and “very agree” options were categorized as willing to receive. This study was approved by the ethics committee of the Kurdistan University of Medical Sciences protocol (IR.MUK.REC.1401.264). A written consent form was sent to participants before the survey began, outlining the project's aims.
3.2.1. Validity and Reliability
The questionnaire was prepared by searching for reliable sources. Heydari et al. (16) evaluated a questionnaire’s transparency, comprehensiveness, and correlation with five academic experts to assess the comprehensiveness and correlation of items. In this research, factor analysis and Cronbach’s alpha coefficient were calculated to ensure the correct selection of measurement items and the reliability of the questionnaire. The study used factor analysis and Cronbach’s alpha coefficient to ensure appropriate question selection and questionnaire reliability. Factor loading values for each subscale of risk communication were 0.599 and 0.647 for News Media Exposure. The values of Information Gathering Ability were 0.542, 0.852, and 0.873. The values of Trust in the Government included 0.565, 0.790, and 0.738. The values of Trust in the News Media values were 0.823, 0.803, and 0.823. The Cronbach’s alpha coefficient was more than 0.7.
The data were analyzed using SPSS software version 22. The chi-square test determined the relationship between demographic variables, including gender, marital status, age, education, number of children, nationality, religion, and underlying disease with “reluctance to receive COVID-19 booster doses”. In addition, univariate logistic regression was performed to identify the relationship between vaccine willingness and risk communication with reporting adjusted odd ration (AOR).
4. Results
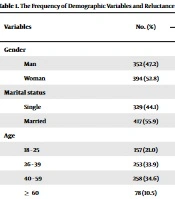
Table 1 reports the demographic characteristics of the participants. More than half of the respondents (61.9%) received the Sinopharm vaccination twice. Table 2 shows that 36.3% are willing to get booster doses of the vaccine when they are foreign (30.4%) and when they are internal or Iranian (14.1%).
| Variables | No. (%) | Willingness to Receive Booster Doses of COVID-19, No. (%) | P-Value | |
|---|---|---|---|---|
| Yes | No | |||
| Gender | ||||
| Man | 352 (47.2) | 141 (40.1) | 211 (59.9) | 0.045 |
| Woman | 394 (52.8) | 130 (33.0) | 264 (67.0) | |
| Marital status | ||||
| Single | 329 (44.1) | 117 (35.6) | 212 (64.4) | 0.701 |
| Married | 417 (55.9) | 254 (36.9) | 264 (63.1) | |
| Age | ||||
| 18 - 25 | 157 (21.0) | 58 (36.9) | 99 (63.1) | |
| 26 - 39 | 253 (33.9) | 77 (30.4) | 176 (69.6) | 0.045 |
| 40 - 59 | 258 (34.6) | 97 (37.6) | 161 (62.4) | |
| ≥ 60 | 78 (10.5) | 39 (50.0) | 39 (50.0) | |
| Education | ||||
| Illiterate, middle school and high school | 142 (19.0) | 54 (38.0) | 88 (62.0) | |
| Diploma | 206 (27.6) | 69 (33.5) | 137 (66.5) | 0.601 |
| University | 398 (53.4) | 148 (37.2) | 250 (62.8) | |
| Number of children | ||||
| ≤ 1 | 421 (56.4) | 148 (35.2) | 273 (64.8) | |
| 2 | 166 (22.3) | 60 (36.1) | 106 (63.9) | 0.709 |
| 3 | 88 (11.8) | 33 (37.5) | 55 (62.5) | |
| ≥ 4 | 71 (9.5) | 30 (42.3) | 41 (57.7) | |
| Ethnicity | ||||
| Kurd | 635 (85.1) | 226 (35.6) | 409 (64.4) | 0.317 |
| Other | 111 (14.9) | 45 (40.5) | 66 (59.5) | |
| Religion | ||||
| Shi’ism | 602 (80.7) | 225 (37.4) | 377 (62.6) | 0.223 |
| Sunni | 144 (19.3) | 46 (31.9) | 98 (68.1) | |
| Underlying disease | ||||
| Yes | 279 (37.4) | 120 (43.0) | 159 (57.0) | 0.003 |
| No | 467 (62.6) | 151 (32.3) | 316 (67.7) | |
| Total | 746 (100) | 271 (36.3) | 475 (63.7) | |
| Variables | No. (%) |
|---|---|
| Sinopharm (two doses) | 462 (61.9) |
| AstraZenica (two doses) | 163 (21.8) |
| CovIran Barkat (two doses) | 66 (8.8) |
| Sputnik V (two doses) | 35 (4.7) |
| Indian Bharat (two doses) | 10 (1.3) |
| PastoCovac (one doses) | 10 (1.3) |
Age, sex, and a history of underlying disease significantly impacted the willingness to receive booster vaccine doses. Men, people over the age of 60, and those with underlying illnesses were more likely to receive a booster dose (P < 0.05). Other demographic characteristics, such as religion and ethnicity, had no significant relationship with the willingness to get a booster dose (Table 1).
The main reasons for refusing a booster dose were the end of the COVID-19 epidemic (56.4%) and fear of side effects from the third dose (55.0%). The two essential sources of information regarding booster doses of the vaccination were social networks (51.6%) and television (51.1%). The t-test showed that individuals who want COVID-19 vaccine booster doses have significantly higher risk communication compared to those who do not (P < 0.001) (Table 3). The multivariate regression results showed that risk communication (AOR = 1.54; CI = 1.08 – 2.20) has a direct and significant relationship with the willingness to receive booster doses of the COVID-19 vaccine (Table 4).
| Variables | Willingness to Receive Booster Doses of the COVID-19 Vaccine | P-Value | |
|---|---|---|---|
| Yes | No | ||
| Risk Communication | 2.60 ± 51.0 | 2.46 ± 48.0 | 0.001 |
a Values are expressed as mean ± SD.
5. Discussion
Males were more inclined to get booster doses of the COVID-19 vaccine (P < 0.05), which is consistent with earlier studies (21, 22). A study found that men’s desire was 2.5 times higher than women’s (23). Female desire may be lower due to psychological gender differences (24), aversion to novel medical technology (25), and belief in vaccine-fertility myths shared on social media (26, 27). The highest willingness to receive the vaccine was observed in the age group over 60. According to a review study, eight out of 12 studies reported a significantly higher likelihood of older individuals accepting the first booster dose of the vaccine (23). The greater tendency in older adults may be due to the high probability of getting a severe form of the disease, hospitalization, and mortality due to COVID-19 (24). People with an underlying condition were more likely to get a booster dosage, while unwillingness in healthy individuals was also found (4). Intervention activities are essential for individuals with high health status but limited exposure to health education due to limited facility visits.
Only 36.3% of participants in this study were willing to get booster doses of the vaccination, compared to 44.6% in a comparable survey in Jordan (25). Research has shown that booster dosages are more common in other nations (26). In Denmark, 90% of the study population responded that they would want it when the booster dosage was offered once (27).
In some countries, vaccination is mandatory (21), but in Oran, the public policy prioritizes administering first and second doses rather than booster shots. In study implementation, COVID-19 decreases mortality and hospitalization, impacting willingness to receive booster doses. Studies have revealed people’s reluctance to accept booster doses due to no longer needing a vaccine and fear of side effects (28, 29). This study confirmed the issue related to COVID-19’s total absence due to elements such as illness subsidence, worry disappearance, and confidence in its total disappearance (29).
The results regarding the acceptance of domestic and foreign vaccines were aligned with a previous study on the challenges of initial vaccine uptake in Tehran. About 58% of participants preferred imported vaccines, while 25% opted for vaccines manufactured in Iran (30). A lack of locally made vaccines during outbreaks exacerbates the issue, as people often choose vaccinations based on past experiences. Researchers suggested that more research be conducted to determine why people distrust local vaccines and then take the steps necessary to improve them. This study found that people with a higher average risk of communication were more willing to get booster doses of vaccines. A study stated that risk communication can help reduce the number of people who do not want to use a booster vaccine (21). According to Miao et al., risk communication plays a significant role in Chinese people's willingness to receive booster doses of vaccines. This approach allows for educating the public about vaccination’s advantages and potential risks (31). Distressing news affects willingness to receive COVID-19 booster doses, and effective messaging and dissemination are crucial for increased acceptance (32). Prior studies have shown that vaccine hesitancy stems from sociocultural factors, distrust in government authorities (33), individual, and group influences, and misinformation about vaccines (34).
Social media and television were the two essential sources of information about the COVID-19 vaccination for participants. Rapid dissemination of fake news, rumors, and false information on social networks can influence people’s actions and behavior during crises by strengthening false beliefs (35). Social networks can implement public health initiatives by producing authentic, scientific content and increasing vaccination willingness.
5.1. Conclusions
The study highlighted the importance of risk communication in addressing vaccine hesitancy and misinformation. Factors such as belief at the end of the COVID-19 pandemic and concerns about potential side effects were the primary reasons for refusing booster doses. Distressing news and false information on social media can influence people’s behavior during crises, underscoring the need for reliable, science-based content dissemination. Effective messaging and accurate information dissemination could increase vaccine acceptance. Vaccine acceptance and protection of public health are emphasized through tailored public health initiatives, accurate information dissemination, and targeted interventions in the face of the pandemic. Further research is recommended to better understand the reasons behind vaccine hesitancy and develop strategies promoting trust and confidence in vaccination programs.