1. Background
Coronavirus (COVID-19) is an acute respiratory illness caused by the new RNA virus, acute respiratory syndrome, and coronavirus SARS-CoV-2 (1, 2). The number of people with COVID-19 worldwide has increased significantly since the first report of SARS-CoV-2 patients in Wuhan, China, in December 2019 (3-5). A large wave of COVID-19 generated by SARS-CoV-2 variants has been experienced in 2022 (Delta, Lambda, Mo, and Omicron). Approximately 80% of people infected with SARS-CoV-2 were at a mild to moderate state. The remaining 20% may reach a severe clinical stage for about one week, and 5% of all individuals will develop intubation or death (3, 6). Identifying the patients’ characteristics that may lead to significant complications and mortality is essential. Knowing about vulnerable populations will lead to implementing prevention strategies, prognosis tools, and potential treatment options in the future (7). Research has shown that elderly (65 years and above) with an underlying disease, such as high blood pressure, chronic kidney disease, obesity, and diabetes, are at increased risk for the disease, as well as higher rates of COVID-19 mortality (8). According to SARS in 2003, Cheng et al. showed a relationship between ABO blood type and post-exposure SARS-CoV-2 infection. Blood type O populations were believed to be less susceptible to SARS. Intrinsic mechanisms were also investigated, showing that human antihistamine antibodies could block the interaction between viruses and cells by binding to the spike (S) protein (9). As a result, efforts have been made to explore further links between patient characteristics and COVID-19. The relationship between blood type and COVID-19 appeared in March 2020 (10). Several brief scientific reports examined the relationship between the ABO group and the risk of SARS-CoV-2 infection during the SARS-CoV-2 epidemic in 2019. Meanwhile, studies on the relationship between blood type and coronavirus 2019 have been published. Early reports of Zhao et al. (11) and Li et al. (12) indicated a relationship between the disease and blood type (13). Recently, patients with type A or AB were related to increased risk and severity of the disease, and patients with type B or O were related to decreased disease severity (14). However, other studies have failed to provide evidence of a relationship between blood type and mortality in COVID-19 patients (15, 16).
2. Objectives
According to the different results, a study was conducted through blood type to evaluate the mortality and survival of patients with COVID-19.
3. Methods
3.1. Study Design
This study was accomplished by retrospective cohort method on the recorded data of COVID-19 patients admitted to Farabi and Golestan-Kermanshah hospitals.
3.2. Sample Size and Sampling Method
This study was conducted on patients with COVID-19 between March 2021 and January 2022 who were selected by convenient sampling. The inclusion criteria were patients with a minimum age of 18 years and a maximum age of 85 years old with positive PCR test results. The exclusion criteria included incomplete information recorded in the patient's files and having concomitant diseases such as hepatitis, AIDS, influenza, and tuberculosis.
3.3. Data Collection Tools and Methods
A researcher-made checklist was used to collect data. The checklist includes demographic information (gender, smoking status, intubation, underlying disease), symptoms of COVID-19 disease (fever and chills, muscle aches, shortness of breath, weakness, and lethargy), blood type (O, A, AB, and B), as well as the patient's condition (death/discharge), which was extracted from the patient's file.
3.4. Data Analyzing
Mean and standard deviation were used to describe quantitative data, and frequency and percentage were used to describe qualitative data. Kaplan-Meyer method was used to determine the survival rate (mean survival time). The rank logarithm test was used to identify variables affecting patient survival time to fit the best model with survival data. The generalized Cox model included all variables with a P-value of less than 0.25. The response variable was the number of hospitalization days. The appropriate model was fitted using the stepwise method by eliminating the effect of confounders. The risk ratio and 95% confidence interval were calculated for factors related to the survival of patients with COVID-19. The Logistic regression model was used to determine the chances of factors related to patient mortality. The collected data were analyzed using STATA software version 14. The significance level of statistical tests was considered 0.05.
4. Results
The present study was performed on 644 patients with COVID-19 with ABO blood group. About 22.67% (n = 146) had blood type O, 11.49% (n = 74) AB, 24.38% (n = 157) B, and 41.46% (n = 267) A. In addition, 74.53% (n = 480) of the patients were male. Blood group A had the highest prevalence of blood group among men (n = 220, 45.83%). There was a significant relationship between gender and blood group (P = 0.001). The mean ± standard deviation of patients, age was 52.55 ± 16.9 years. In general, the mean number of hospitalization days was 7.736 ± 6.32 days, with blood group O with the longest hospital stay at 7.50 ± 10.08 days compared to other blood groups (Table 1).
| Variables | Total | Blood Type | P-Value b | |||
|---|---|---|---|---|---|---|
| O | AB | B | A | |||
| Sex | 0.001 | |||||
| Female | 164 (25.47) | 44 (26.83) | 26 (15.85) | 47 (28.66) | 47 (28.66) | |
| Male | 480 (74.53) | 102 (21.25) | 48 (10.0) | 110 (22.92) | 220 (45.83) | |
| Smoking | 0.912 | |||||
| Yes | 6 (0.93) | 1 (16.67) | 1 (16.67) | 2 (33.33) | 2 (33.33) | |
| No | 638 (99.07) | 145 (22.73) | 73 (11.44) | 155 (24.29) | 265 (41.54) | |
| Entobasion | 0.003 | |||||
| Yes | 69 (15.94) | 13 (13.27) | 3 (4.35) | 12 (17.39) | 41 (59.42) | |
| No | 364 (84.06) | 85 (23.35) | 48 (13.19) | 98 (26.92 | 133 (36.54 | |
| Underlying disease | 0.776 | |||||
| Yes | 277 (37.27) | 47 (20.70) | 29 (12.78) | 55 (24.23) | 96 (42.29) | |
| No | 382 (62.73) | 92 (24.08) | 45 (11.78) | 94 (24.61) | 151 (39.53) | |
| Ward | 0.001 | |||||
| Non-ICU | 199 (30.95) | 27 (13.57) | 18 (9.05) | 83 (41.71) | 71 (35.68) | |
| ICU | 444 (69.05) | 119 (26.80) | 56 (12.61) | 73 (16.44) | 196 (44.14) | |
| Ague | 0.016 | |||||
| Yes | 224 (34.78) | 60 (26.79) | 30 (13.39) | 60 (26.79) | 74 (33.04) | |
| No | 420 (65.22) | 86 (20.48) | 44 (10.48) | 97 (23.10) | 193 (45.95) | |
| Muscle pain | 0.216 | |||||
| Yes | 196 (30.43) | 51 (26.02) | 26 (13.27) | 49 (25.0) | 70 (35.71) | |
| No | 448 (69.57) | 95 (21.21) | 48 (10.71) | 108 (24.11) | 197 (43.97) | |
| Shortness of breath | 0.582 | |||||
| Yes | 473 (73.45) | 107 (22.62) | 56 (11.84) | 109 (23.04) | 201 (42.49) | |
| No | 171 (26.55) | 39 (22.81) | 18 (10.53) | 48 (28.07) | 66 (38.60) | |
| Weakness and lethargy | 0.518 | |||||
| Yes | 139 (21.58) | 28 (20.14) | 16 (11.51) | 30 (21.58) | 65 (46.76) | |
| No | 505 (78.42) | 118 (23.37) | 58 (11.49) | 127 (25.15) | 202 (40.00) | |
| Death | 0.011 | |||||
| Yes | 122 (18.94) | 17 (13.93) | 9 (7.38) | 34 (27.87) | 62 (50.82) | |
| No | 522(81.06) | 129 (24.71) | 65 (12.45) | 123 (23.56) | 205 (39.27) | |
| Age (y) | 52.55 ± 16.9 | 51.95 ± 18.8 | 55.51 ± 17.6 | 55.51 ± 17.6 | 51.25 ± 16.2 | 0.088 |
| BMI | 25.73 ± 3.21 | 24.72 ± 1.99 | 26.24 ± 3.13 | 26.24 ± 3.1 | 25.89 ± 3.6 | 0.004 |
| Temperature | 37.01 ± 0.80 | 36.75 ± 0.69 | 37.07 ± 0.81 | 37.07 ± 0.81 | 37.12 ± 0.86 | 0.003 |
| WBC | 8.48 ± 6.27 | 7.99 ± 3.82 | 8.30 ± 3.98 | 8.30 ± 3.98 | 9.14 ± 8.49 | 0.122 |
| RDW | 14.07 ± 1.89 | 13.85 ± 1.86 | 14.15 ± 2.05 | 14.15 ± 2.05 | 14.18 ± 1.93 | 0.317 |
| Hb | 12.51 ± 1.86 | 12.57 ± 1.87 | 12.51 ± 1.81 | 12.51 ± 1.81 | 12.36 ± 1.87 | 0.316 |
| Lymph | 18.76 ± 11.4 | 18.89 ± 11.2 | 18.86 ± 11.7 | 18.86 ± 11.7 | 17.98 ± 11.30 | 0.384 |
| Cr | 1.23 ± 0.94 | 1.12 ± 0.65 | 1.24 ± 0.65 | 1.24 ± 0.65 | 1.24 ± 0.88 | 0.760 |
| The time in hospitalization | 6.32 ± 7.73 | 7.5 ± 10.08 | 6.11 ± 7.34 | 6.11 ± 7.34 | 5.59 ± 4.37 | 0.088 |
Abbreviation: SD, standard devotion.
a Values are presented as mean ± SD or No (%).
b P-values were calculated by one-way ANOVA and Fisher's exact test or χ2 test for the categorical variables; P < 0.05 was considered significant.
The logistic regression model was used to determine the chances of death of patients regardless of their blood type. The results showed that men casualties were 0.85 times more than women (OR = 0.85, 95% CI = 0.55, 1.33). In addition, the rate of death was 1.03 with a one-year increase in age (OR = 1.03, 95% CI = 1.02, 1.04). The death rate of patients with blood groups AB, B, and A compared to blood group O were 1.05, 2.09, and 2.09, respectively. Patients admitted to the ICU were 1.53 times more likely to die than patients in other wards (OR = 1.53, 95% CI = 0.97, 2.41). Moreover, patients who were intubated were 3.12 times more likely to die than patients without intubation (OR = 3.12, 95% CI = 1.82, 5.32). The death rate of patients per day of hospitalization was 1.03 times higher (OR = 1.03, 95% CI = 1.01, 1.05) (Table 2).
| Variables | Total | Death | Unadjusted | |
|---|---|---|---|---|
| OR (95%Cl) | P-Value b | |||
| Sex | 0.499 | |||
| Female | 164 (25.47) | 34 (20.73) | 1 (Ref.) | |
| Male | 480 (74.53) | 88 (18.33) | 0.85 (0.55, 1.33) | |
| Blood type | ||||
| O | 146 (22.67) | 17 (11.64) | 1 (Ref.) | |
| AB | 74 (11.49) | 9 (12.16) | 1.05 (0.44, 2.48) | 0.910 |
| B | 157 (24.38) | 34 (21.66) | 2.09 (1.11, 3.94) | 0.022 |
| A | 267 (41.46) | 62 (23.22) | 2.29 (1.28, 4.09) | 0.005 |
| Smoking | 0.886 | |||
| No | 638 (99.07) | 121(18.97) | 1 (Ref.) | |
| Yes | 6 (0.93) | 1(16.67) | 0.85 (0.09,7.38) | |
| Entobasion | 0.001 | |||
| Yes | 69 (15.94) | 32 (46.38) | 1 (Ref.) | |
| No | 364 (84.06) | 79 (21.70) | 3.12 (1.82, 5.32) | |
| Underlying disease | 0.001 | |||
| Yes | 227 (37.27) | 63 (27.75) | 1 (Ref.) | |
| No | 382 (62.73) | 55 (14.40) | 2.28 (1.51, 3.42) | |
| Ward | 0.067 | |||
| Non-ICU | 444 (69.05) | 92 (20.72) | 1 (Ref.) | |
| ICU | 199 (30.95) | 29 (14.57) | 1.53 (0.97, 2.41) | |
| Ague | 0.003 | |||
| Yes | 224 (34.78) | 28 (12.50) | 1 (Ref.) | |
| No | 420 (56.22) | 94 (22.38) | 0.49 (0.31, 0.78) | |
| Muscle pain | 0.001 | |||
| Yes | 196 (30.43) | 20 (10.20) | 1 (Ref.) | |
| No | 448 (69.57) | 102 (22.77) | 0.38 (0.23, 0.64) | |
| Shortness of breath | 0.220 | |||
| Yes | 473 (73.45) | 95 (20.08) | 1 (Ref.) | |
| No | 171 (26.55) | 27 (15.79) | 1.34 (0.83, 2.14) | |
| Weakness and lethargy | 0.001 | |||
| Yes | 139 (21.58) | 42 (30.22) | 1 (Ref.) | |
| No | 505 (78.42) | 80 (15.84) | 2.30 (1.49, 3.54) | |
| Age (y) | 52.55 ± 16.9 | 60.07 ± 17.01 | 1.03 (1.02, 1.04) | 0.001 |
| BMI | 77.96 ± 3.21 | 25.97 ± 3.98 | 1.03 (0.96, 1.09) | 0.367 |
| Temperature | 37.01 ± 0.80 | 36.99 ± 0.71 | 0 .98 (0.74, 1.29) | 0.871 |
| WBC | 8.48 ± 6.27 | 9.22 ± 4.08 | 1.01 (0 .99, 1.04) | 0.198 |
| RDW | 14.07 ± 1.89 | 14.65 ± 2.35 | 1.19 (1.08, 1.31) | 0.001 |
| Hb | 12.51 ± 1.86 | 12.38 ± 1.83 | 0.95 (0.86, 1.06) | 0.423 |
| Lymph | 18.76 ± 11.4 | 15.57 ± 11.14 | 0.96 (0.94, 0.98) | 0.001 |
| Cr | 1.23 ± 0.94 | 1.35 ± 1.47 | 1.13 (0.95, 1.35) | 0.154 |
| The time in hospitalization | 6.32 ± 7.73 | 8.00 ± 9.66 | 1.03 (1.01, 1.05) | 0.012 |
a Values are presented as mean ± SD or No (%).
b P-value < 0.05 was considered significant.
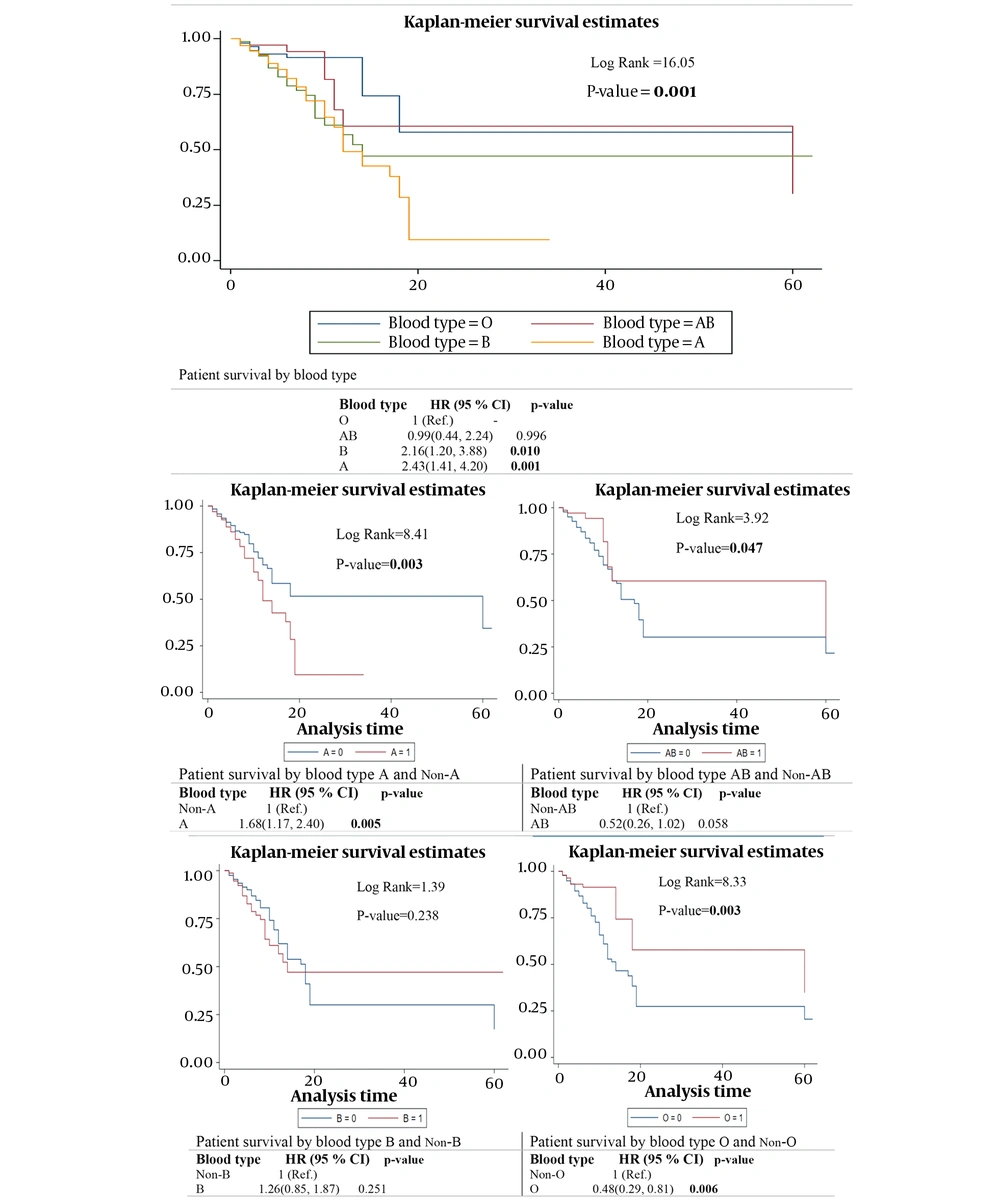
Figure 1 reports the unadjusted Cox regression model and Kaplan-Meyer diagram to compare the hospitalization period with recovery or death status in the ABO blood group. In the Kaplan-Meyer diagram, blood groups O and AB had higher survival rates than blood groups A and B, which showed a significant difference in the log-rank test (P = 0.001). The results of the Cox regression model showed that patients with blood group B had 2.16 and 2.43 times shorter survival time than those with blood group O, which was significant (P = 0.001, Figure 1). Patients with blood type A were 1.68 times shorter than those with blood type A and blood type B was 1.26 times shorter survival time than those with blood type other than B. In addition, the life expectancy of patients with blood groups AB and O was longer than those with blood groups other than AB (Figure 1).
The simple and multiple Cox regression model results showed that men's survival time was 0.96 times more than women (OR = 0.96, 95% CI = 0.64, 1.44). In addition, the survival time decreases 1.02 times for one year older (OR = 1.02, 95% CI = 1.01, 1.03). Patients admitted to the ICU had 1.56 times less survival time than patients admitted to other wards (OR = 1.56, 95% CI = 1.02, 2.37). Moreover, intubated patients had a longer lifespan of 1.37 times longer than patients who were not intubated (OR = 1.37, 95% CI = 0.91, 2.09) (Table 3).
| Variables | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| HR (95%Cl) | P- Value a | AHR (95%Cl) | P- Value a | |
| Sex | 0.876 | - | ||
| Female | 1 (Ref.) | - | ||
| Male | 0.96 (0.64, 1.44) | - | ||
| Smoking | 0.916 | - | ||
| No | 1 (Ref.) | - | ||
| Yes | 1.11 (0.15, 7.99) | - | ||
| Entobasion | 0.133 | - | ||
| No | 1 (Ref.) | - | ||
| Yes | 1.37 (0.91, 2.09) | - | ||
| Underlying disease | 0.044 | 0.882 | ||
| No | 1 (Ref.) | 1 (Ref.) | ||
| Yes | 1.45 (1.01, 2.10) | 1.03 (0.68, 1.54) | ||
| Ward | 0.037 | 0.135 | ||
| Non-ICU | 1 (Ref.) | 1 (Ref.) | ||
| ICU | 1.56 (1.02, 2.37) | 1.40 (0.90, 2.18) | ||
| Ague | 0.004 | 0.125 | ||
| No | 1 (Ref.) | 1 (Ref.) | ||
| Yes | 0.53(0.34, 0.81) | 0.68(0.41, 1.11) | ||
| Muscle pain | 0.040 | 0.519 | ||
| No | 1 (Ref.) | 1 (Ref.) | ||
| Yes | 0.60 (0.37, 0.97) | 0.83 (0.47, 1.45) | ||
| Shortness of breath | 0.993 | - | ||
| No | 1 (Ref.) | - | ||
| Yes | 0.99 (0.64, 1.53) | - | ||
| Weakness and lethargy | 0.001 | 0.002 | ||
| No | 1 (Ref.) | 1 (Ref.) | ||
| Yes | 1.99 (1.37, 2.90) | 1.91 (1.28, 2.85) | ||
| Age (y) | 1.02 (1.01, 1.03) | 0.001 | 1.02 (1.01, 1.03) | 0.001 |
| BMI | 1.03 (0.97, 1.08) | 0.338 | - | - |
| Temperature | 1.04 (0.79, 1.36) | 0.752 | - | - |
| WBC | 1.01 (0.98, 1.03) | 0.526 | - | - |
| RDW | 1.08 (1.01, 1.17) | 0.045 | 1.07 (0.98, 1.16) | 0.090 |
| Hb | 0.99 (0.90, 1.09) | 0.911 | - | - |
| Lymph | 0.98 (0.96,0.99) | 0.048 | 0.99 (0.97, 1.01) | 0.593 |
| Cr | 1.03 (0.91, 1.16) | 0.595 | - | - |
a P-value < 0.05 was considered significant.
5. Discussion
Since the advent of COVID-19, different results have been reported regarding the correlation between blood type, mortality, and survival rates among infected individuals. The relationship between COVID-19 and ABO blood type has been a controversial area and an active research topic worldwide.
In this study, the frequency of blood groups was A (41.46%), B (24.38%), O (22.67%), and AB (11.49%), respectively. A case-control study conducted in Wuhan, China, in 2020 on 105 positive cases of COVID-19 and 103 controls showed the prevalence of blood groups A (42.8%), B (26.8%), AB (8.57%) and O (21.9%) (17). A study by Yan Cheng et al. on 256 hospitalized patients with COVID-19 showed that blood groups were A (25%), B (24%), AB (4%) and O (47%) (18). In addition, a study conducted in South America in 2020 on people with COVID-19 showed that most patients had blood type O (49%), followed by A (27%), B (19%), and AB (7). Since different studies have been performed on diverse populations with different genotypes, the difference in frequency of blood groups in different studies may be due to the study population.
The present study showed that the mean age of people with COVID-19 is 52.55 ± 16.9 years, which showed a significant relationship between age, morbidity, and mortality (P = 0.001). Researchers have also found that age and gender are associated with susceptibility or severity of SARS-CoV-2 infection (19). In other studies, it has been proved that aging results in a higher mortality rate, and the risk of death in people over 50 years is 3.77 times higher than in people under 50 years (20). A study by Nikolic-Zurgich on aging and the immune system showed that immunity is a set of age-related changes that affect the immune system and lymphatic organs and increase vulnerability to infectious diseases over time. As a result, older people are more prone to mortality and complications associated with infectious diseases (21). Age is a significant predictor of morbidity and mortality, which is unsurprising. As a result, specific preventive and therapeutic measures must be implemented in the elderly population.
Women were involved more than men with the disease and lost their lives as a consequence. A study conducted in Massachusetts was also consistent with the present study (22). A survey of 120 people with COVID-19 in Mexico found that the risk of mortality in men was 1.74 times higher than in women but did not show a significant relationship (20). A study by Katharine E on patients with COVID-19 showed that male gender and aging were significantly related to death (7).
People with blood type A were more susceptible to SARS-CoV-2 infection. In the first report, Zhao et al. stated that SARS-CoV-2 tended to infect people with blood type A among people with different blood types, and type O was less infected (11). The results of other studies also showed that people with blood type A are more prone to infectious diseases than other blood groups, which was consistent with the present study (23). Another study showed a significant relationship between COVID-19 disease and blood type A, which was not observed in other blood groups (17). Other studies have suggested that people with blood type A may be at increasing risk for infection, and type O may be protective (16, 24). Determining why blood type A populations are more susceptible to the SARS-CoV-2 virus is complex. In fact, in most cases, the cause of some diseases in a particular blood type is still unclear.
The blood group types among patients with COVID-19, blood groups A and B with increasing risk of death compared with blood type O, were correlated. A study by James Szymanski et al. in New York on 6574 patients with COVID-19 showed that the risk of death in blood group A (HR = 1.17, CI = 1.02 - 1.33) and blood group B (HR = 1.29, CI = 1.08 - 1.54) increased compared to blood group O (13). A study in Wuhan, China, found that people with COVID-19 in blood type A had a higher risk of death (25). Li et al. found a similar relationship between ABO and COVID-19 at a central hospital in Wuhan, China (12). Other studies have also indicated that non-O blood types are at higher risk for infection and death (26). The present study showed that blood group O was younger than the other blood groups, but there was no significant relationship between age and blood groups. A cohort study conducted at three different hospitals in China showed that people with blood type O had a younger mean age, and this study did not show a significant relationship between age and blood type (10). However, an analysis of African Americans hospitalized in the United States found that people with AB blood type had a lower mean age than other blood groups (18). Therefore, age is a confounding factor for the survival of patients based on blood group. Consequently, checking the survival of patients with COVID-19 based on blood groups in almost the same age groups is suggested.
5.1. Conclusions
Based on the results, there was a significant relationship between the survival rate of patients with COVID-19 and their blood type. Blood group A and blood group B had an increasing risk of death compared to blood group O. On the other hand, most hospitalized patients in the intensive care unit had blood type A. Blood groups A and B also had the highest intubation rate, but blood group O was more hospitalized than other blood groups.