1. Background
Tracheal intubation is inevitable after general anesthesia, and its application has a direct relationship with the type and the length of the operation, the patient, and the operating room’s conditions (1). Voice hoarseness and sore throat are more irritating and intolerable for the patients, which increases the requirement for pharmaceutical interventions (2). The frequency of sore throat following tracheal intubation varies from 21 to 100% (1-3). The side effects increase the requirement for post-operative pharmaceutical interventions and higher care at inpatient units (4). Various pharmaceutical and non-pharmaceutical methods are utilized to reduce voice hoarseness and sore throat, with different success rates (5, 6). Novel methods and pharmaceuticals with the lowest level of side effects are increasingly drawing the attention of researchers and anesthesiologists since each method is associated with particular complications, and none can completely prevent the post-tracheal intubation sore throat (2-7).
The compounds in rosemary (carnosol and ursolic acid) have been successfully used as anti-inflammatory agents in most inflammation cases (8). So far, no side-effect associated with the rosemary plant has been reported, and various studies have suggested replacing chemical pharmaceuticals with this plant (9). Considering the benefits of the rosemary plant (10), researchers were motivated to investigate the anti-inflammatory effects of this agent to prevent post-tracheal intubation sore throat and, concurrently, discovered the most suitable method to treat the post-intubation sore throat and avoid the side effects of chemical pharmaceuticals (11). On the other hand, numerous studies have indicated that N-Methyl-D-aspartic acid (NMDA) receptors are also present in the peripheral nervous system besides the central nervous system (12, 13). Ketamine is the most frequently utilized NMDA receptor antagonist and is used extensively in general anesthesia.
2. Objectives
This study compared rosemary plants and ketamine gargles for voice hoarseness and sore throat following tracheal intubation.
3. Methods
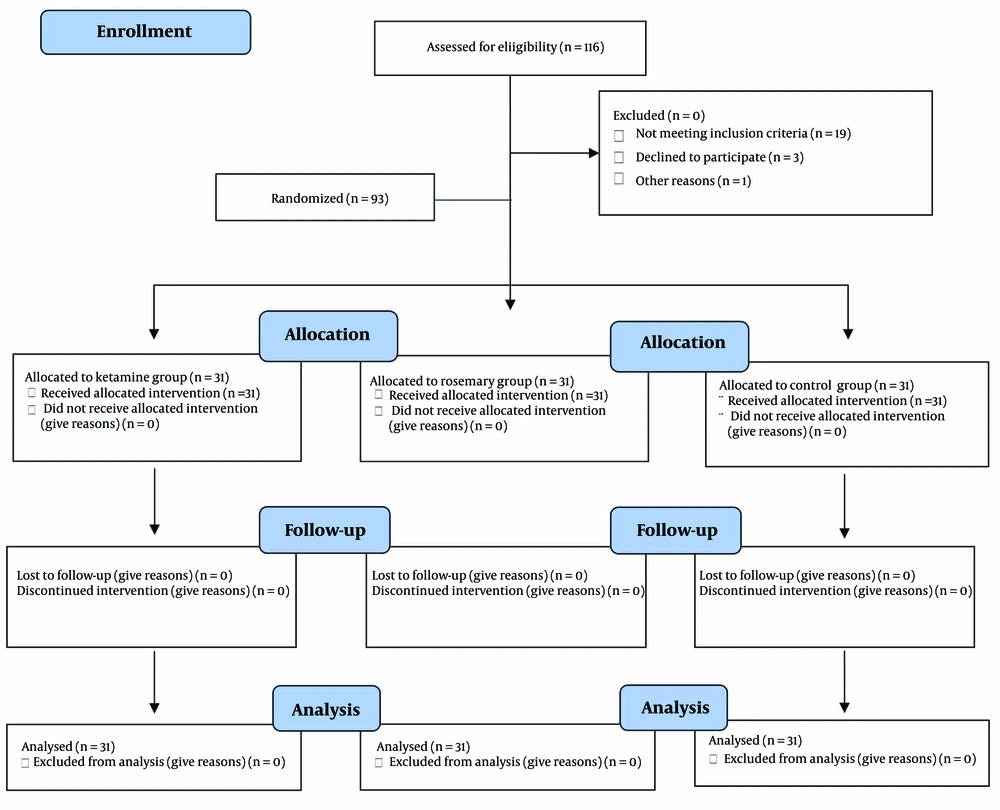
This randomized, triple-blind clinical trial (IRCT 20160307026950N50) was conducted in 18 months (2021 - 2022) at selected hospitals under the supervision of Isfahan University of Medical Sciences, Iran. The required sample was estimated as 116 individuals (31 individuals in each group), using the ratio comparison formula and considering a 95% confidence level, 80% power, sore throat frequency, and the lowest significant difference between the two groups (determined as 35%) (14). The inclusion criteria were candidates for surgeries with general anesthesia, patients of ASA1-2 classes, patients aged 18 to 65 years, patients’ consent to participate in the survey, and operations requiring supine intubation. The exclusion criteria included prolonged surgical duration (more than 3 hours), alteration in anesthesia method (due to any reason), change in routine surgical technique, severe bleeding and blood transfusion requirement during surgery, and severe hemodynamic disturbances during the surgery. The sampling was conducted using convenience sampling after obtaining permission from the Medical Ethics Committee of the Isfahan University of Medical Sciences (with ethical code: IR.MUI.MED.REC.1401.056). The participating patients were randomly allocated to three groups using Randomize Allocation software (14). The required number of participants for the control group was determined to be 54 individuals.
The following diagram includes the patient, which is shown in Figure 1.
3.1. Intervention Method
Participants were divided into three groups after obtaining the research permit from the Committee of Healthcare Ethics of the Isfahan University of Medical Sciences. Before the intubation and preemptive analgesia, the first group gargled the 30 mL solution made by the addition of 30 drops of rosemary (generic name R. officinalis) extract (produced by Fadak Sepahan Herbal Pharmaceutical Company) to 30ml of distilled water for 2 - 3 minutes before the general anesthesia. The second group gargled the solution by adding 40mg ketamine to 30ml normal saline, for 30s, 2 - 3 minutes before the anesthesia induction, and the third group (control) gargled 30ml distilled water, 2 - 3 minutes before the surgery. Every pharmaceutical was administered in a similar appearance and volume (equal volumes for gargling) 2 - 3 minutes before the intubation and initiation of the surgical process. Midazolam, fentanyl, nesdonal, and atracurium were used for induction. Isoflurane (2.1%) and O2 were used for maintenance (NO2 was not used). Every patient received the same fluid therapy protocol during NPO, following the 4 - 2 - 1 rule, while during surgery, it was the 10 - 8 - 6 rule without heating the fluid. Anesthesia induction was initiated with midazolam (0.1 mg/kg), fentanyl (1 g for each kilogram of body weight), atracurium (0.5 mg/kg), and sodium thiopental (5 mg/kg) injections after the patient was placed on the operating bed and connected to the standard monitoring system, including a pulse oximeter, capnography, electrocardiogram, and blood pressure cuff. Then, the anesthesia was continued with isoflurane, O2, and morphine (0.1 mg/kg) after the tracheal intubation to ensure the correct placement of the tube. Ventilation maintained ETCO2 at 35 - 45 normal level and SpO2 at 100%. Muscle relaxation was induced using atropine (0.20 mg/kg) and neostigmine (0.40 mg/kg) at the end of the operation. Patients were extubated after reversing and fully awakening and transferred to recovery. In the case of VAS scores higher than three in recovery, the patients received Apotel (15 mg/kg) to relieve pain.
The measurement methods for obtaining information included the Visual Analogue Scale (VAS) for pain, GRBAS (Grade of Hoarseness; Roughness, Breathiness, Asthenia, and Strain) auditory scale for the severity of voice hoarseness, and a questionnaire to evaluate the patient’s level of satisfaction. The pain intensity was measured using the VAS. The intensity of sore throat pain was recorded using the subjective Sore Throat Pain Intensity Scale (STPIS). The patients were asked to show the severity of their sore throat on the drawn line from 0 to 10 based on their pain intensity. The scores 0, 1 - 3, 4 - 6, and 7 - 10 indicated lack of pain, mild, moderate, and severe pain, respectively.
The therapist graded the level of the patient’s voice hoarseness on a 0 - 3 scale based on the Grade of Hoarseness; Roughness, Breathiness, Asthenia, and Strain (GRBAS) auditory scale designed by the Japan Society of Logopedics and Phoniatrics. The score 0 indicated normal voice without hoarseness, score 1 indicated weak, score 2 indicated moderate, and score 3 indicated high intensity. The patients’ satisfaction level from the effect of the administered drug on the reduction of sore throat pain intensity and voice hoarseness was evaluated based on a Likert scale survey question on a 1 to 5 scale. Score 1 indicated a lack of satisfaction, score 2 showed minimum satisfaction, score 3 revealed relative satisfaction, score 4 presented reasonable satisfaction, and score 5 represented complete satisfaction from the effect of the administered drug on the reduction of sore throat pain and voice hoarseness after the surgery. The variables were controlled and recorded within 24 hours after the surgery. This study was conducted as a triple-blind trial, in which the patients, physicians, and the individuals in charge of data analysis were unaware of the groups, drugs administered to the patients, and the study method.
The quantitative data were analyzed with ANOVA, and the chi-square test statistical test data were analyzed using SPSS software version 25. Tests with P-values lower than 0.05 were considered statistically significant.
4. Results
The results did not indicate significant differences between the patients' ages (P = 0.10), BMI (P = 0.64), and gender (P = 0.90). Table 1 presents supplementary information.
| Variables | Control; (n = 54) | Ketamine; (n = 31) | Rosemary; (n = 31) | P-Value |
|---|---|---|---|---|
| Age (y) | 37.86 ± 11.54 | 43.93 ± 16.15 | 43.16 ± 14.01 | 0.10 b |
| BMI | 26.19 ± 3.65 | 25.28 ± 4.80 | 25.70 ± 4.43 | 0.64 b |
| Anesthesia duration (min) | 135.02 ± 26.41 | 133.06 ± 27.91 | 128.90 ± 20.79 | 0.56 b |
| Surgery duration (min) | 121.76 ± 24.47 | 119.84 ± 24.64 | 115.65 ± 19.65 | 0.51 b |
| Recovery duration (min) | 107.07 ± 25.80 | 104.68 ± 25.85 | 104.42 ± 27.75 | 0.87 b |
| Gender | 0.90 c | |||
| Female | 22 (40.7) | 12 (36.7) | 13 (41.9) | |
| Male | 32 (59.3) | 19 (63.3) | 18 (58.1) |
a Values are expressed as mean ± SD or No. (%).
b One-way ANOVA.
c Chi-square test.
The results indicated no significant difference in hemodynamic changes, including the systolic blood pressure (P = 0.73), diastolic blood pressure (P = 0.97), SpO2 level (P = 0.06), and heart rate (P = 0.31) between the patients of the three groups.
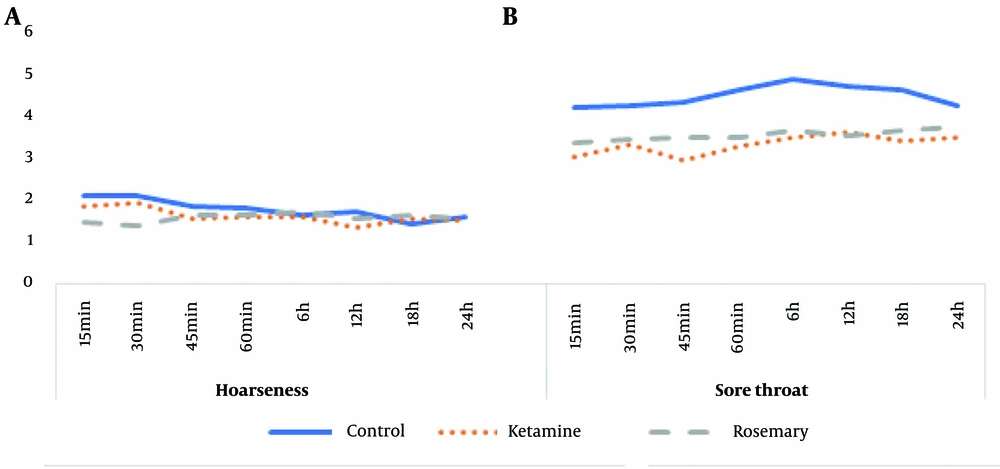
Table 2 represents the Analysis of Repeated Measures ANOVA of Differences in Voice Hoarseness and Sore Throat Over Time in Each Intervention Group.
| Parameters and Groups | 15 min | 30 min | 45 min | 60 min | 6 h | 12 h | 18 h | 24 h | P-Value |
|---|---|---|---|---|---|---|---|---|---|
| Hoarseness | 0.15 | ||||||||
| Control | 2.10 ± 0.863 | 2.12 ± 0.872 | 1.86 ± 0.700 | 1.82 ± 0.560 | 1.67 ± 0.595 | 1.75 ± 0.812 | 1.46 ± 0.798 | 1.42 ± 0.647 | |
| Ketamine | 1.88 ± 1.166 | 1.96 ± 1.207 | 1.56 ± 0.712 | 1.60 ± 0.764 | 1.62 ± 0.498 | 1.38 ± 0.590 | 1.57 ± 0.598 | 1.52 ± 0.512 | |
| Rosemary | 1.48 ± 0.511 | 1.39 ± 0.656 | 1.65 ± 0.647 | 1.65 ± 0.647 | 1.74 ± 0.619 | 1.57 ± 0.507 | 1.65 ± 0.487 | 1.57 ± 0.507 | |
| Sore throat | 0.008 | ||||||||
| Control | 4.22 ± 1.734 | 4.28 ± 1.742 | 4.35 ± 1.650 | 4.63 ± 1.815 | 4.89 ± 2.089 | 4.72 ± 2.08 | 4.63 ± 2.25 | 4.26 ± 2.13 | |
| Ketamine | 3.04 ± 1.098 | 3.32 ± 1.345 | 2.96 ± 1.136 | 3.28 ± 1.458 | 3.52 ± 1.475 | 3.64 ± 1.55 | 3.44 ± 1.53 | 3.52 ± 1.50 | |
| Rosemary | 3.39 ± 1.783 | 3.45 ± 1.786 | 3.52 ± 1.749 | 3.52 ± 1.823 | 3.68 ± 2.088 | 3.55 ± 2.12 | 3.68 ± 2.18 | 3.74 ± 2.17 |
a Values are expressed as mean ± SD.
Table 2 indicates a significant difference in voice hoarseness among the three groups during the 24 hours after the surgery (P = 0.001). However, the sore throat intensity of the rosemary group was significantly lower (P = 0.008).
Figure 2 illustrates the changes in voice hoarseness over time in each intervention group separately. The results are presented by moderating the effect of 15-minute intervals.
Table 3 presents the time of first pain sensation, pethidine administration, and patient satisfaction of each group.
| Variables | Control; (n = 54) | Ketamine; (n = 31) | Rosemary; (n = 31) | P-Value b |
|---|---|---|---|---|
| First time of pain (min) | 36.39 ± 16.11 | 38.23 ± 16.81 | 43.55 ± 11.19 | 0.11 |
| Consumable pethidine | 30.09 ± 11.14 | 26.45 ± 7.09 | 25.48 ± 3.94 | 0.03 |
| Satisfaction | 3.87 ± 1.05 | 4.42 ± .95 | 4.39 ± 1.08 | 0.02 |
a Values are expressed as mean ± SD.
b One-way ANOVA.
Table 3 indicates no significant difference in the time of first pain sensation between the three groups (P = 0.11). However, the mean pethidine administration of the control group was significantly higher (P = 0.03), and the satisfaction level of the control group was significantly lower (P = 0.02).
5. Discussion
The present study aimed to conduct a comparative investigation on rosemary and ketamine gargles’ effect on voice hoarseness and sore throat after tracheal intubation. The results indicated no differences in hemodynamic changes (including systolic blood pressure, diastolic blood pressure, SpO2 level, and heart rate) among the three groups. Various factors affect the post-operative sore throat, including age, BMI, anesthesia duration, surgery duration, recovery duration, and gender. This study did not indicate a significant difference between the demographic variables of the groups. Dehghani and Anvari demonstrated no difference between the age and anesthesia duration of their studied groups (placing a sterile gauze soaked in rosemary extract inside the patient’s throat and placing a sterile gauze soaked in distilled water inside the patient’s throat (15). The group matching was suitable, and the study had no confounding variables.
According to the present study, there were no significant differences in the voice hoarseness of the three groups during the 24 hours after the surgery. However, the sore throat intensity of the three groups was different during the 24 hours after the surgery, and the rosemary group indicated lower intensities than the ketamine and control groups. There are limited studies on using rosemary and ketamine extracts to prevent voice hoarseness and sore throat after intubation compared with the results of the current study. In this regard, Justo et al. found that proinflammatory cytokines levels increase, and the rosemary essence removes excess CO2 and decreases cell inflammation in laboratory environments where cells are exposed to supercritical conditions and accumulated CO2 (16). Asadizaker et al. revealed that topical ointment of rosemary reduces the incidence of catheter-related phlebitis caused by antibiotic therapy (17). Faridi Tazeh kand et al. studied the relationship between the ketamine spray on the tracheal tube’s cuff and the reduction of postoperative sore throat, cough, and voice hoarseness and indicated a significant decrease in the sore throat incidence in the ketamine group compared with the control group (18). According to Ahuja et al., nebulized ketamine significantly reduced the incidence and intensity of sore throat after intubation when used in conjunction with nebulized ketamine (19). Sanatkar et al. evaluated the effect of pretreatment with intratracheal ketamine on post-intubation sore throat among patients undergoing strabismus surgery and concluded that intratracheal ketamine can reduce post-operative sore throat and the requirement of analgesic drugs (20). Inconsistent with the current study's results, Dehghani and Anvari indicated that the incidence of sore throat among female patients who underwent surgery with difficult intubation and received rosemary herbal medicine was not different from that of the control group (8). In another study, Dehghani and MohammadiPour Anvari revealed that injection of rosemary extract into the patient’s throat after the intubation had no reducing effect on the sore throat as a frequent post-intubation complication (15). The differences between the mentioned study and the current research results can be attributed to the personal indices of the patient, the intubation period, and other causes. Carnosol, a compound in rosemary extract, has a high potential to reduce inflammation due to its anti-inflammatory and antioxidant effects. This compound may have contributed to the significant reduction in inflammation and subsequent decrease in the intensity of sore throat observed in the current study. Previous studies have revealed that chloroform and hexane extracts of rosemary have similar anti-inflammatory effects to indomethacin and reported identified anti-inflammatory compounds, including trientine, oleic acid, and micrometric acid (21).
The results of the current study indicated no differences between the time of the first pain sensation among the three groups. However, the mean pethidine administration in the control group was higher, and the satisfaction level of the control group was lower. Accordingly, intratracheal administration of ketamine and rosemary can probably control the patient’s pain and increase satisfaction, but the differences were insignificant. The similarity between the three groups may be due to the different ages of the test subjects, the difference in the pain threshold of the individuals, and the low concentration of rosemary and ketamine extract. Nevertheless, clinical trials have reported that topical application of ketamine in case studies of patients with neuropathic pains and cancer had an analgesic effect. Ghasemzadeh Rahbardar et al., in their research on an animal model, reported positive anti-inflammatory effects of this extract in reducing neuropathic pains (22). Tahoonian-Golkhatmy et al. also revealed that consuming rosemary capsules can effectively reduce pain duration, which plant can be utilized as a therapeutical method (23). The results of the mentioned study were in line with the current research. This finding can be contributed to the higher analgesic effect of ketamine compared with other anesthesia induction agents. Evidence suggests that ketamine occupies the narcotic receptors in the brain and spinal cord, which can cause some analgesic effects of ketamine. Interference with NMDA receptors may mediate general anesthesia effects and sometimes the analgesic effects of ketamine. According to preclinical studies, rosemary inhibits pain by interaction with opioid receptors and 5-hydroxytryptamine (5-HT1A) (24). Rosemary extract also demonstrated an effective analgesic activity through the 5-HT1A receptor regarding the endogenous opioids in the serotonergic system (25). On the other hand, rosemary’s solution contains carnosol and carnosic acid, which act as potent anti-inflammatory agents and anti-oxidants that reduce interleukin β and TNFα, cyclooxygenase-2 (COX-2) enzymes, and prostaglandin production. The analgesic effect appears related to the compounds’ antispasmodic and anti-prostaglandin impact (26).
The current study's limitations included the low concentration of the rosemary and ketamine extract and the lack of accurate information on the purity of the material, which did not consider the time consumed for intubation and the number of intubation attempts. The researchers recommend conducting further studies to investigate the effects of this drug in the form of a gel.
5.1. Limitations
Although gargling is an old and well-known way to relieve a sore throat, not everyone is equally capable of performing this technique correctly. This study sample was small, so further studies are required. Therefore, a study with a more significant number of samples is needed to compare ketamine and rosemary.
5.2. Conclusions
Rosemary and ketamine gargling did not affect the post-intubation voice hoarseness but effectively impacted the post-tracheal intubation sore throat intensity. Ketamine and rosemary gargling do not reduce patients' pain intensity, but they increase their level of satisfaction and help them better control their pain.