1. Introduction
Ralstonia pickettii is a rare non-fermentative gram-negative bacterium and a highly resistant bacterial species in natural environments (1, 2). Although this bacterium is environmental, it can be a rare nosocomial infection agent based on the limited studies reported worldwide. According to the case reports, most people infected by this bacterium include children, infants, hospitalized people, and autoimmune disease or immunodeficiency patients. This bacterium causes contamination of hospital water resources, sterile and injectable fluids, hospital devices, and surgical equipment (2). In this study, bloodstream infection caused by R. pickettii was identified in a hospitalized patient with uterus and cervical cancer and metastatic squamous cell carcinoma (SCC) to the colon who is undergoing surgery and blood transfusion. Since this bacterium and its infections are uncommon worldwide and this report is the first from our region, a case report was decided upon.
2. Case Presentation
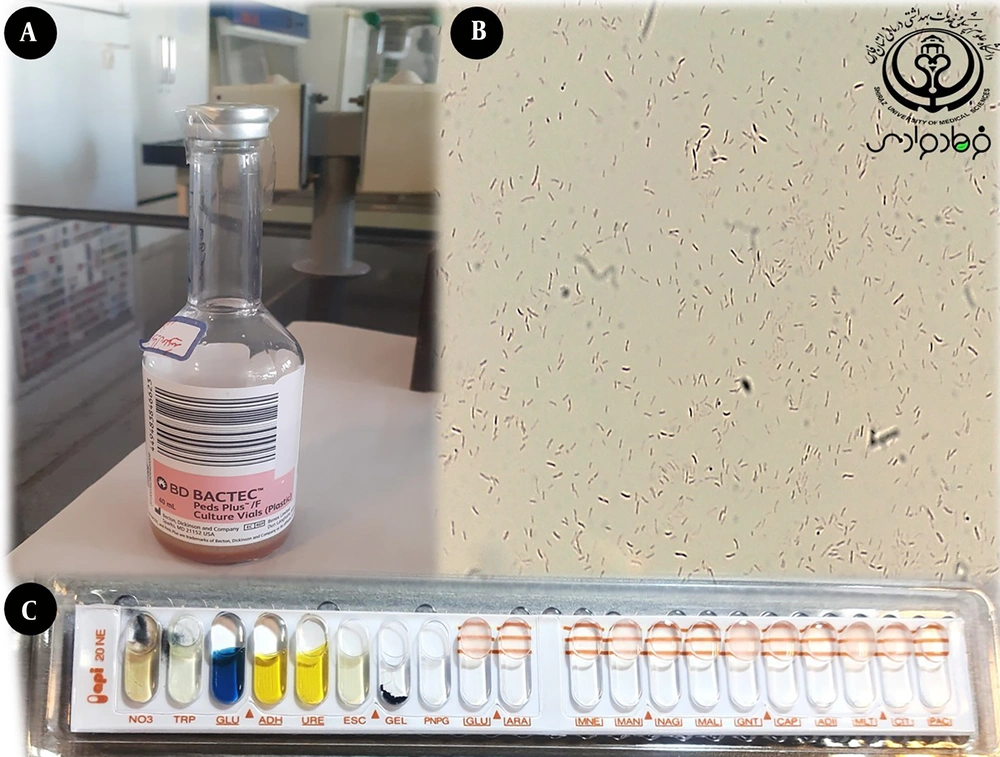
A 46-year-old woman was admitted to the general surgery department of the teaching hospital of Shiraz, Iran. She came with chief complaints of abdominal pain, nausea, and vomiting, and initial laboratory examinations documented White Blood Cell (WBC) 10.9 × 109 cells/L, Hemoglobin (Hb) 10.1 g/dL, neutrophils 70 %, Blood Urea Nitrogen (BUN) 12 mg/dL, and creatinine 1.2 mg/dL rates. Her colostomy did not work for four days with a rule out of obstruction. Before admission, she was under hysterectomy, colectomy, colostomy, and chemotherapy three weeks ago. Biochemistry results presented BUN 18 mg/dL and calcium 9 mg/dL levels one week after hospitalization, but the creatinine 1 mg/dL rate remained constant. Further, the patient received pantoprazole (PROTONIX I.V. 40 mg) and octreotide (100 mcg/mL) during hospitalization. Abdominopelvic sono showed gallbladder partially distended condition. In addition, the left kidney, containing a stone of about 7 mm, was detected without wall thickness and moderate stasis. Furthermore, diffuse thickening of the bowel wall and moderate to severe free fluid in the abdominopelvic cavity were seen. Moreover, the amount of Hb 9 g/dL suddenly decreased during hospitalization, and serological tests showed high C-Reactive Protein (CRP) quantitative 10 mg/L results. She received packed red blood cells twice during hospitalization and surgery. Ileostomy and release of adhesion bands were performed in laparotomy for severe adhesion bands and recurrences of tumors causing abstractions during surgery. In addition, the procalcitonin measurement results of 2.6 ng/mL and a small amount of CRP of 12 mg/L indicated a systemic infection. Two consecutive blood cultures using the BD BACTEC™ FX Instruments were positive for the patient, and the content of BACTEC bottles was extracted for culture and laboratory examination (Figure 1). The culture results indicated pinpoint non-fermenting colonies without hemolysis after a 48‐h incubation at 37°C on Mac Conkey Agar and blood agar in aerobic condition. Gram staining showed gram-negative bacilli with oxidase positive reactions, gelatin liquefaction, resistance to Polymyxin B (300 U disk) or Colistin (1 µg disk), and inability to lysine decarboxylation. This characteristic was a sign of bacteremia with R. pickettii. In addition, bioMérieux API 20NE was used to confirm R. pickettii (Figure 1). Antibiotic susceptibility testing (AST) for R. pickettii is performed using the Kirby–Bauer disk diffusion method using CLSI 2021 guidelines and antibiotics that are commonly prescribed in medical centers (3, 4). AST results for R. pickettii are characterized in Table 1. According to AST reports, Meropenem (1 g/Q8h/IV) was prescribed for the patient. Fortunately, the blood culture results were negative after 14 days after starting antibiotic treatment. Based on the documentation and observations about the possibility of contamination of hospital equipment, including surgical instruments and equipment used in blood transfusion, the mentioned patient may have been infected with R. pickettii during surgery or received packed red blood cells. Fortunately, rapid diagnosis of bacteremia caused by microorganisms and rapid treatment saved the patient from further complications such as sepsis. Fortunately, in this report, R. pickettii bacteremia was treated with the Meropenem antibiotic. Furthermore, ciprofloxacin was prescribed for the patient after discharge from the hospital. Finally, the patient left the hospital on her own accord.
| Antibiotic Agents | |
|---|---|
| Susceptible | Resistant |
| Ampicillin-sulbactam (10/10 µg) | Amikacin (30 µg) |
| Cefepime (30 µg) | Ampicillin (10 µg) |
| Cephalexin (30 µg) | Amoxicillin-clavulanic acid (20/10 µg) |
| Ciprofloxacin (5 µg) | Ceftazidime (30 µg) |
| Ceftriaxone (30 µg) | Cefixime (5 µg) |
| Cefotaxime (30 µg) | Chloramphenicol (30 µg) |
| Meropenem (10 µg) | Gentamicin (10 µg) |
| Levofloxacin (5 µg) | Tobramycine (10 µg) |
| Piperacillin/Tazobactam (100/10 µg) | |
| Co-Trimoxazole (25 µg) | |
| Tetracycline (30 µg) | |
| Tigecycline (15 µg) | |
Antibiotic Susceptibility Test Results for Ralstonia pickettii
3. Discussion
Although Ralstonia is an environmental and resistant bacterial agent, which can rarely cause infection in humans, recently, this bacterium has been classified in the family Burkholderiaceae, rRNA group II, based on DNA‐rRNA hybridization. Ralstonia pickettii was introduced as a type of species that is rarely associated with human infections. Although the virulence factors and pathogenesis of Ralstonia are not completely clear, Ralstonia is a rare cause of hospital infection, and its infections are mostly related to its ability to form biofilm in medical equipment and hospital instruments. The biofilm formation in this bacterium is due to a quorum sensing and robust signal exchange system. This system is probably the most critical virulence factor for pathogenesis and resistance in harsh environmental conditions (4, 5). According to various case reports, Ralstonia is associated with catheter-related bacteremia, pneumonia in cystic fibrosis patients, osteomyelitis, hemoperitoneum infection, recurrent meningitis, neonatal sepsis, native valve endocarditis, and peritoneal fluid infection after internal surgery. People at risk for this bacterium include newborns, infants, children, hospitalized patients with autoimmune disease, immunodeficiency or immunocompromised patients, and patients hospitalized in oncology units and infectious departments (5-9). Further, Ralstonia is responsible for pollution in pediatric peritoneal dialysis, haemato-oncology wards, infusion-related septicemia in the oncology department, an outbreak in a pediatric hospital, sepsis in a hemodialysis patient, cancer institutions, community-acquired pneumonia (6-15). Since R. pickettii is competent in the formation of biofilm in medical equipment and it can be considered the primary source of the contamination of intravenous fluids, distilled water, heparin, respiratory care solutions, hemodialysis water, and sterile saline in the hospital, operating theater, and operating room equipment (10-15). As a result, transferring this bacterium to patients during common surgical operations, blood transfusions, hemodialysis, and plasmapheresis can lead to blood infection and sepsis, especially in cancer patients (14, 15). Equally, the present study is the first report of the detection of R. pickettii bloodstream infection in a hospitalized patient with uterus and cervical cancer with metastatic squamous cell carcinoma to the colon. Although different studies have mentioned immunocompromised patients as the main population at risk for R. pickettii bacteremia, the results indicated that patients with uterus and cervical cancer are also susceptible to R. pickettii bacteremia after surgery and blood transfusion. The mentioned patient may have been infected with R. pickettii during hysterectomy, colectomy, colostomy, and laparotomy surgery or during receiving packed red blood cells by polluted intravenous needle, rubber tube, and preparing the Y tube with contaminated normal saline. Hence, recognizing the source of infection can be helpful in appropriate infection control, treatment, and prevention. Health workers, nurses, and physicians, especially in the neonatal or pediatric intensive care units, operating theaters, and blood transfusion units, should be conscious and learn about the transmission routes of Ralstonia among hospital personnel and patients. In addition, blood transfusion, plasmapheresis, hemodialysis, appropriate hand hygiene, sterility of the infusion devices, surgical instruments, including cutting and dissecting, grasping and holding, and hemostatic Instruments must be controlled during common surgical operations. Moreover, the germ-freeness of the extracorporeal devices and catheter care should constantly be monitored, especially for patients with cancer diseases, immunocompromised, and infants under blood transfusion or common surgical operations. Nevertheless, there is no specific instruction for AST and standard therapeutic guidelines for Ralstonia. Some studies have shown that Aminoglycosides and Carbapenems have successfully treated this agent. Similarly, in this study, R. pickettii bacteremia was treated after Meropenem prescribing. Laboratories play an essential role in diagnosing and preventing Ralstonia species. Although not all laboratories worldwide may have diagnostic facilities such as the BACTEC system, medical centers and hospitals should prepare the minimum facilities for phenotypic diagnosis through bioMérieux API 20NE and culture-based methods. Finally, the contamination of medical devices by Ralstonia should be followed periodically, especially in the dialysis departments and operating rooms, according to the hospital's infectious quality control program.
3.1. Conclusions
Based on the results, rare cases of nosocomial R. pickettii bloodstream infection were reported in hospitalized patients with uterus and cervical cancer with metastatic squamous cell carcinoma to the colon under surgery and blood transfusion. Nurses, laboratory experts, and physicians should consider the nosocomial infection of Ralstonia in cancer departments, especially during common surgical operations and blood transfusions, especially for cancer patients. Furthermore, appropriate infection control and prevention of infectious agent spread in medical devices, hospital solutions, catheters, and surgery equipment in hospitals and medical centers are necessary.