1. Background
Preterm birth is defined as birth before the 37th week of pregnancy (1), which is classified into three subgroups, extremely preterm (< 28 weeks), very preterm (28 - 32 weeks), and moderate preterm (32 - 37 weeks) (2). Preterm birth accounts for 3.1% of the global burden of diseases (3). Preterm birth in Iran has been estimated to be a total of 10% (4).
Cesarean section (C-section) is increasing worldwide, making it a global concern (5, 6). This trend in Iran is also rising, especially in private hospitals (7). The World Health Organization does not consider C-section to be more than 10% beneficial for the mother and baby (8). Meanwhile, the C-section rate in Iran is estimated at 48% (9). The literature generally states that vaginal delivery (VD) is a potential risk for neonatal mortality for preterm infants, and C-section serves as a preventive strategy for its reduction (10). However, there is controversy regarding the effect of the mode of childbirth on the death of preterm infants (11). Although C-section may reduce neonatal death, they can increase maternal morbidity and mortality (12, 13). A study in Brazil showed that C-section is associated with an increased risk of infant mortality unless there is a clear indication for the procedure (14).
Many factors predict C-section in preterm birth. A large cross-sectional study showed that the mother’s age, socioeconomic status, body mass index, parity, type of pregnancy, preeclampsia, infant height, and baby’s head circumference are associated with C-section in Tehran, Iran. Sometimes, C-section is the preferred procedure of mothers and doctors to save the baby (15, 16). A study in preterm neonates showed that women who delivered vaginally were younger, had lower rates of hypertensive disorders and diabetes mellitus, and had higher rates of drug abuse as compared to those who delivered by C-section. Neonates who were born by VD had higher birth weights and a lower rate of SGA than those who were born by C-section. However, VD neonates had higher Apgar scores, as compared with C-section, the neonatal composite outcome was similar between the two modes of delivery (17). The factors associated with C-section (15, 18, 19) have been extensively addressed, but factors associated with C-section in preterm birth are not well documented.
2. Objectives
Accordingly, this paper evaluates the factors associated with C-section in preterm births at a Tertiary Hospital in Rasht, the center of the province of Gilan, Iran.
3. Methods
3.1. Study Design and Setting
This retrospective medical record review was conducted on neonatal subjects born between 2017 and 2022 at the Al-Zahra Maternity Hospital, Rasht, Iran, to determine the factors associated with C-section among preterm births.
Rasht is a populous city in the north of Iran equipped with one public referral maternity hospital. This hospital has two wards for neonatal hospitalization (Premature Neonate Unit and Neonatal Intensive Care Unit). Most pre-term births are performed because Al-Zahra is a tertiary hospital. According to Rezaeian et al.(20) which reported the prevalence of preterm delivery to be 7.1% and with an error of 5% using ratio estimation, the minimum sample size was determined to be 1126 people.
3.2. Sampling, Data Collection Procedure, and Tool
All medical records of neonates admitted between May 2017 and March 2022 were included. Two midwives and a trained intern used a structured checklist to collect data from the medical records of 1161 preterm infants. The checklist was adapted after reviewing various literature on similar studies. In this study, the characteristics of the mother's age, gestational age, pregnancy and childbirth history, C-section cause, and neonate complications were investigated.
3.3. Ethics Considerations
Ethics approval was obtained from the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (IR.GUMS.REC.1399.302). All reviewed medical records had a signed informed consent form for the use of patient medical data completed by the neonates' parents.
3.4. Data Analysis
The gathered data were analyzed in SPSS software version 25. The chi-square and Fisher's exact tests were performed to analyze the relationships between nominal scale variables. Factors with ≤ 0.2 significant level in the bivariate logistic regression analysis were considered in the multivariable logistic regression analysis. The multivariable analyses were conducted using multiple logistic regression models at a 95% confidence interval (CI) and P < 0.05 statistical significance.
4. Results
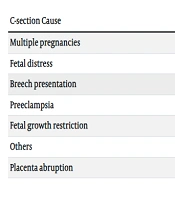
The mean age of mothers was 30.90 ± 6.24 years old. Sixteen of the reviewed records were excluded from the study (five revisits and eleven out-of-hospital admissions). Finally, 1145 medical documents were imported into the study. Most of the preterm births (77%) were C-sections of which, 44.4% were repeated. The rest were performed primarily due to multiple pregnancies and fetal distress. Table 1 presents the C-section causes among mothers who had their first C-section.
| C-section Cause | No. (%) |
|---|---|
| Multiple pregnancies | 154 (33.8) |
| Fetal distress | 145 (31.9) |
| Breech presentation | 67 (14.7) |
| Preeclampsia | 34 (7.5) |
| Fetal growth restriction | 23 (5.1) |
| Others | 21 (4.6) |
| Placenta abruption | 11 (2.4) |
Table 2 represents the maternal and neonatal characteristics of neonates based on the mode of childbirth. The primary analysis showed a significant difference between the mother's age (P < 0.001), gestational age (P < 0.001), abortion history (P = 0.007), hypertension (P < 0.001), preeclampsia (P = 0.003), fetal growth restriction (P = 0.001), fetal distress (P < 0.001), meconium (P = 0.013), and the preterm birth cause (P < 0.001) with the mode of childbirth (Table 1).
| Variables | Vaginal Delivery (N = 263) | C-section (N = 882) | P-Value a |
|---|---|---|---|
| Age | < 0.001 | ||
| < 35 | 184 (24.4) | 570 (75.6) | |
| ≥ 35 | 47 (14.6) | 275 (85.4) | |
| Infertility | 0.054 | ||
| Yes | 36 (17.1) | 174 (82.9) | |
| No | 215 (23.3) | 708 (76.5) | |
| History of abortion | 0.007 | ||
| Yes | 39 (15.8) | 208 (84.2) | |
| No | 212 (23.9) | 674 (76.1) | |
| History of death child | > 0.999 | ||
| Yes | 17 (21.5) | 62 (78.5) | |
| No | 234 (22.2) | 820 (77.8) | |
| Hypertension | < 0.001 | ||
| Yes | 41 (13.8) | 257 (86.2) | |
| No | 210 (25.1) | 625 (74.9) | |
| Preeclampsia | 0.003 | ||
| Yes | 12 (11.1) | 96 (88.9) | |
| No | 239 (23.3) | 786 (76.7) | |
| Diabetes | 0.085 | ||
| Yes | 63 (18.8) | 272 (81.2) | |
| No | 188 (23.6) | 610 (76.4) | |
| Gestational age (w) | < 0.001 | ||
| ≤ 28 | 41 (49.4) | 42 (50.6) | |
| 29 - 32 | 50 (25.5) | 146 (74.5) | |
| ≥ 33 | 159 (19.4) | 659 (80.6) | |
| Sex | 0.885 | ||
| Female | 113 (22.3) | 394 (77.7) | |
| Male | 136 (22.7) | 462 (77.3) | |
| Birth weight (gr) | 0.118 | ||
| < 2500 | 156 (23.1) | 518 (76.9) | |
| ≥ 2500 | 71 (18.9) | 304 (81.1) | |
| Congenital malformation | 0.428 | ||
| Yes | 10 (27) | 27 (73) | |
| No | 241 (22) | 855 (78) | |
| Fetal growth restriction | 0.001 | ||
| Yes | 18 (12.1) | 131 (87.9) | |
| No | 233 (23.7) | 751 (76.3) | |
| Fetal distress | < 0.001 | ||
| Yes | 0 (0) | 132 (100) | |
| No | 251 (25.1) | 750 (74.9) | |
| Meconium | 0.013 | ||
| Yes | 5 (8.8) | 52 (91.2) | |
| No | 246 (29.9) | 830 (77.1) | |
| Preterm birth cause | < 0.001 | ||
| Spontaneous | 232 (27.4) | 616 (72.6) | |
| Iatrogenic | 13 (6.1) | 201 (93.9) |
a Chi-square or Fisher's exact test.
b Values are expressed as No. (%).
The variables with P < 0.2 were introduced to the logistic regression model. The analysis identified the following as factors associated with C-section: The mother's age (P < 0.001), gestational age (P < 0.001), neonate's weight (P = 0.042), infertility history (P = 0.042), abortion history (P = 0.006), and preterm birth cause (P < 0.001) (Table 3).
| Variables | β | SD | Wald | P-Value | OR (95% CI) |
|---|---|---|---|---|---|
| Mother's age | 0.063 | 0.015 | 18.186 | < 0.001 | 1.06 (1.034, 1.09) |
| Gestational age | 0.216 | 0.036 | 35.794 | < 0.001 | 1.24 (1.15, 1.33) |
| Birth weight | -0.464 | 0.229 | 4.125 | 0.042 | 0.62 (0.40, 0.98) |
| Hypertension | 0.196 | 0.204 | 0.015 | 0.430 | 1.21 (0.74, 1.97) |
| Preeclampsia | 0.026 | 0.467 | 0.003 | 0.955 | 1.02 (0.41, 2.56) |
| Diabetes | 0.025 | 0.204 | 0.015 | 0.902 | 1.02 (.068, 1.52) |
| Infertility history | 0.461 | 0.228 | 4.083 | 0.043 | 1.58 (1.01, 2.48) |
| Abortion history | 0.636 | 0.232 | 7.481 | 0.006 | 1.88 (1.19, 2.97) |
| Fetal growth restriction | -0.162 | 0.313 | 0.267 | 0.605 | 0.85 (0.46, 1.57) |
| Fetal malformation | -0435 | 0.427 | 1.039 | 0.308 | 0.64 (0.28, 1.49) |
| Preterm birth reason | 1.609 | 0.380 | 17.957 | < 0.001 | 4.99 (2.37, 10.53) |
5. Discussion
Given the high rate of C-sections in the study setting in recent years and public preference for C-section to vaginal delivery due to attitudinal and operational barriers (21), the C-section rate was high among preterm births. The most common reason for the C-section procedure was repeated C-sections. Mother's age, gestational age, birth weight, infertility and abortion history, and preterm birth were found to be the factors associated with C-section in preterm births.
5.1. Neonatal Factors
The results of this study indicated that the number of C-section operations increases as the gestational age increases with each week, which can be attributed to the fact that the increase in gestational age in preterm births increases neonate survival chance. Doctors accept the risk of C-section for the mother more easily. In line with this finding, a study on term infants also found that older gestational age is a risk factor associated with an increased risk of C-section (22).
Birth weight is another neonatal factor that predicts C-section. Preterm neonates ≥ 2,500 g were 1.5 times more likely to deliver through C-section than neonates < 2,500 g. This finding is in line with the study of Alhassan in Ghana, which indicated that the odds of birth by C-section decreased among pregnant women with low birth weight (23).
5.2. Maternal Factors
The current study found that mothers ≥ 35 years old were more likely to have C-section compared to mothers < 35 years old. This finding broadly supports the work of other studies in this area. Manyeh et al. found that mothers aged 30 - 34 years were more likely to have C-section compared to those < 20 years (22). Another study showed that maternal age ≥ 35 years is one of the factors associated with increased odds of C-section (24).
In addition, a history of infertility and abortion were predictors of C-sections. Another large study in southwest Iran also showed that previous abortion and previous infertility were the risk factors for C-section (25). Sinnott et al. also concluded that a prior history of miscarriage is a predictor for C-section (26). On the other hand, some studies have shown that C-section is one of the risk factors for infertility and abortion (27, 28). This cause-and-effect relationship cannot be definitively determined due to the study's cross-sectional nature. However, abortion and infertility are predictors of C-sections after splitting repeated C-sections. Maybe women with a history of abortion and infertility and their doctors are more concerned about saving the baby and are more inclined to choose C-section.
5.3. Iatrogenic Preterm Birth
Although hypertension and preeclampsia were found to have a stronger association with C-sections in the primary analysis, no association was identified between these conditions and C-sections in the regression analysis results. The iatrogenic preterm births were about five times more likely to take the C-section procedure than spontaneous preterm births. By the present results, Dehaene et al. found higher C-section rates in iatrogenic preterm births (29). Considering the role of iatrogenic preterm birth in C-sections, it seems that a possible reduction in iatrogenic births could decrease the C-section rate. In addition, iatrogenic preterm births had a higher rate of neonatal death at discharge compared to spontaneous preterm births. In general, some neonatal complications are associated with etiologic types of preterm birth. Thus, proper management of different etiological subgroups of preterm births can prevent adverse neonatal outcomes.
This study has several strengths, including a large sample of preterm births in a referral tertiary hospital. However, several limitations should be noted. First, some key factors related to C-sections (the mother's level of education and insurance status) were not explored since the data were mainly gathered from only the medical records of neonates. Second, a definite opinion about the causal relationships can be made due to the cross-sectional design. Third, missing data may have affected the results due to the incompleteness of some of the neonates’ medical records.
5.4. Conclusions
The incidence of C-sections is significant among preterm births in the Alzahra tertiary care hospital. Mother's age, gestational age, birth weight, infertility and abortion history, and iatrogenic preterm birth were the factors associated with C-section in preterm births. Physicians must pay attention to these factors in managing preterm births. In addition, preterm birth management based on their etiology can prevent adverse neonatal outcomes.