1. Introduction
Acute scrotum denotes conditions characterized by a new onset of scrotal pain, erythema, and swelling. In the case of the acute scrotum, mainly observed among male adolescents, the patient should be assessed for scrotal torsion, epididymal-orchitis, and torsion of the testicular appendix (1). It is critical to distinguish testicular torsion from other causes of acute scrotum because of its limited golden time to rescue. Epididymitis is defined as inflammation or infection of the epididymis and is a common cause of acute scrotum in pediatric patients. Orchitis is the inflammation of the testis and is usually unilateral (2, 3). At a young age, when sexually transmitted disease (STD) is not a concern, the causes of epididymal-orchitis might be urinary tract infection as well as genitourinary anomalies (4). Although epididymal orchitis might be caused by bacterial urinary tract infection, viruses like mumps and rubella are among the main causes. Reports exist of cases of orchitis after the measles, mumps, and rubella (MMR) vaccine (5, 6). Bacteria, as causative agents of STD, can also cause orchitis in sexually active males (7). Primary autoimmune orchitis is defined as an autoimmune involvement of the testes characterized by the presence of specific anti-sperm antibodies (ASA) (8, 9). Testicular vasculitis might be associated with autoimmune vasculitis such as polyarteritis nodosa, Behçet's disease, and Henoch-Schönlein purpura (8-10). Limited cases of testicular torsion have been reported so far in patients suffering from sickle cycle anemia (11).
Sometimes, there is an overlap between symptoms of testicular infarction and testicular torsion, making the differentiation difficult. As a potentially severe complication of epididymitis in the context of trauma, testicular infarction and ischemia might occur.
Significant complications of the MMR vaccine include aseptic meningitis or temporary low platelet count. Swollen salivary glands, a maculopapular rash, feeling unwell, a high temperature for 7 to 11 days, and small joint arthralgia 2 to 3 weeks after the vaccination can occur. Overall, the MMR vaccine is very safe and effective. Two doses of this vaccine are about 97% effective at preventing measles. Involvement of the testis is sporadic (12). Literature in medical databases (PubMed, Scopus, International Statistical Institute, Web of Science, Cochrane, and Embase databases) has shown very limited cases occurring after vaccination in late adolescence. There was only one report of testicular ischemia as a complication of epididymal-orchitis, in which testicular infarction happened in a young man who received the MMR vaccine a few days ago (12). We found no report of epididymal-orchitis following MMR vaccination at a young age. Here, we present an 18-month-old male infant with epididymal orchitis followed by testicular torsion after the MMR vaccine.
There was only one report of testicular ischemia as a complication of epididymal-orchitis, in which testicular infarction happened in an infant who had just received the MMR vaccine, which is a rare event (2). We found no report of epididymal-orchitis following MMR vaccination at a young age. Here, we present an 18-month-old male infant with epididymal orchitis followed by testicular torsion after the MMR vaccine.
2. Case Presentation
Here, we report on an 18-month-old male infant who presented with a one-day history of gradually worsening painful left scrotal swelling following a booster dose of MMR. He was the first product of a non-consanguineous marriage. He was normal regarding all developmental milestones. All vaccinations were up to date. There were no signs of upper respiratory tract involvement in the days before vaccination. He was a circumcised boy with no history of prior urinary tract infection. There was no history of testicular torsion or genital anomaly in any of his family members.
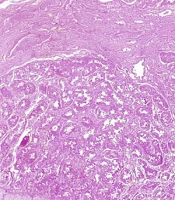
His parents noticed some redness in the left scrotal area the day after vaccination. They thought it might be due to an insect bite or diaper rash and did not seek medical advice. On the following day, erythema worsened, and the infant became irritable. The patient was referred to an educational and therapeutic center because of increased restlessness and lack of response to self-administered treatment with topical ointments. His vital signs were normal. He did not have nausea or vomiting. No history of trauma and urethral discharge was detected. Genital examination revealed a red, tender, indurated left testicle with normal cremasteric reflex. A color Doppler sonography was performed to rule out testicular torsion. Both testes were detected with normal size. The left testis was a little bit heterogeneous compared to the right side. According to the report, testicular vascularity evaluation was unreliable regarding young age and testicular immaturity. The left epididymis showed an increased echo pattern and vascularity compared to the right side. No evidence of hydrocele was detected in either scrotum. The imaging result was not in favor of testicular torsion. An oral antibiotic was administered. Two days later, the patient was reexamined because of no response to oral treatment. Examination showed that the left testicle was erythematous and indurated (Figure 1). The child was very restless. Another emergency color Doppler ultrasound was requested, revealing severe inflammation with a heterogenic pattern and decreased vascularity in the left epididymis. A significantly increased thickness in the left scrotal wall and left spermatic cord was accompanied by mild hydrocele. The left testicle was inflamed and showed a heterogenic and striated echo pattern. No blood flow was detected in the left testicle compatible with the testicular infarct. The right testicle was of normal size, had a parenchymal echo, and had a smooth, soft contour. No evidence of solid or cystic lesions in any testicles was seen. The epididymis and spermatic cord on the right side appeared normal. The patient was referred to a pediatric surgeon.
2.1. Surgical Exploration
The appearance of the left scrotum was completely edematous and erythematous. There were about two rounds of intravaginal torsion (Figure 2). The left testicle looked firm and dark in color. The spermatic cord vessels were thrombotic in appearance, and the testicular appendix seemed completely necrotic. The left testicle was removed (Figure 3). Orchidopexy of the right side was performed to preserve the right testicle, which was normal in appearance.
2.2. Pathologic Evaluation
2.2.1. Macroscopic View
The specimen was received in formalin and consisted of a piece of reddish-brown testis tissue 1.5 × 1.3 × 1.3 cm along with an attached spermatic cord 1cm long and 0.6 cm in greatest diameter. On cut sections, the testis shows a dark-red solid cut surface with a soft consistency and the gross appearance of hemorrhagic infarction.
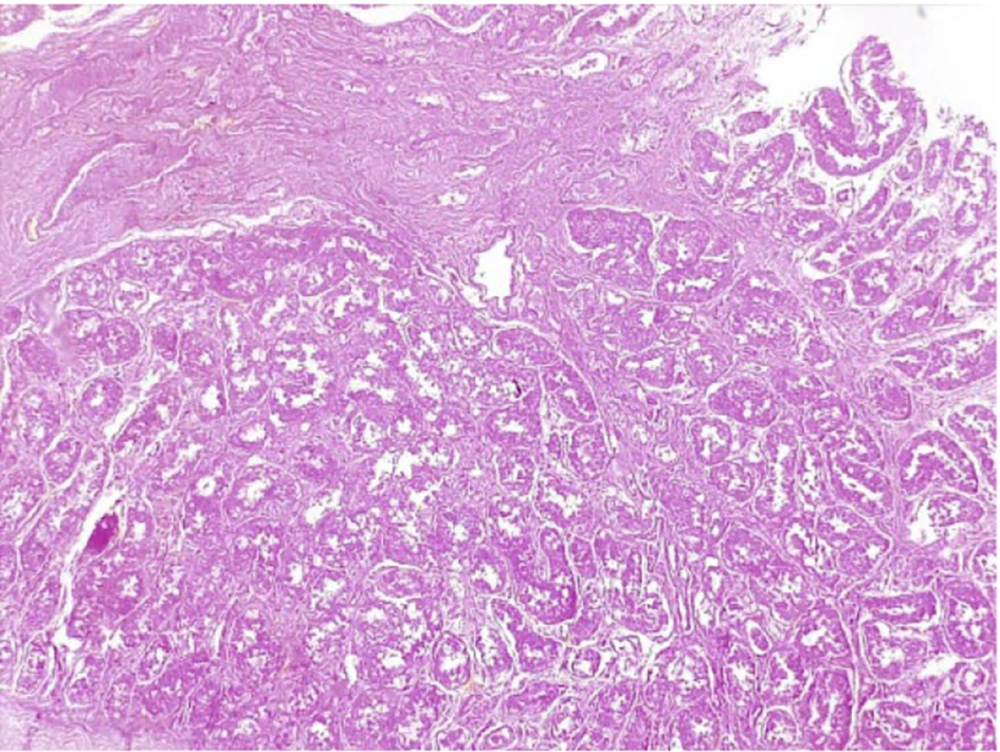
2.2.2. Microscopic View
Sections show testis tissue with marked vascular congestion and extensive areas of hemorrhagic infarction and necrosis. Shadows of infarcted seminiferous tubule architecture and foci of hemosiderin-laden macrophage deposition are evident. The spermatic cord surgical margin is intact. There is no evidence of malignancy in this specimen (Figure 4).
3. Discussion
A spectrum of conditions affect the scrotum, varying from incidental findings to pathologic causes requiring urgent diagnosis and treatment (13, 14). The most common causes of acute scrotal pain in childhood and adolescence include testicular torsion, torsion of the testicular appendage, and epididymal-orchitis. Testicular torsion is the most important because of the danger of testicular loss. Testicular torsion might be intravaginal or extra-vaginal. Intravaginal torsion results from the inadequate fixation of the testis to the tunica vaginalis through the gubernaculum testis. Bell clapper deformity is the most common abnormality in which testicular attachment to the tunica vaginalis is lost and is associated with increased mobility and transverse lying of the testis in the scrotum (13, 15).
Necrosis of the testis occurs due to impaired blood supply to the tissue caused by torsion of the spermatic cord vessels or infarction in the testicular tissue itself. In this case, a necrotic testicle was observed during surgery, which had occurred in the context of two rounds of torsion. There is sometimes an overlap between symptoms of testicular infarction and testicular torsion. Radiological and pathological evaluations cannot distinguish them from a few cases of testicular infarction after epididymal-orchitis have been reported (2).
Neonatal testicular torsion rarely occurs within 30 days of delivery. The disease is non-acute even if it happens during pregnancy, but it is generally detected during the immediate postpartum period or the first neonatal examination (16, 17). Postnatal onset torsion occurs after birth. In this case, testicles are normal at the initial physical examination. There is a possibility that it could lead to vascular compromise and ischemia. Necrosis and testicular loss will ensue without timely correction (16). Epididymo-orchitis can occur in males of various age groups. In most cases, epididymitis typically resolves with antibiotics, analgesics, and supportive measures such as rest, elevation of the scrotum, and applying ice packs to reduce swelling and discomfort. There are typically no long-term complications (18). Complications are preventable, and most patients recover without any sequelae, except for rare cases of testicular atrophy and sterility. However, there are rare reported cases of testicular torsion that have been attributed to increased testis volume (19). There is no need to consult in most cases except in cases with abscess formation or immune-compromised patients (5).
While it is commonly associated with infections (20), there have been anecdotal reports suggesting a potential association between the MMR vaccine and the subsequent occurrence of epididymal-orchitis (12, 21). The MMR vaccine contains freeze-dried, live, attenuated viruses and has been extensively studied and proven to provide long-lasting immunity against measles, mumps, and rubella (22). Measles, mumps, and rubella vaccine is now used routinely by national immunization programs, and the morbidity of infections caused by these three viruses has dramatically declined. There have been isolated reports of epididymal orchitis following its administration, while the MMR vaccine is generally well-tolerated (12, 21). Such reports are rare and should be considered within the broader context of the vaccine's overall safety profile and its substantial benefits. The benefits of the MMR vaccine, including its ability to protect against potentially severe diseases, far outweigh the potential risk of epididymal orchitis (23). Aseptic meningitis is the most frequent adverse event after mumps vaccination (0.0005 - 0.00005%), whereas the frequency of orchitis is very low (24).
Abdelbaky et al. reported a case of an 18-year-old man who presented with painful scrotal swelling within eight days after MMR vaccination. Finally, he was diagnosed with a diagnosis of epididymal-orchitis after a Doppler sonographic evaluation (12).
A 12-year-old boy developed persistent right testicular pain after trauma, accompanied by nausea, vomiting, and gradual swelling of the right scrotum. Scrotal Doppler sonography showed the right epididymitis, right scrotal wall swelling, and right testicular torsion. He underwent emergency scrotal exploration. During the operation, only testicular ischemia but no testicular torsion was reported. After decompression, the testicular blood flow was restored. This case indicated that acute epididymal-orchitis could cause secondary testicular ischemia under the influence of multiple factors. This study revealed that sonography and MRI scans are more sensitive for early ischemia detection than scrotal color Doppler sonography (2).
Kanda et al. reported a 35-year-old man with right orchitis two weeks after mumps vaccination. Unlike our case, the examinations and paraclinical evaluations did not show torsion (24).
Clifford et al. reported three cases of scrotal swelling after MMR vaccination. The first one was a 37-year-old man who presented with bilateral testicular pain and swelling three days after the MMR vaccine. The sonographic evaluation was consistent with orchitis. The second case was a 36-year-old man with unilateral scrotal swelling 48 hours after MMR vaccination. He was diagnosed with nonspecific inflammation in ultrasonography. The last case was a 12-month-old infant presented with redness and swelling of both testicles within two weeks of MMR vaccine. The symptoms gradually resolved within three days without further workup (21). Related to the above cases, Horiguchi and Uchida described a 26-year-old man with complaints of high-grade fever and right testicular pain and swelling after the mumps vaccine, which improved during seven days of supportive treatment (25).
In this regard, Suzuki et al. also reported that a 16-year-old male was admitted because of acute orchitis with high fever and painful swelling of the right testis 12 days after MMR vaccination (26).
The exact mechanism underlying the potential association between the MMR vaccine and epididymal orchitis is not fully understood. Numerous factors can trigger inflammation, which is believed to be an immune system response. The human immune system activation can cause acute, subacute, or chronic inflammation in the patient's tissues (27). The epididymis contains dendritic cells, lymphocytes, basal cells, macrophages, and innate immune molecules that may be activated by any immune system stimulus and cause inflammation within the epididymis and testicle (28). The proposed immune mechanism seems logical in the context of a very short interval between vaccination and the occurrence of complications (21).
The main difference between the mentioned cases is the occurrence of testicular torsion after epididymal orchitis after the MMR vaccination, and no similar case has been reported by reviewing the literature. Previously reported cases had transient post-vaccine orchitis with normal Doppler ultrasound and improved with follow-up. It is essential to know the importance of testicular swelling after MMR vaccination in infants. Such patients should be evaluated and followed up in terms of irreversible consequences.
3.1. Conclusions
The patient should seek an urgent medical consultation in the case of any pain, swelling, or redness of the scrotum due to the even rare possibility of testicular torsion after MMR vaccination. Physicians should pay attention to the fact that testicular swelling after vaccine injection is not just a transient epididymal orchitis but may be a medical emergency. Such patients should be thoroughly evaluated and followed up regarding irreversible consequences.