1. Background
The last strategic plan of the World Health Organization (WHO) emphasized ten global health threats, five of which are directly related to infection prevention and control (1). A hospital IPC team must include trained and expert members to address these threats in healthcare environments and ensure accurate and consistent implementation of best practices (2). Hospital infections are one of the most severe health system problems that cause many costs and effects on the system. About two million hospital infections are reported annually in the US (3), which are also prevalent in Iran and related to considerable morbidity and mortality rates (4).
Based on the prior studies, one-third of these infections would have been controlled with appropriate infection control plans (5), which can prevent considerable costs. Training personnel is one of the primary methods to control hospital infection (6, 7). For example, correct hand hygiene is one of the most essential preventive actions (8), which can improve compliance in personnel and decrease hospital infections considerably (7).
In the past, the primary training method and the lecture method were in the classrooms. Today, multimedia can be used as a practical part (9). Another way is active learning methods, in which participants can work in small groups, and the trainer can approach the educational goal through Techniques like brainstorming, problem-solving, and discussing. A significant difference is observed in the effectiveness of these strategies compared to the traditional methods (10) .Regarding the present study, infection prevention and control training (IPC) focuses more on the nurses. Physicians can play a significant role in dealing with this problem and are among the leading representatives of IPC, but they receive little training in working with this issue (11).
2. Objectives
Therefore, short-term workshops were held to increase the knowledge level and awareness of physicians (medical residents and faculty members) of a big tertiary collegiate hospital in Tehran regarding effective IPC training methods. The training was organized through active learning methods that required participant interaction, multimedia, and classical methods such as short lectures (12).
3. Methods
This cross-sectional study was conducted as health systems research (HSR) with a pre-test and post-test design on 249 doctors of internal and surgical departments (faculty and assistants) in Imam Khomeini Hospital in Tehran, Iran. The inclusion criteria included willingness to participate in research and having more than one year of clinical work experience.
The study included 279 participants (by census method) out of a target group of 409 doctors and a minimum sample size of 215 people. Other doctors refused to participate in the study due to not willing to participate in the workshop or not having enough time. Of the 279 participants, 31 were excluded from the study due to not having completed the questionnaires properly. Finally, the study was conducted on 248 people. The data were collected with a special pre-test and post-test questionnaire designed for this purpose. The questionnaire was composed after the study population was determined and the professors checked for reliability and validity. A total of 30 points were awarded to the questionnaire, which included close- and open-ended questions. The workshops were held in the Imam Khomeini hospital complex in Tehran, Iran. The participants' awareness before the workshop was evaluated by a standardized questionnaire, and then the training was held by the pioneer professors in the IPC field and the hospital infection control unit, using multimedia and short lectures. The participants' awareness was again evaluated using the questionnaire at the end of the workshop.
The questionnaires were designed using the KAP (Knowledge, Attitude, Practice) method. A Questionnaire of 30 questions was appropriate to the educational content of the workshops, including multiple choice answers or short answers completed by the participants both before and after the workshop. The questionnaire had four sectors, including demographic and basic information of the participants, knowledge, attitude, and performance (epidemiological information, disease transmission, infection prevention and control principles, and clinical management). The educational content and references were selected based on the infection control guidelines of the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and the policies communicated by the Ministry of Health and Medical Education. The validity and reliability of questionnaires were assessed both quantitatively and qualitatively. An expert panel including an infectious disease expert, infection control fellowship, microbiologist, epidemiologist, and infection control supervisor with sufficient experience, research, and publications in this field was used to determine the qualitative validity. Cronbach's alpha coefficient was used for reliability.
The working method started with the first step, including the researcher explaining the purpose of the study, and the participants were given a pre-test to measure their performance. Then, training was provided to the participants in two-way communication and group training, as well as a training package in the form of an eight-hour workshop. Content details and headings include surveillance systems, ways of transmission of infections, major hospital infections, microbial resistance, the main components of the infection control program of medical centers, hand hygiene, standard precautions, and precautions based on transmission, personal protective equipment, safe injection, isolation, outbreak management, antibiotic stewardship, environmental hygiene, general disinfection and sterilization of instruments, waste management, care bundles to prevent instrument-related infections (DAIs), occupational exposures, and needle sticks.
The necessary permits were obtained from the Research Ethics Committee of Tehran University of Medical Sciences under 96-03-113-36103 and the relevant officials after the Research project was approved by the university's Research Vice-Chancellor.
The collected data were analyzed using SPSS software version 26 and descriptive statistics and analysis methods. P < 0.05 was considered significant.
4. Results
In the study, 251 residents, 211 people, and 158 faculty members participated in workshops. Of these, 22 residents and eight professors did not complete the questionnaire. Therefore, 189 residents and 60 faculty members finally completed the study.
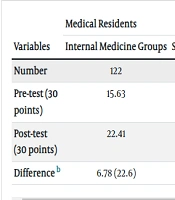
Of the 189 residents, 122 were related to internal medicine groups, and 67 were residents of surgery fields. Among faculty members, 39 were in internal medicine, and 21 were in surgical fields.
The mean mark of the pre-test for internal residents was 15.63 (out of 30) and 13.11 for surgical residents. The post-test mean was 22.41 and 18.09 for internal and surgical residents, respectively. These points were 19.52 (pre-test) and 22.39 (post-test) for internal medicine faculty members and 18.70 (pre-test) and 20.64 (post-test) for surgery faculty members.
Accordingly, a significant increase was observed in all groups (Table 1). The paired sample T-test was used to determine whether the difference was due to chance.
| Variables | Medical Residents | Faculty Members | ||
|---|---|---|---|---|
| Internal Medicine Groups | Surgery Groups | Internal Medicine Groups | Surgery Groups | |
| Number | 122 | 67 | 39 | 21 |
| Pre-test (30 points) | 15.63 | 13.11 | 19.52 | 18.70 |
| Post-test (30 points) | 22.41 | 18.09 | 22.39 | 20.64 |
| Differenceb | 6.78 (22.6) | 4.98 (16.6) | 2.87 (9.57) | 1.94 (6.46) |
a Pre-test Post-test difference was significant in all groups, with a P-value of 0.000.
b Values are expressed as No. (%).
5. Discussion
The present study was conducted for the first time in Iran to investigate the impact of holding infection control training courses for physicians. The results indicated that holding training courses for doctors significantly improves their ability to control infection. Aligned with the present study's results, previous studies also observed that increasing the treatment staff's knowledge to control and follow up on the infection seems necessary (13, 14). Abalkhail A. et al. indicated that the provision of training based on written programs helps improve the knowledge of medical staff about standard infection control precautions and is effective in facilitating the positive attitude and performance of staff (15). Another study also observed that it is vital to provide training and document specific educational programs continuously. There were gaps between the knowledge and performance of health system employees in infection control. This issue further defines the importance of providing planned training on a continuous and periodic basis, as well as continuous monitoring of employees' performance (16).
In this regard, the results of the clinical trial study conducted in 2021 can be referred. The results obtained in this study showed that providing training in modules and face-to-face training has a more significant effect on the knowledge and performance of health system employees. In addition, the three-month follow-up compared to the immediate investigations after the intervention showed a decrease in the knowledge and performance of the treatment staff, so it was suggested that the necessary training should be provided continuously and every six months in the form of in-service training to the staff, especially the nurses (17).
Therefore, another study observed that factors such as older age, longer work experience, and higher educational status were significantly related to the knowledge and practice of infection prevention. In-service training, availability of infection prevention equipment, and adherence to infection prevention guidelines were also associated with infection prevention programs.
A recommendation was made to improve the level of education specialists, provide continuous access to infection control resources and training, as well as provide practical standards, continuous monitoring, and guidance to enhance infection control goals (18).
Despite the emphasis on providing continuous and ongoing training programs, a lack of awareness of infection control and prevention measures has been shown several times after training (19, 20). Therefore, healthcare staff should be aware of and pay special attention to various aspects such as hand hygiene, wearing personal protective equipment (PPE), immunization to prevent communicable and Infectious diseases, understanding the methods of infection transmission, assessing patients for infections, disinfecting medical devices, and proper disposal of hazardous waste.
It is essential for treatment staff to adhere to infection prevention and control (IPC) precautions, methods, and strategies to minimize healthcare-associated infections (HAIs) in healthcare environments (6).
5.1. Conclusions
Based on the results about the need for training physicians in controlling hospital infections and the significant difference in their marks before and after the workshop, it seems necessary for healthcare system authorities and hospital infection control committees to prepare conditions for holding such training workshops.