1. Background
Infections have been documented among the foremost causes of maternal mortality in the course of childbirth (1). In this context, surgical site infections (SSIs) are likely to occur one month after surgery or up to one year due to implant placement in surgical incisions (2). Obesity, diabetes mellitus (DM), corticosteroid use, suppressed immune system, anemia, hypertension, and wound hematomas caused by inadequate hemostasis have been acknowledged as the main risk factors associated with such infections (3).
Contaminated incisions are, in this way, considered as the pathogenesis of uterine infections following Cesarean section (C-section). Bacteria colonized in the cervix and vagina enter the amniotic fluid during delivery, which also invades the weakened uterine tissue after childbirth. Subsequently, cellulitis appears in the parametrial region following infection of the retroperitoneal fibroareolar connective tissue (4).
According to the centers for disease control and prevention (CDC), SSIs have been classified to date into incisional (e.g., superficial or deep) and organic (e.g., anatomical regions) types resulting from surgical wounds within one month following surgery. These wounds can be clean, clean-contaminated, contaminated, and dirty (5). As a whole, SSIs are potential complications linked with surgical procedures. In this regard, the high incidence rate of such postpartum infections has been reported across the world (6). Pregnant women are thus susceptible to infections during childbirth, including SSIs, which have been ranked the fourth most common hospital-acquired infections (HAIs) (7). In this line, fever is the key criterion for diagnosing postpartum uterine infections. Naturally, the degree of fever corresponds to the levels of infection and sepsis. Chills accompanied by fever point to bacteremia or endotoxemia. Patients typically complain about abdominal pain, and then parametric sensitivity is developed during abdominal and bimanual examinations. Leukocytosis may be 15000 - 30000 cells/μL, even though childbirth increases the leukocyte count. Many women further go through foul-smelling discharge with no infections and vice versa. Some other infections, particularly those induced by group A β-hemolytic streptococcus, may also be accompanied by a slight, odorless discharge (8).
As preventable complications, SSIs are heavy burdens incurred on patients regarding morbidity, mortality, and treatment costs. In this respect, over 60% of cases suffering from such infections experience prolonged intensive care units (ICUs) compared to patients with no evidence of infections, which are also more likely to expire compared to individuals without SSIs (9). SSIs are among the significant healthcare burdens, such as increased length of stay (LOS) in hospitals and post-discharge care expenditures (10). Although instrument sterilization methods and infection prevention strategies have advanced considerably, SSIs remain the primary cause of HAIs (11). Although the number of institutions and specialists has multiplied, the incidence rate of such infections after C-section is still high worldwide, particularly in developing nations (12).
2. Objectives
Thus, assessing the predisposing factors for SSIs following C-section is essential to develop more targeted interventions and minimize occurrence and complications, thereby lowering hospital costs and LOS. From this perspective, the present study was conducted to determine the frequency and risk factors of SSIs after C-sections in pregnant women referred to the maternity ward of Ali ibn Abi Talib Hospital in Zahedan, Iran, from 2020 to 2022.
3. Methods
This study was conducted for 18 months, from early September 2020 to February 2022, using a descriptive cross-sectional research design on all women referred to the maternity ward of Ali ibn Abi Talib Hospital undergoing C-section, elective, or emergency surgery. The patients were selected by the census method and tracked for one month after surgery if they met the inclusion criteria.
The inclusion criteria were signifying an informed consent form, cooperating during examinations and follow-up, and the absence of active infections, such as bacteremia, septicemia, or chorioamnionitis. Individuals with a Body Mass Index (BMI) over 40kg/m2, pelvic inflammatory disease (PID), a history of coagulation disorders, cardiovascular disease (CVD), intraoperative hemorrhage, and surgeries for gynecologic cancers were also excluded. The local ethics committee of the Zahedan University of Medical Science approved the study procedure (IR.ZAUMS.REC.1400.343).
3.1. Statistical Analysis
The data were analyzed using SPSS 22 software. Mean (standard deviation) and number (percentage) were used to describe quantitative and qualitative variables. t-tests, chi-square, and logistic regression were used to determine the factors affecting the occurrence or absence of infection.
4. Results
In this study, out of 5,300 elective and emergency C-sections performed at Ali ibn Abi Talib Hospital in Zahedan, 120 cases (2.26%) that resulted in postoperative infections and were subsequently returned to the hospital were investigated.
As shown in Table 1, the mean ± standard deviation (M ± SD) of the patients’ age was 28.68 ± 7.21, with minimum and maximum values of 15 and 44, respectively. The M ± SD of the age of those undergoing elective and emergency C-sections was also 27.18 ± 5.74 and 30.05 ± 8.12, respectively. The Mann-Whitney U test results revealed no significant difference between the study groups (P = 0.56).
| Variables | No. (%) | Age; (Mean ± SD) | Minimum-Maximum |
|---|---|---|---|
| Elective CS (scheduled) | 57 (47.5) | 27.18 ± 5.74 | 15 - 39 |
| Emergebcy CS (labored) | 63 (52.5) | 30.05 ± 8.12 | 15 - 44 |
| P-value = 0.56 | - | - | - |
| Total | 120 | 28.68 ± 7.21 | - |
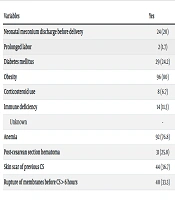
The Incidence and risk factors for surgical site infection following C-section are presented in Table 2. The results showed that the frequencies of cases of obesity and anemia were 80% and 76.7%, respectively. In addition, skin scars from previous cesarean deliveries, pre-labor rupture of the membranes (more than 6 hours), and post-C-section hematoma were detected in 36.7, 33.3, and 25.8% of cases with SSI after cesarean delivery, respectively. In addition, 24.2% of patients with SSI after C-section had DM, and 20% of studied cases had a history of passing meconium. Moreover, a small percentage of patients had a history of immune deficiency (11.3%) and Corticosteroid use (6.7%). Almost all studied subjects were not prolonged under C-section (98.3).
| Variables | Yes | No |
|---|---|---|
| Neonatal meconium discharge before delivery | 24 (20) | 96 (80) |
| Prolonged labor | 2 (1.7) | 118 (98.3) |
| Diabetes mellitus | 29 (24.2) | 91 (75.8) |
| Obesity | 96 (80) | 24 (20) |
| Corticosteroid use | 8 (6.7) | 112 (93.3) |
| Immune deficiency | 14 (11.3) | 106 (85.5) |
| Unknown | - | 4 (3.2) |
| Anemia | 92 (76.8) | 28 (23.3) |
| Post-cesarean section hematoma | 31 (25.8) | 89 (74.2) |
| Skin scar of previous CS | 44 (36.7) | 76 (63.3) |
| Rupture of membranes before CS > 6 hours | 40 (33.3) | 80 (66.7) |
a Values are expressed as No. (%).
5. Discussion
SSIs, as one of the prominent leading causes of surgical mortality, are ever-increasing as a result of the growing number of C-sections performed in private and public hospitals. Accordingly, the frequency and risk factors for SSIs after C-sections in the women referred to the maternity ward of Ali ibn Abi Talib Hospital were investigated from 2020 to 2022. During this time interval, 5300 cases of C-sections were practiced, of whom 120 patients (2.26%) were readmitted owing to postoperative infections. According to the CDC, the incidence rate of SSIs after C-section is, on average, 3.15% (13). In a study in Norway, Eriksen et al. reported this value as 8.2% (14). A meta-analysis concluded that the incidence rate of SSIs in the European Union state members was under 10%. This was also less than 7% in the United States, over 30% in Africa, between 10 and 20% in Asia, and not more than 22% in the Middle East (15). In a comparable study, Dousti and Haghdoost estimated the incidence rate of SSIs after C-section to be about 25% in the women referred to the hospitals in Tabriz, Iran (16). Moradi et al., determining the incidence rate of SSIs after C-sections and the associated factors in Vali-E-Asr Hospital in Fasa, Iran, also stated that the rate of such infections was 5% (17). However, the occurrence of SSIs after C-sections was lower, as compared to previous research. This discrepancy could be attributed to the widespread use of prophylactic antibiotics, the outpatient treatment of superficial infections leading to SSIs, and even some factors such as visiting other medical centers for patients and referring to hospitals in big cities in case of facing the same problems. In addition, observing sterilization principles, continuously reducing operating room pollution, dedicating much attention to the cases of infection, advising patients to maintain hygiene and routine vaginal and abdominal washing, and applying a wide variety of disinfectants could effectively minimize SSIs (15). In line with these recommendations, Mirteimoori and Sakhavar investigated the addition of vaginal wash with betadine to routine abdominal washing on post-C-section infections. In this respect, this practice before elective C-section significantly diminished the incidence rate of fever, endometrium, inflammation, and wound infection (18).
The study findings indicated that almost half of the cases having SSIs (47.5%) had undergone elective C-sections, which was much higher compared to the international standards. As reported by the World Health Organization (WHO), a maximum of 15% of deliveries should be performed by C-section, but the incidence rate of this method in many countries is higher; for example, about 30% in the US and 46% in China (19, 20). Although C-sections account for 10 - 20% of all deliveries in Europe, there has been a significant increase in the number of people in Iran who undergo this surgical procedure as compared to women who deliver vaginally. In today's world, 40 - 60% of pregnancies are terminated by C-section, much higher than statistics published elsewhere (21, 22). The current study findings were consistent with the incidence rates in other parts of Iran. Notably, pregnant women can become more aware of vaginal delivery benefits and C-section harms, as well as maternal-fetal complications, when they take part in childbirth preparation classes accompanied by their husbands. Childbirth fear in this manner is reduced, and as a result, elective C-sections are positively reduced. Moreover, the cases in need of C-sections are better diagnosed if pregnant women receive prenatal care, the necessary examinations, and ultrasound in the last month of their pregnancy, thereby avoiding emergency C-sections, which are recognized as a significant risk factor for postpartum infection (23). Notably, the incidence rate of such infections drops, and the medical staff finds more opportunities to observe health tips.
Furthermore, the current study findings demonstrated that four-fifths of the cases with SSIs after C-section are overweight. Pregnant women, specialists, and medical staff working in the field of public health in Iran, especially those in Zahedan, may want to take note of this warning. Obesity not only predisposes to infections but also aggravates other risk factors for postoperative infections, such as hypertension and DM (24.2% in the present study). In this line, in another study assessed the wound dehiscence rate as one of the consequences of SSIs after C-section. They found a significant relationship between SSIs and incision opening and maternal hypertension and DM. As well, Schneid-Kofmann et al. and Onyekwelu et al. validated the same results in their studies (24, 25). Notably, DM could weaken the immune system, which could then be the leading cause of SSIs after C-section (26). Therefore, much attention should be given to monitoring and controlling weight, blood pressure, and blood sugar in pregnant women before, during, and after C-sections to prevent upcoming risks.
Anemia was found in 76.7% of the cases experiencing SSIs after C-sections in this study. Getaneh et al. (2020), in a review study of 11 articles on SSIs and the related factors after C-section, revealed that anemia increases the risk of postoperative infections in patients by 4.56 times (27). Assawapalanggool et al. also indicated that the amount of hemoglobin under 11g/dL could augment the risk of infections by 2.19 times (28). Therefore, anemia has been documented in previous research as a predisposing factor for SSIs, which agrees with the findings in the present study. Moreover, hemorrhages following C-sections and SSIs are almost twice more than those in natural childbirth. Almost 3% of pregnant women undergoing C-sections need a blood transfusion (29); therefore, this surgical procedure is one of the main factors aggravating anemia. Accordingly, it is recommended to routinely check total blood cell count, reflect on the related indices before and after delivery, and even treat anemia immediately to prevent some complications, such as SSIs after C-section.
Chu et al. (30) and Kehl et al. (31) identified premature rupture of membranes (PROM) as one of the leading causes of SSIs after C-section among 40 patients (33.3%) suffering from SSIs. In 2014, Wilkosz et al. further suggested the history of PROM as one of the risk factors for SSIs after C-section (32). Here, the present study harmonized with the mentioned works.
Additionally, pregnant women were always believed to need C-sections if they underwent one. Nowadays, it is thought that natural childbirth can be performed under the supervision of a gynecologist and a midwife when the previous C-section's cause is not present in this pregnancy (e.g., as opposed to an earlier pregnancy during which the fetus was positioned transversely, this pregnancy has the fetus positioned head-down). The patient is in a well-equipped hospital, and pregnant women should be accordingly informed that natural childbirth is much safer than a major surgery, like a C-section, when there are no contraindications (33). Therefore, educating pregnant women about the complications of C-sections, especially the repeated ones, seems to reduce the number of elective surgical procedures and the incidence rate of SSIs.
This study was limited by the dispersal of the patients in Sistan and Baluchestan province, Iran, and referral to other medical centers and big cities in case of SSIs after C-section, which could hinder follow-up. In this study, only SSIs were investigated, but other infections could also be one reason for the fall in the incidence rate of SSIs compared to previous research outcomes worldwide. However, one of the study's strengths is identifying obesity and anemia rates among pregnant women in this region and Sistan and Baluchestan provinces, emphasizing the need for follow-up, planning, and policymaking to control these two risk factors.
5.1. Conclusions
Although the frequency of SSIs and their complications were generally desirable in the present study, they could cause irreversible damage to maternal-fetal health and even impose very high costs on families and society. For that reason, physicians and midwives are suggested to provide comprehensive explanations regarding natural childbirth benefits and C-section harms before childbirth to encourage pregnant women to have natural delivery when there are no indications for C-section. Moreover, much attention should be devoted to monitoring and controlling BMI, blood sugar, blood pressure, and anemia and treating them to prevent this mysterious, concerning complication.