1. Background
Low back pain is often thought of as idiopathic, although sacroiliac joint (SIJ) dysfunction is a source of low back or buttock pain. Seventy five percent of those with chronic low back pain can be identified as roughly (1, 2). Like any other joint, the sacroiliac can be damaged, degenerated, and inflamed. Its supporting soft tissue can also be damaged. Dysfunction of this joint can be due to pregnancy, trauma, fracture, inflammatory arthroplasty symptoms, increased load on the joint, and degenerative changes after lumbar fusion surgery, which also includes the sacrum (3). The sacroiliac joint mechanics is the largest joint in the body. It has a critical role in mechanical low back pain (4). There is no specific pattern, and sacroiliac joint pain is indistinguishable from other causes of lower back pain (5). When the patients do not respond to standard therapies such as analgesia and inflammation, other treatments should be considered, such as intra- and extra-articular injections or injection of a neurolytic (6). Studies have shown that intra-articular injection of the sacroiliac can relieve long-term pain (7). Fluoroscopy has been used as a reliable technique in many procedures (8). However, this method has limitations, such as exposing the person to radiation and the direct and indirect costs associated with this method. Studies have also suggested that to affect the accuracy and correctness of this method, additional studies must be conducted (9, 10). Alternatively, ultrasound is helpful in many musculoskeletal treatment and rehabilitation processes. This method has advantages such as cost-effectiveness, no need for radiation, and ease of use. However, regarding the application of this method in intra-articular sacroiliac injections, the studies that have been done so far have not been conclusive about its accuracy and selection as the preferred method for performing sacroiliac injections (11). Some studies have shown both methods' effectiveness but concluded that ultrasound requires more experience and skill (12). According to the sonographic landmarks, the needle can easily be inserted in the desired location using the ultrasound technique. Still, more research is needed to be widely and acceptably accepted in the clinic (13). Methods such as a needle guide are required to inject the sacroiliac joint effectively. It should be noted that the C-arm method is currently used for injection into the sacroiliac joint. But this method is an expensive method that can be used in all centers does not exist. The radiation received by the patient should also be considered in the C-arm method (14). Ultrasound has become a helpful tool used in many reintegration and musculoskeletal medicine procedures because it compensates for cost-effectiveness, lack of radiation, readiness of use, and dynamic examination. However, more research is desirable in this area so that it can become a more generally accepted practice.
2. Objectives
In this study, intra-articular injection of the sacroiliac via ultrasound guide was compared with the fluoroscopic method as a more straightforward, more accessible method without radiation damage, which, based on the available evidence, had acceptable accuracy and effectiveness.
3. Methods
The Institutional Review Board of Iran approved this study (IR.GUMS.REC.1399.408). The present study was a pilot study with at least 76 patients in two groups. Patients with chronic low back pain were referred to the pain clinic. The study was conducted in the pain clinics affiliated with the Guilan University of Medical Sciences, including Razi, Shafa, and Velayat Hospitals. The research was carried out in 2020. This study determined the sample size as a pilot, with a minimum of 30 patients assigned to each group. The ultrasound device used in this research was the General Electric (GE) DEC 9900 C-arm. This device and a 2.5 to 8 MHz ultrasound probe guided the sacroiliac joint intra-articular injection. The ultrasound probe was curved with a 2.5 to 8 MHz frequency range.
3.1. Inclusion Criteria
Patients over 18 years old with persistent sacroiliac joint pain. At least four positive tests out of 7 in clinical examinations. Average pain of at least 3 out of 10 (NRS). Pain lasting for at least 3 months and no response to at least one or two conservative treatments (oral medications, anti-inflammatories, analgesics, muscle relaxants, physical therapy).
3.2. Exclusion Criteria
Lower back pain without differentiation between sacroiliac joint and L5/S1 discogenic pain. Sensitivity to contrast dye or contraindications to fluoroscopy. Active lesions in structures related to the sacroiliac joint (e.g., lumbar spine, hip pathologies). Active inflammatory diseases, untreated coagulopathies, previous intra-articular injection, infection, bleeding, trauma to the target site.
The preliminary diagnosis was based on a history of pain lasting 3 months or longer in the buttock, groin, or thigh, regardless of associated lower extremity symptoms. Positive physical examination included tenderness over the area just below the posterior superior iliac spine, the Patrick test, or Gaenslen’s test (Figure 1) (15). The patient is placed in the prone position (lying face down). A pillow is placed under the abdomen to flex the lumbar region slightly and optimize the spine's positioning.
The drug injected was Bupivacaine 0.2% (manufacturer: L Molteni; Italy) and methylprednisolone 40 mg Iranian (manufacturer: Caspian Tamin Co, made in Iran), which was done with a Sharp Curve 22 needle. The type of ultrasound device, 2.5 to 8-MHz ultrasound probe and ultrasound machine, and fluoroscopic images were obtained through General Electric DEC 9900 C-arm. Guided injections are used per the technique previously described in the literature (Figure 1) (16). Patients in both groups in terms of passive and elective pain intensity based on Numerical Rating Scale (NRS) pain severity in NRS is rated on an 11-point numeric rating scale (from 0 = ''no symptom'' to 10 = ''worst symptom imaginable'') (17) [before (time zero), 15 minutes after and 24 hours after the procedure), the length of the procedure was compared. Also, when the patient was transferred to recovery, he was evaluated for negative tests before injection.
3.3. Statistical Analysis
Data analysis was performed using SPSS version 21. Descriptive statistics were represented as percentage, mean, and standard division. Mann-Whitney, Kolmogorov-Smirnov, and t-tests were used for parametric and non-parametric analysis. The significance level of tests was ≤ 0.005 in this study.
4. Results
Seventy-six patients were screened for this study intervention, including 30 in the ultrasound-guided and fluoroscopy-guided groups. There was no difference between the two groups in terms of basic characteristics [Gender, age and Body Mass Index (BMI)] No statistically significant difference between the mean age, weight, height, and BMI of patients in the two groups using ultrasound guide and fluoroscopic guide in the intra-articular injection of the sacroiliac joint (P < 0.005) (Table 1).
| Variables | Fluoroscopic | Sonography | P-Value |
|---|---|---|---|
| Sex | 0.263 | ||
| Man | 14 | 16 | |
| Female | 24 | 22 | |
| Age (y) | 47.55 ± 15.9 | 43.07 ± 11.53 | 0.173 |
| Weight (kg) | 75.44 ± 11.29 | 75.63 ± 13.28 | 0.24 |
| Height (cm) | 165.32 ± 10.23 | 168.15 ± 10.03 | 0.948 |
| BMI (kg/m2) | 27.56 ± 2.97 | 26.6 ± 2.93 | 0.176 |
| 19 < BMI ≤ 25 | 9 | 12 | 0.471 |
| 25 < BMI < 30 | 19 | 21 | |
| > 30 | 8 | 5 |
Demographic and Clinical Features of Study Patients a
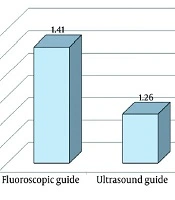
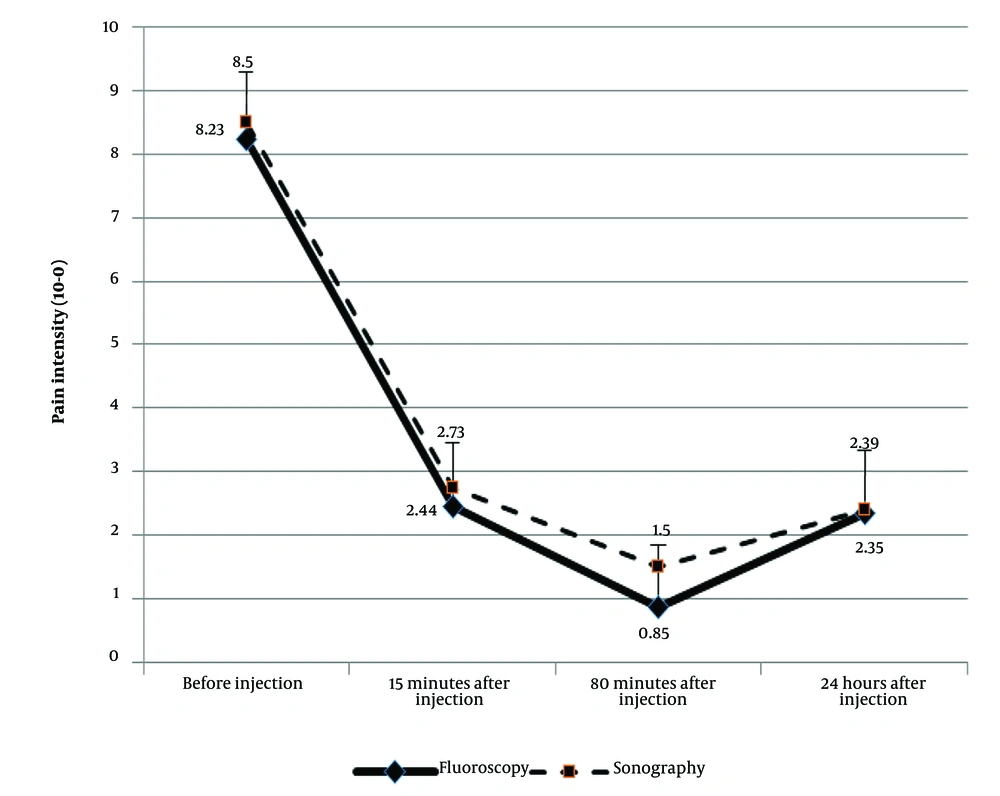
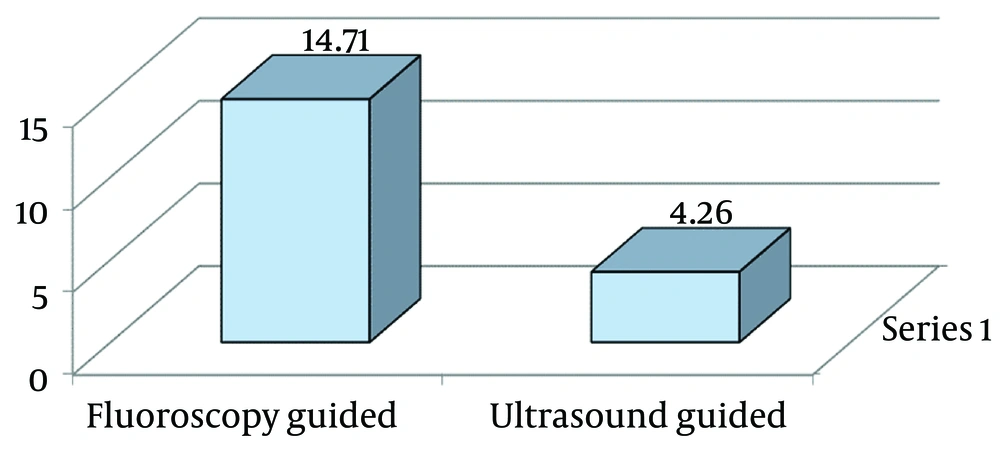
Gender can often influence the severity or response to certain interventions, as biological differences between males and females may affect pain perception, anatomy, or response to treatment. However, in this study, the lack of significant difference between the groups based on gender was noted, suggesting it may not have had a major impact on the results. Age is another important variable in clinical studies because it can affect the course of diseases, the effectiveness of treatment, and the body's healing capacity. While the mean age was compared in both groups, no statistically significant difference was observed. There is no statistically significant difference between patients' mean age, weight, height, and BMI in the two groups using the ultrasound and fluoroscopic guide. There is a statistically significant difference between the mean pain intensity values based on the NRS Index during the study periods in the two groups of patients (P < 0.001). There is a statistically significant difference between the mean pain intensity values during the studied periods in patients of the two groups (P < 0.001). However, there was no statistically significant difference between the course of changes in the mean pain intensity values during the studied periods in the two groups of patients (P = 0.389). There was no statistically significant difference between the mean pain intensity before injection, 15 minutes after injection, and 24 hours after injection between the two groups of patients using a fluoroscopic guide and ultrasound guide in intra-sacroiliac injection (P < 0.005). Still, 60 minutes after injection, it is seen between the two groups of patients using a fluoroscopic guide and sonographic guide in intra-sacroiliac joint injection (P = 0.01) (Figure 2). No statistically significant difference was seen between changes in the mean pain intensity values during the studied periods in the two groups of male patients (P = 0.484). There was no statistically significant difference between the course of changes in the mean pain intensity values during the studied periods in the two groups of female patients (P = 0.687). There is a statistically significant difference between the mean time of the procedure in the two groups (P < 0.001) (Figure 3). There was no statistically significant difference between the mean number of punctures (frequency of injections) (P < 0.365) (Figure 4).
5. Discussion
The sacroiliac joint is an essential biomechanical structure with high nerve conduction and complex movements and can be a source of pain. In recent years, sacroiliac joint involvement has been recognized as one of the leading causes of low back pain (18, 19). One of the available treatments to reduce pain in this joint is the injection of local anesthetic into the joint; also, the method of injection and the accuracy of the operation are essential issues (20). Due to incorrect and unacceptable injection into the sacroiliac joint, fluoroscopy or ultrasound guide is recommended. Our findings showed that at 60 minutes, the pain intensity was significantly lower in the fluoroscopic group than in the ultrasound group. But this superiority was not seen after 24 hours. Therefore, it cannot be one of the advantages of the fluoroscopic method. The average number of punctures could indicate the performer's mastery, which was not significantly different between the two groups. The significant result obtained in this study was a significant difference between the mean time of the procedure (intra-sacroiliac joint injection) in the two groups of patients using the ultrasound guide compared to fluoroscopy. Various studies have reported results that sometimes align with this research and disagree (18, 20). showed that both methods were effective and uncomplicated. In their study, there was no difference in superiority between the two methods (21). According to the findings of our study, performing a diagnostic block of a sacroiliac joint under ultrasound guidance in patients with a high probability of pain due to this joint has a relatively high accuracy and has no specific side effects. Therefore, due to this issue and the use of ultrasound, no restrictions or side effects were observed in other imaging methods. Ultrasound-guided sacroiliac joint diagnostic block can be a valuable alternative to this block guided by other imaging techniques such as fluoroscopy and CT-scan knew.
As comparisons of various studies show, the results are not in the same direction. Several factors can justify differences in study results. Heterogeneous method, selection of local anesthetics, corticosteroids, and other drugs, differences in studied populations, different evaluation criteria, and different follow-up times vary from one day to several months, in addition to the above, the NRS-based report of pain intensity, which is the patient's declaration of pain intensity, is entirely dependent on patients' interpretation and definition of pain. These factors affect the results of the study. The influence of race, different populations, and the physician's skill, accuracy, and experience in operating are also essential factors.
5.1. Conclusions
The results of our study showed differences in accuracy, effectiveness, or overall patient satisfaction between the two techniques. Considering the advantages that have been reported about the ultrasound method, such as ease, cost-effectiveness, no risk of the patient being exposed to radiation, the possibility of performing it next to the patient's bed, and based on the results of this study, performing ultrasound has been introduced as the superior method. However, to generalize it, more general studies are needed.