1. Background
In 1983, Marshall and Warren discovered the gram-negative bacteria (Helicobacter pylori), which infects the human gastric mucosa (1, 2). Helicobacter pylori is the first bacteria designated as a definite carcinogen by the World Health Organization's (WHO) International Agency for Research on Cancer (IARC) at 1994 (3). Over 50% of people worldwide may carry the spiral-shaped bacterium H. pylori, which develops in the digestive tract (4). Helicobacter pylori could be responsible for serious stomach disorders such as peptic ulcers and gastric cancer.
The incidence among children globally is recognized, and it varies by country. The prevalence of H. pylori infection is high in under developed countries may reach 70%, even in children while in developed countries, it is typically less than 40% of the total population, and much lower in children (1, 5). Socioeconomic status and improvement of hygiene are two factors that have contributed to reduce of the prevalence of H. pylori worldwide (6). Infants and young children are susceptible to developing H. pylori infections, which often last a lifetime if untreated (7, 8). Since few studies have been done and the majority of infected infants do not exhibit any symptoms, it is unknown how prevalent the H. pylori infection is in infants compared to adults (9).
Many paediatric epidemiologic research revealed that H. pylori infection started in infancy and with later peak incidence between the ages of 5 - 7 years (8).
The National Center for Health Statistics of the Centers for Disease Control and Prevention (CDC) has carried out extensive surveys and revealed family history of H. pylori infection or previous treatment of H. pylori infection in the family is a risk factor for infection, while parental education level, family history of gastrointestinal manifestations or stomach cancer is not associated with increased risk of infection (10).
2. Objectives
The aim of this study was to determine the prevalence of H. pylori infection and associated factors during infancy.
3. Methods
This study is a cross-sectional study that was conducted on 110 infants (6 - 12 months of age) referred to the Rapareen teaching hospital clinic and Kurdistan health centre in Erbil city from 1st Feb. to 1st Aug. 2023.
The samples were included in the study with the convenience sampling method after explaining the goals and process of the study to their parents or legal guardians and obtaining their informed consent.
Demographic information and certain clinical data were obtained, crowding indexes are generally quantitative measures based on American Crowding Index/people per room: It is defined as the number of people living in a dwelling divided by the number of rooms, overcrowding occurs if there are more than 1.5 persons per room (11).
Hygienic measures like hand washing; improper means poor water sources or food handling, washing and sterilization.
3.1. Inclusion Criteria
- Healthy infants between 6 months and 1 year.
- Absence of gastrointestinal symptoms or underlying chronic illness.
3.2. Exclusion Criteria
- Dissatisfaction to continue studying.
- Recent antibiotic and proton pump inhibitors (PPIs) treatment.
- Underlying serious illness.
Informed and written consent were obtained from parents or caregivers of infants and ensure that participants are properly informed about:
- Study purpose: Participants being informed why this research conducted.
- Testing procedures: Explanation of how the stool test will be conducted, and any potential risks involved (such as discomfort, risk of false positives/negatives, etc.).
- Confidentiality: Assurance that all information will remain confidential.
- Voluntary participation: Emphasizing that participation is voluntary.
- Results: Whether participants will be informed of their individual test results and if they will have access to any follow-up care or treatment based on the results.
SPSS version 23 statistical software was used for data analysis. Also, descriptive statistical tests were used to report demographic variables, chi-square test to compare qualitative variables between groups, Student's t-test to compare averages, and logistic regression to examine variables affecting the incidence rate. A multivariable logistic regression model is used to simultaneously evaluate the influence of multiple predictor variables on a binary outcome, such as whether a stool test for H. pylori is positive or negative. Predictor variables (independent variables) are the factors could influence whether a stool test is positive or negative for H. pylori. Goodness-of-Fit have been used and it is the multivariable logistic regression model allows you to understand the simultaneous effects of multiple predictors on the odds of testing positive for H. pylori. It also helps to control for potential confounders, such as age or gender, when assessing the relationship between other variables and the outcome.
Helicobacter pylori status was determined for infants and their mothers by H. pylori antigen linear cassette was used to diagnose Helicobacter infection. Helicobacter pylori Ag linear cassette is a flow chromatographic immunoassay. When an adequate volume of extracted fecal specimen is dispensed into the sample well of the test cassette, the specimen migrates by capillary action across the cassette. Helicobacter pylori antigen if present in the specimen will bind to the anti-H. pylori conjugates. The immunocomplex is then forming a burgundy colored T band, indicating a H.P positive test result. Absence of the T band suggests a negative result.
4. Results
The mean age of the examined infants was 8.99 ± (2.074) and slightly males were more dominant (56.4%) with mean age of studied group is 8.856 ± (1.157) as shown in Table 1.
| Variables | Mean ± SD or No. (%) |
|---|---|
| Age (mo) | 8.99 ± 2.074 |
| Maternal age | 29.463 ± 5.809 |
| Paternal age | 32.745 ± 6.503 |
| Weight (kg) | 8.856 ± 1.157 |
| Length (cm) | 71.099 ± 10.128 |
| Gender | |
| Male | 62 (56.4) |
| Female | 48 (43.6) |
| Gestational age | |
| Term | 97 (88.2) |
| Preterm | 13 (11.8) |
| Feeding | |
| Breast | 47 (42.7) |
| Bottle | 43 (39.1) |
| Mixed | 20 (18.2) |
| Exclusive breast feeding for 6 months | |
| Yes | 26 (55.3) |
| No | 21 (44.6) |
| Family hx. of Helicobacter pylori infection | |
| Yes | 24 (21.8) |
| No | 86 (78.2) |
| Socioeconomic state | |
| Upper | 27 (24.5) |
| Middle | 48 (43.6 ) |
| Lower | 35 (31.8) |
| Mean size of the household (Crowding Index) | |
| 1 (< 1) | 8 (7.4) |
| 2 (1 - 1.49) | 48 (43.6) |
| 3 (> 1.5) | 54 (49 ) |
| Hygiene measures | |
| Proper | 92 (83.4) |
| Improper | 18 (14.6) |
The type of feeding in infants showed that 47 (42.7%) infants were breast feeding, 43 (39%) infants were bottle fed, and 20 (18.3%) infants were breast feeding and bottle. Twenty six (55.3%) of infants were exclusive breastfed for at least 6 months. Also majority of babies were of families of different socioeconomic status, Crowding Index of 2 or more and proper hygienic measures (Table 1).
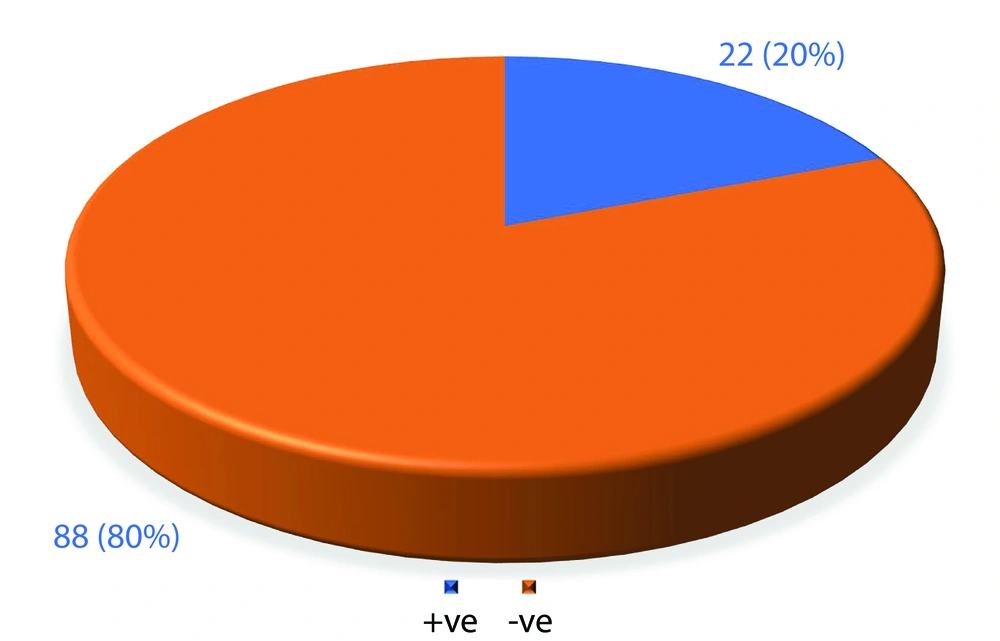
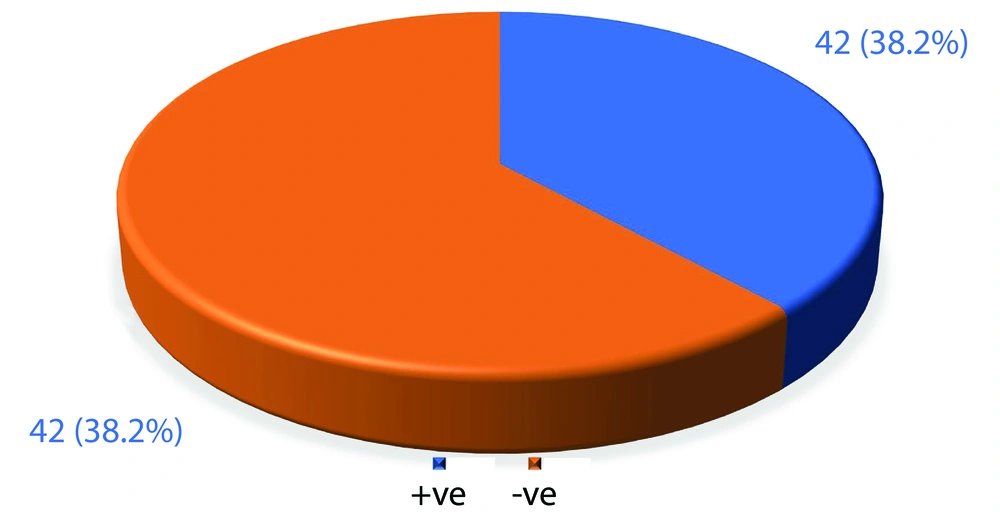
In this study, the prevalence of Helicobacter infection among infants and their mothers were shown is 22 (20%) and 42 (38.2%) cases respectfully (Figures 1 and 2).
In Table 2, significant associations were evident between infants with H. pylori infection with gestational age, less exclusive breast-feeding duration, parental H. pylori infection, improper hygiene and high Crowding Index.
| Variables | Infants | P-Value | |
|---|---|---|---|
| Helicobacter pylori (+) | Helicobacter pylori (-) | ||
| Gestational age | 0.01 | ||
| Term | 16 | 81 | |
| Preterm | 6 | 7 | |
| Gender | 0.211 | ||
| Male | 15 | 47 | |
| Female | 7 | 41 | |
| Type of feeding | 0.4 | ||
| Breast | 10 | 37 | |
| Bottle | 8 | 35 | |
| Mixed | 4 | 16 | |
| Exclusive breast feeding for 6 months | 0.01 | ||
| Yes | 2 | 24 | |
| No | 8 | 13 | |
| Family Hx of Helicobacter pylori infection | 0.001 | ||
| Yes | 10 | 14 | |
| No | 12 | 74 | |
| Socioeconomic state | 0.01 | ||
| Upper | 2 | 25 | |
| Middle | 8 | 40 | |
| Lower | 12 | 23 | |
| Household (Crowding Index) | 0.001 | ||
| 1 (< 1) | 1 | 7 | |
| 2 (1 - 1.49) | 3 | 45 | |
| 3 (> 1.5) | 18 | 36 | |
| Hygiene measures | 0.001 | ||
| Proper | 17 | 75 | |
| Improper | 5 | 13 | |
| Mother Helicobacter pylori | 0.001 | ||
| Helicobacter pylori (+) | 14 | 28 | |
| Helicobacter pylori (-) | 8 | 60 | |
| Maternal age | 30.142 ± 5.706 | 9.044 ± 5.875 | 0.33 |
| Paternal age | 33.238 ± 6.176 | 32.441 ± 6.723 | 0.52 |
Risk factors like high Crowding Index families and maternal H. pylori infection significantly increase rate of infection among their infants while term delivery, exclusive breast feeding for at least 6 months and older maternal age can reduce it as displayed in Table 3.
| Variables | OR | 95% CI | P-Value |
|---|---|---|---|
| Gestational age | |||
| Term | 0.6 | 1.03 - 1.965 | 0.04 |
| Preterm | 1 | ||
| Type of feeding | |||
| Breast | 0.2 | 0.03 - 2.3 | 0.3 |
| Bottle | 0.4 | 0.07 - 2.41 | 0.4 |
| Mixed | 1 | ||
| Duration of breast feeding for 6 months | |||
| Yes | 0.3 | 0.1 - 0.6 | 0.02 |
| No | 1 | ||
| Family Hx of Helicobacter pylori infection | |||
| Yes | 0. 6 | 0.12 - 3.13 | 0.5 |
| No | 1 | ||
| Maternal age | 0.76 | 0.63 - 0.99 | 0.04 |
| Paternal age | 1.21 | 1.09 - 1.49 | 0.07 |
| Socioeconomic state | |||
| Upper | 3.03 | 0.51 - 14.84 | 0.2 |
| Middle | 0.98 | 0.27 - 3.5 | 0.9 |
| Lower | 1 | ||
| Household (Crowding Index) | |||
| > 1.5 | 2.1 | 1.08 - 1.28 | 0.003 |
| 1 - 1.49 | 1.7 | 1.03 - 1.66 | 0.07 |
| < 1 | 1 | ||
| Hygiene measures | |||
| Proper | 4.7 | 1.11 - 20.02 | 0.08 |
| Improper | 1 | ||
| Mother Helicobacter pylori | |||
| +ve | 1.16 | 1.01 - 1.24 | 0.001 |
| -ve | 1 | ||
a 1 means the reference group in multivariable logistic regression and the basis for comparing and investigating the effects of the investigated variable on the development of the disease.
5. Discussion
In this study, the prevalence of H. pylori infection among infants and their mothers were 20% and 38.2% respectfully. Many studies conducted in Iraq to know the frequency of infected patients and were mainly on adults with varying prevalence ranging from 30% to 70% in the last 5 years (12-15) and these diverse results explained mainly by different methods used for identification of the bacteria, also factors like sample size, residency and symptomatic patients can affect results. In Erbil city, a report of confirmed 2320 cases aged between 10 to 60 years were recorded annually from 2019, 2021 and 2022; displayed prevalence of 50.14% ,69.87% and 40.98% respectfully (16)
In the study of Merino et al. (17) with the aim of investigating the dynamics of Helicobacter infection in the first six months of infancy, the results showed that the prevalence of Helicobacter infection among infants is 23%, which is consistent with the results of this study. In a cohort study in Bangladesh, the prevalence of Helicobacter infection in the first year of life was found to be 28.6% (18) while Nizami et al. (19) surprisingly revealed higher frequency exceeding 50% as method of diagnosing the disease was different from the present study.
By examining risk factors, it was shown that the prevalence of H. pylori varies according to sex, gestational age, infant feeding method, positive H. pylori family history, maternal age, socioeconomic status, Crowding Index, hygiene measures and mother H. pylori infection.
The breast milk has a major protective effect against illnesses in infancy and childhood because of containing a lot of bioactive compounds which enhance immunity and protection against many infectious agents (20), so nutrition has influence on acquisition of H. pylori infection. Thomas et al. found a big relation between the age of acquiring the infection and the amount of anti-H. pylori IgA in breast milk (21), as conclusion they found that IgA in breast milk may have a role in delaying getting of H. pylori infection.
A study of Tabatabaei at al. (22) have reported that breastfed children were less affected with H. pylori than bottle fed children. Another study conducted in Germany (23) showed that breastfeeding is not a protective factor against H. pylori while in Japan (24) and others (25) supporting the results of this study that exclusive breastfeeding decrease risk of acquiring the infection but still there no strong evidence to be considered as a protective factor against H. pylori and could have transient protective effect among breastfed infants that reduced later during childhood as demonstrated by many researchers (25).
It seems that the risk of developing Helicobacter infection in infants who have one or more of their family members had a history of Helicobacter infection is much higher. In a study conducted by A Palanduz et al. (16) showed that 9% of children had a positive family history of H. pylori, even higher in this study reaching up to 24%.Lack of access to drinking water and poor sanitation were proven risks for conducting H. pylori infection in many studies (26, 27) as demonstrated in our results.
According to Galal et al. and Mehesin et al. revealed that the higher the Crowding Index, the higher the risk of Helicobacter infection for children, and the risk of infection with a congestion index higher than 3 is higher (28, 29).
In this study, it was shown that 63% of the infant who were positive for H. pylori, their mothers were also positive for Helicobacter infection, which in agreement with the study of Osaki et al. in Japan (30) and other studies (31) Also, in a study conducted by Spotts et al. in Ethiopia, none of the demographic variables had an effective role in getting H. pylori infection (32) and only the history of maternal infection had a direct effect on Helicobacter infection in children, nearly similar to our results.
5.1. Limitations of the Study
A larger sample size would increase the robustness of the findings. The convenience sampling method may introduce selection bias, as the participants might not be representative of the entire infant population in Erbil city. Random sampling would be a more rigorous approach, also recommend specific areas for future research, such as longitudinal studies to assess the long-term impact of infant H. pylori infection or interventional studies.
5.2. Conclusions
Helicobacter infection is not uncommon during infancy, exclusive breast feeding decrease the risk of H. pylori infection in infancy, while other variables such as gestational age, overcrowding and mother’s H. pylori positivity are known as predictors of H. pylori infection.