1. Introduction
Cerebral vein thrombosis (CVT) is a rare but potentially life-threatening condition characterized by the formation of blood clots within the cerebral venous system. While various predisposing factors have been identified, such as prothrombotic disorders, hormonal contraceptives, and pregnancy (1), the occurrence of CVT following spinal cord detethering surgery is exceptionally rare (2). Spinal cord detethering procedures are typically performed to relieve tension on the spinal cord caused by adhesions or abnormal tissue attachments to prevent neurological deficits or complications (2). However, the association between spinal cord detethering surgery and subsequent CVT remains poorly understood, and only a few cases have been reported in the literature to date (3). On one hand, the occurrence of CVT following spinal surgeries is generally rare and has only been reported in a few case reports. On the other hand, tethered cord syndrome has an overall prevalence of 0.25 per 1000 live births, which also classifies it as a rare condition. The simultaneous occurrence of these two rare events highlights the significance of reporting this case.
In this article, we present the case of a 26-year-old woman who developed CVT shortly after undergoing spinal cord detethering surgery for tethered spinal cord syndrome. We discuss the patient's diagnosis, treatment, and outcome in detail, highlighting the difficulties in managing this rare and complicated clinical scenario. Thrombosis of cerebral veins is one of the complications of central nervous system surgeries, but this complication has been reported very rarely after tethered cord release surgery. The headache caused by thrombosis in these patients may be confused with that caused by intracranial hypotension. By sharing this case, we hope to add to the growing literature on the relationship between tethered cord release surgery and CVT, raising awareness and promoting early recognition and management of this uncommon but significant complication.
2. Case Presentation
A 26-year-old female patient underwent an MRI of her brain and spine due to lower limb weakness and urinary frequency. The MRI revealed a low-lying central cord extending towards S1 and a 29 × 10 mm lipoma with fat signal intensity at the S1 level connected to the distal part of the cord, indicative of a caudal-type lipoma combined tethered cord. No brain lesions were found. The patient underwent a tethered cord release surgery without any complications and was discharged three days later. However, five days after the surgery, the patient began experiencing a headache that improved when lying down but worsened when sitting. The headache partially responded to outpatient treatment but did not entirely disappear. After 20 days, the patient was admitted to our center with a severe headache that did not respond to painkillers. Upon admission, the neurological examination was normal, and the margin of the optic disc was sharp.
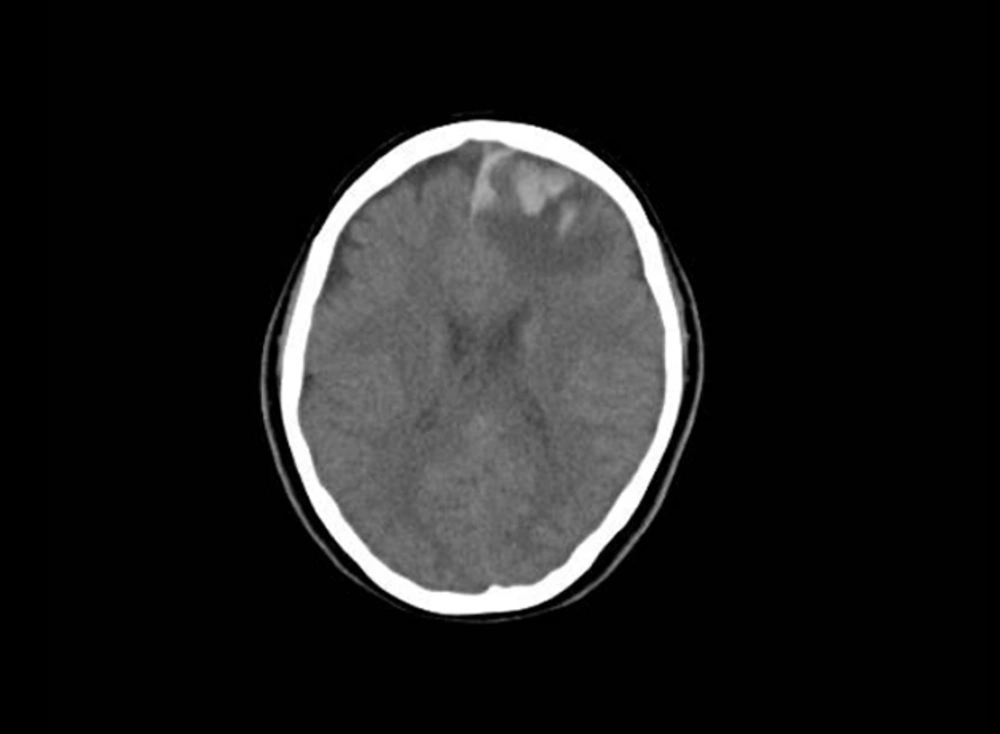
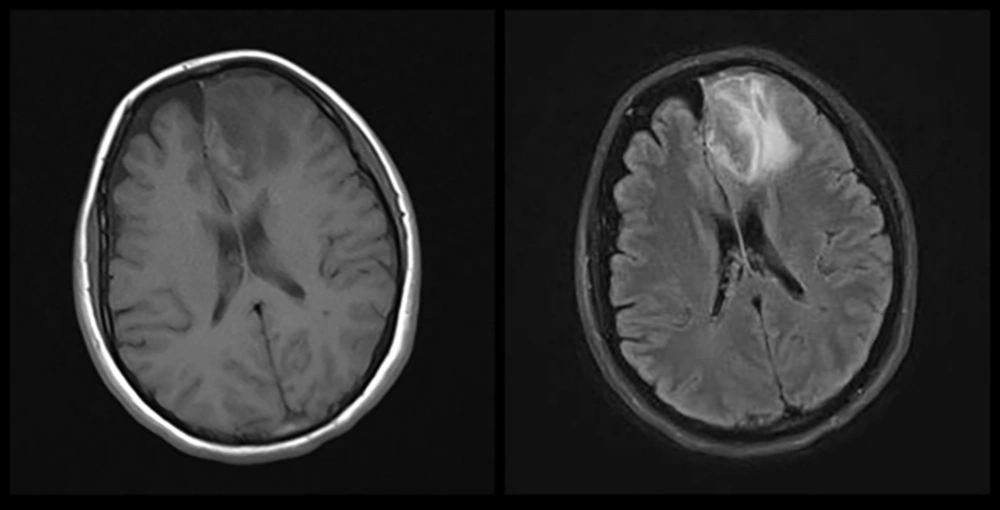
At the beginning of the patient's hospitalization, a brain CT scan was performed that showed no abnormal findings, but one day after admission, the patient had two episodes of generalized tonic-clonic seizures, each lasting about one minute, so a control brain CT was conducted that revealed evidence of hemorrhagic infarction in the left frontal lobe (Figure 1). The patient underwent a Brain MRI ± Gad and brain MRV ± GAD due to suspected hemorrhagic infarction caused by CVT. In the performed imaging, the patient's MRI showed an abnormal signal area with high intensity in T2 and intermediate to low intensity in T1. There was a restriction in some areas in the left frontal lobe, which showed no enhancement after the contrast agent injection (Figure 2). The imaging showed no normal opacification in the superior sagittal sinus and the left Trolard vein (Figure 3). These findings indicated a hemorrhagic infarct caused by thrombosis. The patient was treated with an intravenous heparin infusion to keep the Partial thromboplastin time (PTT) between 50 to 70.
Additionally, the patient was given Levetiracetam 500 every 12 hours and a combination pain reliever consisting of acetaminophen 500 mg, ibuprofen 200 mg, and caffeine 40 mg every 8 hours. The patient's headache eased after two days of treatment, and there were no recurring seizures. Three days after starting heparin, the patient began taking warfarin 5 mg daily. However, three days after taking 5 mg of warfarin, the patient's International Normalized Ratio (INR) was 4.6. Due to this, the patient's heparin was stopped, and warfarin was put on hold. Despite warfarin being on hold, the patient's INR was greater than 3 for the next four days. On the fifth day, the patient's INR was 2.2, and the patient was given warfarin at a dose of 1.25 mg daily. In the following days, the patient's INR was maintained between the range of 2 - 3 while using 1.25 mg of warfarin. The patient did not experience any new neurological symptoms or seizures during her hospital stay. The control CT scans conducted on the 9th and 15th day of the hospitalization indicated no expansion of the brain lesion. After 17 days of hospitalization, the patient was discharged with a complete resolution of her headache, an INR of 2.28, and a prescription for 1.25 mg of warfarin to be taken daily, and the INR range was maintained within 2 to 3.
3. Discussion
Cerebral vein thrombosis is a rare but potentially life-threatening condition that can occur due to various underlying factors (1, 4, 5). In this case, a 26-year-old woman presented with CVT following cord release surgery that resulted in intracranial hypotension. The development of CVT in the context of postoperative intracranial hypotension underscores the importance of considering this complication in patients undergoing neurosurgery, particularly those involving the spinal cord.
Until now, limited studies have discussed the relationship between Intracranial hypotension and the occurrence of cerebral vein clots (4, 6). The cause of this problem is the decrease in cerebral blood flow, which causes blood stasis in the venous system, which leads to thrombosis in the cerebral veins.
Tethered cord release surgery can disrupt the normal anatomy of the spine, potentially causing CSF leakage and consequently reducing CSF pressure. In this patient, it was discussed the importance of monitoring patients who undergo spinal surgeries as part of post-operative care for symptoms of reduced CSF pressure, such as headache and nausea.
The treatment of CVT with anticoagulant drugs aims to reduce the clot's spread and its complications (1, 4). In this case, the timely initiation of anticoagulant medications led to the disappearance of the patient's symptoms and her complete recovery. The decision to prescribe anticoagulants should be made carefully, and the patient's bleeding risk should be considered. Also, it is necessary to closely monitor laboratory factors to check the therapeutic effectiveness of prescribed anticoagulants.
The favorable outcome in this case underscores the importance of early recognition and intervention in patients with CVT secondary to intracranial hypotension. Furthermore, it highlights the potential utility of anticoagulant therapy in this context, although further studies are warranted to elucidate optimal treatment strategies in this patient population. Additionally, long-term follow-up is necessary to assess for potential recurrence of thrombotic events and monitor for anticoagulant therapy complications.
In conclusion, headaches in patients who have undergone neurosurgery and particularly spine surgery should be taken seriously, considering that they have the possibility of cerebrospinal fluid leakage and can indicate a serious vascular accident; if this lesion is diagnosed and treated on time, it’s dangerous and severe complications can be prevented.