1. Background
Sleep is one of the most important aspects of life and a basic need for everyone. Dissatisfaction with sleep conditions is one of the most common reasons for visiting physicians. According to the statistics, complaints of poor sleep quality based on self-reports from people in Western countries were 10% - 48% (1). Lack of treating sleep problems can lead to physical and psychological illnesses such as gastrointestinal ulcers, obesity, depression, anxiety, etc. (2). It should be noted that the worst effects of sleeplessness show themselves in the workplace and reduce the productivity and even the excessive absenteeism (3). Nurses are among those who face sleep problems more than others due to their shift work (4). Obviously, reduced quality of sleep in this group will reduce the quality of service they provide to patients and, consequently, endanger the community health in the long run (5). Evidence suggests that reduced quality of sleep of nurses decreases the quality of care for patients, and also decreases their quality of life and life span (6). The results of a study by Dong et al. in 2017 in China showed that 63.9% of nurses had a PSQI of over 5, which indicated poor sleep quality in this group of hospital staff (1). A common treatment for improving sleep quality is the use of benzodiazepines. Their excessive consumption, however, leads to complications such as forgetfulness, headache, dizziness, and dependence (7, 8). Complementary therapies such as aromatherapy, acupuncture, acupressure, and music therapy have been widely used in recent years (9). Chang et al. investigated the effect of aromatherapy as a complementary therapy on the sleep quality of nurses and found that nurses’ PSQI significantly increased after the intervention in the treatment group (10). Acupuncture is considered as a common complementary therapy in in Asian and European countries (11). According to the theory of traditional chinese medicine (TCM), the simultaneous stimulation of SP6, HT7, and LI4 points improves sleep quality (12, 13). Lee and Wilson stated that the physiological effects of acupuncture are conveyed through the stimulation of the mentioned points that stimulate the production pathway of gamma-Aminobutyric acid (GABA) and consequently this neurotransmitter suppresses the excessive activity of the central nervous system; this process can be effective in increasing the duration and quality of sleep (13-15). Due to invasiveness and insertion of needles, traditional acupuncture can lead to complications such as subcutaneous hematomas and pneumothorax (16, 17). Transcutaneous electrical acupoint stimulation (TEAS) has been used as a safe and low-risk method since 1970 (18, 19). The importance of nursing in medical care is indispensable and the nurses have to be screened continuously by monitoring systems for quality of sleep, and treated effectively in case of any problems. Studies on the treatment of sleep problems in nurses in Iran are scanty. The aim of this study was to evaluate the effect of TEAS on nurses’ sleep quality in Kermanshah, Iran.
2. Methods
2.1. Samples
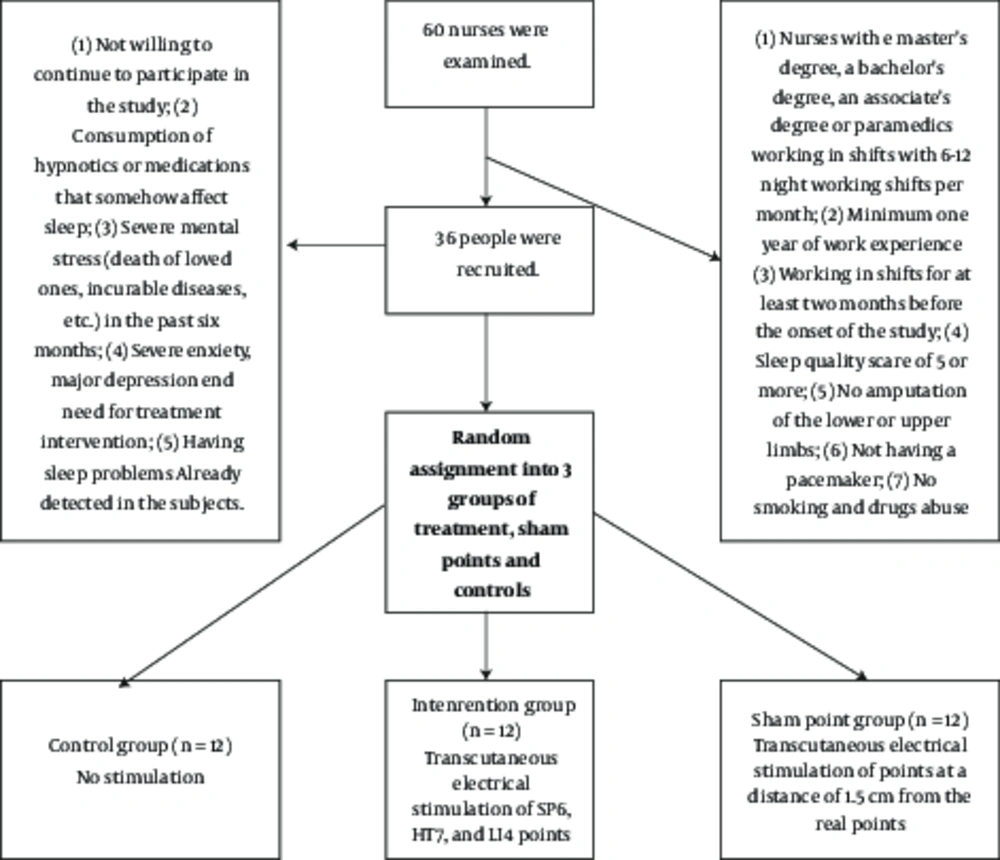
The research population included shift working nurses in Kermanshah hospitals. After screening by PSQI, nurses with sleep quality problems were randomly divided into three groups: real points, sham points and control.
The study population consisted of all shift working nurses working in teaching hospitals in Kermanshah, Iran. The sampling was done by convenience sampling. The research units were randomly (by rolling dice) assigned to three groups of real points, sham points, and control. The sample size was calculated 11 subjects for each group (two intervention groups and one control group). Considering 10% loss of samples, 12 subjects were selected for each group. TEAS was performed by an acupuncturist.
2.2. Data Collection and Intervention Tools
Data were collected by demographic characteristics form and PSQI from nurses with shift works with sleep disorders in 2015. The intervention was performed by an acupuncture device (Acuhealth Pro 900; Serial No. C2375; Made in Italy) which can accurately locate acupuncture points and is actually equipped with the AcuPoint Finder. After finding the energy channel and the intended point, the device produces electrical impulses of 2.5 Hz without using a needle by pressing the treatment button.
The points stimulated in this study were selected based on the clinical guidelines of acupuncture and similar studies. These points included:
Sp6 (Sanyingjiao): It is anatomically located on the ankle (five centimeters above the medial malleolus)
H7 (Shenmen): This point is located on the pisiform in the wrist
LI4 (Hugo): This point is located on the soft tissue between the thumb and index finger in the hands.
These points have been widely used in studies on sleep (13, 19-21).
Interventions were performed at the workplace of the subjects. In the real points group, the mentioned points were stimulated by the device on both sides. Based on previous studies, the number of sessions were determined eight sessions (twice per week, for one month). Each session lasted five minutes. Each point was stimulated for 50 seconds. In the sham-point group, the stimulated points were 1.5 to 2 centimeters away from the main acupoints. The control group received no intervention. One month after the first intervention session, the PSQI questionnaire was completed by the subjects again.
PSQI is a questionnaire for measuring sleep quality that identifies seven sleep areas of individuals over the past month: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction. Questions are answered by the subjects. The score of each scale of the questionnaire is between zero and three. The score of three indicates a severe problem. The sum of the scores of the seven components will constitute the total score, which is between zero and 21. A total score of five or more indicates an undesirable sleep quality (22). This questionnaire has a validity of 86.5% and a reliability of 89.5% and has been used in many studies. Several studies have been conducted in Iran on various research communities using this tool (23).
Descriptive statistics such as mean, standard deviation, and frequency; and analytical statistics such as Student’s t-test and Chi-square test were used to analyze the collected data in the SPSS-16 software.
This study was extracted from the results of a master’s dissertation in special care nursing that was approved by the ethics committee of Kermanshah University of Medical Sciences. It was also registered in the Iranian registry of clinical trials (IRCT2015021319508N2). Subjects participated in this study with informed consent.
3. Results
Of the 60 nurses who were examined initially, 36 nurses participated in the study, of whom 22 (61.1%) were female and 14 (38.8%) were male; 31 (86.1%) had a bachelor’s degree and 5 (13.8%) had a master’s degree; and 21 (58.3%) were married and 15 (41.6%) were single. The mean age of the nurses was 34.16 ± 11.34. The mean work experience of the nurses was 8.34 ± 6.71 years. Nurses were randomly divided into three groups of 12. The real points group consisted of seven females (58.3%) and five males (41.6%), the sham points group consisted of eight females (66.6%) and four males, (33.3%) and the control group consisted of seven females 58.3%) and five males (41.6%). There was no statistically significant difference in terms of age, sex, marital status, educational level, work experience, and sleep quality score among the three groups (P > 0.05).
The results of this study showed that the score of subjective sleep quality significantly decreased after the intervention in the real points group (P = 0.003), while the changes in the score of this variable in the sham points (P = 0.31) and control (P = 0.56) groups were not significant after the intervention. The score of sleep latency significantly decreased after the intervention in the real points group (P = 0.004), while the changes in the score of this variable in the sham points (P = 0.31) and control (P = 0.15) groups were not significant after the intervention. The score of sleep duration significantly decreased after the intervention in the real points group (P = 0.005), while the changes in the score of this variable in the sham points (P = 0.15) and control (P = 0.31) groups were not significant after the intervention. The score of habitual sleep efficiency significantly decreased after the intervention in the real points group (P = 0.004), while the changes in the score of this variable in the sham points (P = 0.08) and control (P = 0.31) groups were not significant after the intervention. The score of habitual sleep efficiency significantly decreased after the intervention in the real points group (P = 0.005), while the changes in the score of this variable in the sham points (P = 0.18) and control (P = 0.15) groups were not significant after the intervention. The score of use of sleeping medications was reduced after the intervention in the real points group, but it was not statistically significant (P = 0.157). Also, changes in the scores of this variable in the sham points (P = 0.317) and control (P = 0.31) groups were not significant after the intervention. The score of daytime dysfunction significantly decreased after the intervention in the real points group (P = 0.001), while the changes in the score of this variable in the sham points (P = 0.102) and control (P = 0.083) groups were not significant after the intervention. The results showed that the total PSQI score significantly decreased in the real points group after the intervention (P < 0.001). The total score in the sham points group decreased significantly, too (P = 0.016), while this difference was not significant in the control group (P = 0.31). The total score of the real points group after the intervention was significantly different from that of the sham points and control groups (P < 0.001). It should be noted that the difference in the score of this variable after the intervention was not significant between the sham points and control groups (P = 0.36). Table 1 shows the mean and standard deviation of PSQI total and components scores in the three groups before and after the intervention.
| PSQI Components | Real Points 1 | Sham Points 2 | Control 3 | P Value 1 | P Value 2 | P Value 3 |
|---|---|---|---|---|---|---|
| Subjective sleep quality | 1.91 ± 0.51 B, 0.58 ± 0.66 A | 1.83 ± 0.71 B, 1.66 ± 0.65 A | 1.58 ± 0.66 B, 1.50 ± 0.79 | 0.003 | 0.31 | 0.56 |
| Sleep latency | 2.33 ± 0.77 B, 1.00 ± 0.73 A | 2.41 ± 0.51 B, 2.25 ± 0.62 A | 2.51 ± 0.66 B, 2.25 ± 0.86 A | 0.004 | 0.30 | 0.15 |
| Sleep duration | 1.83 ± 0.71 B, 0.83 ± 0.83 A | 1.75 ± 0.62 B, 1.58 ± 0.79 A | 1.66 ± 1.07 B, 1.58 ± 0.99 A | 0.006 | 0.30 | 0.15 |
| Habitual sleep efficiency | 1.75 ± 1.21 B, 0.91 ± 0.90 A | 1.58 ± 0.90 B 1.33 ± 0.88 A | 2.16 ± 0.93 B, 2.08 ± 0.90 A | 0.004 | 0.08 | 0.12 |
| Sleep disturbances | 1.75 ± 0.75 B, 0.83 ± 0.71 A | 1.83 ± 0.71 B 1.58 ± 0.79 A | 1.91 ± 0.28 B, 2.08 ± 0.51 A | 0.005 | 0.18 | 0.15 |
| Use of sleeping medications | 0.33 ± 0.49 A, 0.16 ± 0.38 A | 0.41 ± 0.51 B, 0.38 ± 0.42 A | 0.25 ± 0.45 B, 0.30 ± 0.40 A | 0.157 | 0.31 | 0.17 |
| Daily dysfunction | 2.25 ± 0.75 B, 0.91 ± 0.79 A | 2.08 ± 0.79 B, 1.75 ± 0.75 A | 1.83 ± 0.83 B, 1.58 ± 0.90 A | 0.001 | 0.1 | 0.18 |
| Total PSQI | 12.16 ± 1.46 B, 5.25 ± 2.26 A | 11.91 ± 1.62 B, 10.50 ± 1.00 A | 11.83 ± 2.91 B, 11.41 ± 3.26 A | 0.001 | 0.016 | 0.31 |
Abbreviations: A, After; B, Before.
4. Discussion
Shift works are of the most important causes of psychological and physical disorders in nurses. The most common of these disorders is reduced sleep quality. This problem has consequences such as reduced focus and accuracy in caring for the patients, as well as reduced quality of life of the nurses. As a result, addressing the quality of sleep in this group is of paramount importance. Therefore, nurses should always be checked for sleep disorders during their working life and treated accordingly (24-26). The PSQI results of the subjects in this study indicated that this method of treatment can improve total score and components score of PSQI (excluding the use of sleeping medications index). The results of a study by Chien et al. in 2013 on 389 nurses working in night shifts showed that 75.8% of nurses had a PSQI score of over 5, which indicated the low quality of sleep in a group of health care staff (7). In terms of the effect of TEAS on the quality of sleep, the present study conform with the results of Hadded et al. in Brazil in 2011, and Timoty Kawk et al. in China in 2013 (20, 27). King et al. showed that acupuncture can be effective in improving daily dysfunction and subjective sleep quality (28). The results of a study by Tsay titled “acupressure and transcutaneous electrical acupoint Stimulation in improving fatigue, sleep quality and depression in hemodialysis patients” were consistent with this study. Their results showed that PSQI score in the real points and sham points groups was significantly lower than that of the control group after the intervention. In their study, there was no statistically significant difference between the real points and the sham points after the end of the intervention, which can be indicative of the effect of induction among the subjects of the sham-point group, which is also consistent with the present study. The results of D. Warren Spence et al. explain the physiological effects of acupuncture on the brain. They stated that acupuncture increases the sleep duration and subsequently improves sleep quality in patients with insomnia by increasing the amount of melatonin (29).
4.1. Conclusion
It is suggested that the sleeping conditions of nurses be continuously controlled by health systems and appropriate treatments be conducted in case of any disturbances. The results and their comparison with other similar studies showed that TEAS can be used as a low-cost, accessible, and low-risk method for treating sleep disorders, including poor quality of sleep in nurses.