1. Background
Aging is associated with serious changes in various biological, psychological and social domains (1). Sleep is also an area that seriously changes with old age. Studies have shown that the physiology of sleep changes in the old age (2), which is often associated with an increase in complaints about sleep (2, 3).
In this period, sleep is lighter and more disrupted, and the overall night sleep time is reduced. Sleep disorders in the old age result from intrinsic physiological changes, mental and physical comorbidities, and medications (2). Sleep hygiene is defined as behaviors that ease sleep while avoiding behaviors that cause sleep disturbance (4). In other words, sleep hygiene means habits that help people have a comfortable and good sleep, or the habit of healthy sleeping. These habits are easy, and most people are aware of them, but do not follow them at bedtime (4). The most common causes of sleep disorders, insomnia, and poor sleep are the failure to observe sleep hygiene principles. Sleep hygiene principles are small lifestyle changes that have a large impact on improving the sleep quality (5).
Insufficient sleep hygiene refers to behaviors that are in contrast with good sleep and cause insomnia. ICSDI defines this type of insomnia as follows: A sleep disorder caused by daily activities of life that prevent the continuation of sleep with high quality and complete daily alertness. Many behaviors can interfere with sleep (6). There are important recommendations on the principles of sleep hygiene that are effective in providing a comfortable sleep (7). The most common cause of sleep disorders, insomnia, and poor sleep is not respecting the principles of sleep hygiene and sleep deprivation which have adverse effects including inefficiency and undermining the body system, inability to concentrate, snoozing during the day, feeling irritable, depression, anxiety, moodiness and fatigue during the day, difficulty getting up from sleep, reduced ability of learning and memorizing, decreased performance of mental alertness, and increased violence (8). Overall sleep hygiene on the other modifiable lifestyle and environment components as well as on behaviors that can correct sleep. Often, a series of simple changes in habits or the sleeping environment can be helpful (9).
Modern life has increased human longevity through medical technology. Increasing life expectancy is associated with increased physical and mental diseases. Furthermore, patients with physical and mental diseases live a longer life. Depression, cardiovascular diseases, pulmonary diseases, malignancies, and painful diseases are common in old age (10-13). These diseases and their treatments, especially the medications, affect older adults’ sleep. Cardiovascular and hypertension medications that are extensively used in old age have an adverse effect on sleep. Many physical diseases disturb sleep and alertness. In addition, sleep may accompany physical illnesses (14).
The disruption of the sleep-wake cycle leads to the disruption of other physiological activities of the body such as loss of appetite, fatigue, lack of concentration, exacerbation of diseases and physical problems (15, 16). Given the increasing number of older people and that they spend a significant portion of their lives in the aging period, their problems are of particular importance (17).
2. Objectives
Sleep hygiene is one of the main aspects of health in older adults. Therefore, this study aimed to investigate the epidemiology of sleep hygiene in older adults and its related factors.
3. Methods
In this descriptive-analytic study, the study population consisted of all older adults aged 60 years and older in Kermanshah in 2017. They lived in the community and with their families. This study used randomized cluster sampling. The municipal districts of Kermanshah were considered clusters, of which five clusters were randomly selected. In each cluster, a number of neighborhoods were selected randomly, in each neighborhood, a number of older adults were selected with convenience sampling. After obtaining informed consent, subjects were interviewed. Among the inclusion criteria were the age of 60 and older and willingness to participate in the study. Older adults and their families were asked about substance abuse, sleeping pills, and mental disorders and their medical history was checked. Older adults who abused substances, consumed sleeping pills, and had mental disorders were excluded. The Berlin questionnaire (BQ) was used to identify those with sleep apnea. The data collection tool consisted of two parts. The first part was about demographic features including age, sex, education level, occupation, and older adults’ diseases, and the second part was the Sleep Health Index (SHI). SHI is a 13-item self-report questionnaire evaluated in 2006 by Mastin et al. (18) SHI was designed to evaluate the environmental and behavioral variables that could increase sleep disturbances (adverse effects on sleep). SHI was designed and adjusted according to the diagnostic criteria mentioned in the International Classification of Sleep Disorders (ICSD) for inadequate sleep hygiene. In this questionnaire, each item is scored with a 5-point scale (always, often, sometimes, rarely, and never). The scores for SHI range from 13 to 65, with a higher score indicating poorer sleep hygiene. To test the psychometric properties of SHI, Mastin et al. (18) used this questionnaire in a population of 632 volunteer psychology students during two semesters. These researchers calculated the Cronbach’s alpha (0.66) and test-retest reliability (0.71) for SHI. Also, Chehri et al. (19) examined the psychometrics of the Persian version of SHI in women. The internal consistency of SHI was 0.83 and it showed a good test-retest reliability (r = 0.84). The exploratory factor analysis revealed three factors: sleep-wake cycle behaviors (4 items), bedroom factors (3 items), and sleep-affecting behaviors (6 items). SPSS software V. 16, descriptive statistics (frequency distribution, mean, and standard deviation) and Kolmogorov-Smirnov, Mann-Whitney and Kruskal-Wallis tests were used to analyze the data.
4. Results
In this study, 598 individuals aged 60 - 80 years old in Kermanshah, Iran were studied in 2017. Their mean age was 68.33 ± 8.75 years, 53.3% were female, 80.6% were married, 44.8% had a high school diploma, and 24.7% were self-employed. Other demographic characteristics are presented in Table 1.
| Variables | Frequency (%) |
|---|---|
| Sex | |
| Female | 319 (53.3) |
| Male | 279 (46.7) |
| Age | |
| 60 - 70 | 421 (70.4) |
| 70 - 80 | 177 (29.6) |
| Marital status | |
| Single | 9 (1.5) |
| Married | 482 (80.6) |
| Divorced and widowed | 107 (17.9) |
| Educational level | |
| Illiterate | 203 (33.9) |
| Under high school diploma | 268 (44.8) |
| High school diploma | 85 (14.2) |
| Academic | 42 (7) |
| Occupation | |
| Housewife | 201 (33.6) |
| Unemployed | 32 (5.4) |
| Self-employed | 148 (24.7) |
| Employee | 107 (17.9) |
| Others | 110 (18.4) |
| Tea, cups | |
| None | 24 (4) |
| < 6 | 442 (73.9) |
| ≥ 6 | 132 (22.1) |
| Smoking, cigarettes | |
| None | 513 (85.8) |
| < 10 | 55 (9.2) |
| ≥ 10 | 30 (5) |
| Coffee, cup(s) | |
| None | 559 (93.5) |
| 1 | 30 (5) |
| 2 - 3 | 9 (1.5) |
In total, 14.5% of older adults had chronic headaches, 22.2% had heart diseases, 8.2% had pulmonary diseases, 2.8% had brain diseases, 17.7% had diabetes, 41.1% had hypertension, 21.7% had sleeping apnea, 49.8% snored, and 68.7% had fatigue and drowsiness.
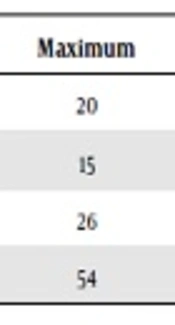
The mean score of SHI in older adults was 28.72 ± 6.99 (range: 13 - 54), and 64.5% had poor sleep hygiene (SHI > 26) Table 2.
| Variable | Number of Questions | Mean ± SD | Minimum | Maximum |
|---|---|---|---|---|
| Sleep-awake cycle behaviors | 4 | 9.93 ± 3.17 | 4 | 20 |
| Bedroom factors | 3 | 5.58 ± 2.51 | 3 | 15 |
| Sleep-affecting behaviors | 6 | 13.20 ± 3.97 | 6 | 26 |
| Sleep hygiene index (total score) | 13 | 28.72 ± 6.99 | 13 | 54 |
Kolmogorov-Smirnov test showed the non-normal distribution of SHI data.
Regarding the relationship of sleep hygiene with demographic characteristics, results showed a significant relationship between the following variables: sleep-wake cycle behaviors and education level (P < 0.002), bedroom factors and educational level (P < 0.001), and bedroom factors and occupation (P < 0.001). The findings also showed that sleep hygiene had a significant relationship with the consumption of tea, coffee and smoking habits (P < 0.001). The relationship between demographic variables and sleep hygiene is presented in Table 3.
| Variables | Sleep-Awake Cycle Behaviors | Bedroom Factors | Sleep-Affecting Behaviors | Sleep Hygiene Index (SHI) |
|---|---|---|---|---|
| Sex | ||||
| Female | 9.94 ± 3.18 | 5.63 ± 2.42 | 12.88 ± 3.64 | 28.45 ± 6.57 |
| Male | 9.93 ± 3.18 | 5.53 ± 2.61 | 13.57 ± 4.28 | 29.03 ± 7.44 |
| P value | 0.990 | 0.280 | 0.107 | 0.523 |
| Marital status | ||||
| Single | 11.22 ± 3.34 | 7.33 ± 2.50 | 13.88 ± 3.82 | 32.44 ± 4.30 |
| Married | 9.93 ± 3.16 | 5.45 ± 2.39 | 13.20 ± 4.01 | 28.59 ± 6.99 |
| Divorced and widowed | 9.82 ± 3.25 | 6.03 ± 2.92 | 13.17 ± 3.80 | 29.03 ± 7.15 |
| P value | 0.270 | 0.072 | 0.778 | 0.101 |
| Education | ||||
| Illiterate | 9.79 ± 2.94 | 6.15 ± 2.39 | 12.50 ± 3.25 | 28.45 ± 6.30 |
| Under high school diploma | 9.66 ± 2.98 | 5.42 ± 2.48 | 13.59 ± 4.20 | 28.67 ± 6.96 |
| High school diploma | 11.31 ± 3.96 | 5.05 ± 2.38 | 13.35 ± 4.45 | 29.72 ± 8.54 |
| Academic | 9.57 ± 3.03 | 4.92 ± 2.44 | 13.83 ± 4.20 | 28.33 ± 7.03 |
| P value | 0.002 * | 0.001 * | 0.050 | 0.801 |
| Occupation | ||||
| Housewife | 10 ± 3.22 | 5.46 ± 2.42 | 12.73 ± 3.70 | 28.20 ± 6.64 |
| Unemployed | 10.37 ± 2.21 | 6.12 ± 2.02 | 13.06 ± 3.56 | 29.56 ± 5.15 |
| Self-employed | 9.65 ± 2.85 | 5.45 ± 2.36 | 13.66 ± 4.10 | 28.77 ± 6.71 |
| Employee | 10.41 ± 3.86 | 5.03 ± 562 | 14.06 ± 4.74 | 29.51 ± 8.33 |
| Others | 9.60 ± 2.98 | 6.33 ± 2.77 | 12.67 ± 3.35 | 28.61 ± 7.06 |
| P value | 0.178 | 0.001 * | 0.099 | 0.655 |
| Tea, cups | ||||
| None | 9.95 ± 3.77 | 5.54 ± 3.006 | 13.16 ± 3.71 | 28.66 ± 7.96 |
| < 6 | 9.97 ± 3.15 | 5.37 ± 2.44 | 12.95 ± 3.89 | 28.29 ± 6.79 |
| ≥ 6 | 9.81 ± 3.17 | 6.28 ± 2.54 | 14.08 ± 4.18 | 30.18 ± 7.33 |
| P value | 0.928 | 0.001 | 0.044 | 0.021 |
| Smoking, cigarettes | ||||
| None | 9.95 ± 3.23 | 5.50 ± 2.49 | 12.76 ± 3.81 | 28.22 ± 6.91 |
| < 10 | 9.81 ± 2.72 | 5.81 ± 2.46 | 14.63 ± 3.14 | 30.27 ± 6.26 |
| ≥ 10 | 9.90 ± 3.11 | 6.43 ± 2.84 | 18.20 ± 4.08 | 34.53 ± 6.79 |
| P value | 0.944 | 0.154 | 0.001 | 0.001 |
| Coffee, cup(s) | ||||
| None | 9.86 ± 3.15 | 5.57 ± 2.47 | 13.10 ± 3.90 | 28.54 ± 6.89 |
| 1 | 10.33 ± 3.45 | 5.60 ± 3.20 | 14.30 ± 4.99 | 30.23 ± 8.33 |
| 2 - 3 | 13.11 ± 1.76 | 6.33 ± 2.39 | 15.88 ± 3.51 | 35.33 ± 5.07 |
| P value | 0.003 | 0.459 | 0.041 | 0.005 |
The relationships of sleep hygiene with underlying diseases in the study population are presented in Table 4. The findings of the Mann-Whitney test showed a significant difference between sleep hygiene and pulmonary diseases (P < 0.001), diabetes (P < 0.002), sleep apnea (P < 0.001), snoring (P < 0.001), and fatigue and drowsiness during sleep (P < 0.001).
| Variables | Frequency (%) | Sleep-Awake Cycle Behaviors | Bedroom Factors | Behaviors Affecting Sleep | Sleep Hygiene Index (SHI) |
|---|---|---|---|---|---|
| Chronic headache | |||||
| Yes | 87 (14.5) | 9.66 ± 3.17 | 5.4 ± 2.26 | 14 ± 4.26 | 29.06 ± 7.17 |
| No | 511 (85.5) | 9.98 ± 3.18 | 5.61 ± 2.55 | 13.07 ± 3.9 | 28.37 ± 6.97 |
| P value | 0.594 | 0.588 | 0.051 | 0.710 | |
| Cardiac diseases | |||||
| Yes | 133 (22.2) | 10.27 ± 3.11 | 5.9 ± 2.71 | 13.62 ± 3.95 | 29.81 ± 7.09 |
| No | 465 (77.8) | 9.83 ± 3.19 | 5.49 ± 2.44 | 13.09 ± 3.97 | 28.41 ± 6.94 |
| P value | 0.193 | 0.153 | 0.196 | 0.055 | |
| Pulmonary diseases | |||||
| Yes | 49 (8.2) | 10.89 ± 3.37 | 5.52 ± 2.46 | 15.75 ± 4.64 | 28.35 ± 6.78 |
| No | 549 (91.8) | 9.85 ± 3.15 | 6.26 ± 2.96 | 12.98 ± 3.82 | 32.91 ± 8.01 |
| P value | 0.027b | 0.114 | 0.001b | 0.001b | |
| Brain diseases | |||||
| Yes | 17 (2.8) | 10.29 ± 3.56 | 6.41 ± 3.12 | 15.75 ± 4.64 | 32.91 ± 8.01 |
| No | 581 (97.2) | 9.92 ± 3.17 | 5.55 ± 2.49 | 12.98 ± 3.82 | 28.35 ± 6.78 |
| P value | 0.681 | 0249 | 0.125 | 0.067 | |
| Diabetes | |||||
| Yes | 106 (17.7) | 10.54 ± 3 | 6.24 ± 2.59 | 13.80 ± 3.81 | 30.59 ± 6.82 |
| No | 492 (82.3) | 9.80 ± 3.2 | 5.44 ± 2.47 | 13.08 ± 3.99 | 28.32 ± 6.97 |
| P value | 0.014b | 0.002* | 0.112 | 0.002b | |
| Hypertension | |||||
| Yes | 246 (41.1) | 10.24 ± 3.05 | 5.79 ± 2.68 | 13.29 ± 4.03 | 29.33 ± 6.68 |
| No | 352 (58.9) | 9.72 ± 3.24 | 5.43 ± 2.37 | 13.15 ± 3.93 | 28.3 ± 7.18 |
| P value | 0.072 | 0.193 | 0.700 | 0.098 | |
| Sleep apnea | |||||
| Yes | 130 (21.7) | 10.8 ± 3.38 | 6.38 ± 2.81 | .1514.82 ± 4 | 32 ± 7 |
| No | 468 (78.3) | 9.69 ± 3.08 | 5.36 ± 2.38 | 12.76 ± 3.84 | 27.81 ± 6.67 |
| P value | 0.004b | 0.001b | 0.001b | 0.001b | |
| Snoring | |||||
| Yes | 298 (49.8) | 10.41 ± 3.30 | 5.89 ± 2.63 | 13.73 ± 3.97 | 29.93 ± 6.74 |
| No | 300 (50.2) | 9.46 ± 2.97 | 5.27 ± 2.34 | 12.05 ± 3.72 | 26.08 ± 6.81 |
| P value | 0.004 | 0.004 | 0.001b | 0.001b | |
| Fatigue and drowsiness | |||||
| Yes | 411 (68.7) | 10.37 ± 3.14 | 5.82 ± 2.58 | 13.73 ± 3.97 | 29.93 ± 6.74 |
| No | 187 (31.3) | 8.96 ± 3.04 | 5.06 ± 2.28 | 12.05 ± 3.72 | 26.08 ± 6.81 |
| P value | 0.001b | 0.001b | 0.001b | 0.001b |
aValues are expressed as mean ± SD unless otherwise indicated.
bSignificant at P < 0.05
Also, the results of the logistic regression test showed that sleep hygiene in older adults is reduced with increasing smoking and increasing age. Furthermore, diabetes, fatigue, drowsiness, and sleep apnea were of the most important factors affecting sleep hygiene.
5. Discussion
The aim of this study was to investigate the epidemiology of sleep hygiene in older adults and its related factors. In this study, older adults described their sleep hygiene status as moderate, and there was no significant difference between men and women. Also, sleep hygiene had no significant relationship with marital status, education, and occupation of older adults. Meanwhile, in a study by Khazaie et al. who studied sleep hygiene patterns in Iranian adult population, sleep hygiene had a significant relationship with sex, age, occupation, and marital status of patients (20). This inconsistency can be due to the difference in the mean age of the two populations, that is, the population in their study was younger than ours (35 vs. 68.33) (20). Cho et al. (21) reported a significant correlation between SHI and age.
In a study by Golenkov and Poluektov (22), women and educated individuals had the highest awareness of sleep hygiene. These were consistent with the present study. Also, sleep hygiene had no significant relationship with the education of older adults. The reason for this difference can be due to the difference in the mean age of the population in the two studies.
Among the most important diseases affecting sleep hygiene, sleep-wake cycle behaviors, bedroom factors, and sleep-affecting behaviors were pulmonary diseases and diabetes, apnea and snoring, and fatigue and drowsiness. Few studies have been done in this regard.
In the present study, sleep hygiene in older adults had a significant relationship with drinking tea, drinking coffee, and smoking, which was in line with the studies by Irish et al. (23) and Nobahar and Vafai (24). Golenkov found that the lowest awareness about sleep hygiene was that of alcohol users and smokers.
Kline et al. (25) reported that women with insomnia who observed more sleep hygiene behaviors had fewer insomnia problems than those with fewer sleep hygiene behaviors. Tea consumption was higher in women with less sleep hygiene behaviors.
The present study found no significant relationship between sleep hygiene and chronic headache. Cho et al. (21) examined sleep hygiene in a group of patients with chronic pain. The results showed that among sleep hygiene-related indicators, sleep disturbing behaviors and irregular sleep-wake cycle were most affected by chronic pain. This means that people with chronic pain have more problems in terms of disruption and sleep-wake disorder. Ellis et al. (26) reported that sleep hygiene can help reduce insomnia. McCrae et al. (27) also concluded that the effectiveness of sleep hygiene as a treatment for insomnia in later years of life, are questionable and need further research.
5.1. Conclusions
Sleep hygiene in older adults is affected by physical and psychosocial factors. In order to help improve the health and quality of sleep in older adults, it is recommended that comprehensive and practical solutions be considered. Plans to increase awareness, training sleeping time hygiene behaviors, providing consulting services to older adults, and improvement of their health and medical services should be considered.