1. Introduction
McCain-Albright syndrome (MAS) is a rare disease, with a prevalence of 1/1,000,000 to 1/100,000 which is characterized by Café-au-lait skin spots, polyostotic fibrous dysplasia (PFD), endocrine disorders such as hyperthyroidism, Cushing’s syndrome, PP, rickets/osteomalacia, excessive growth hormones and hepatic and cardiac involvements (1, 2). MAS is a rare sporadic disease characterized by bone fibrous dysplasia, café-au-lait skin spots and a variable association of hyperfunctional endocrine disorders. Fibrous dysplasia of bone (FD) may include single or multiple skeletal sites, and presents by touch and/or pain and sometimes pathological fractures. Advanced accelerated scoliosis is also common in this syndrome. In addition to PP (vaginal bleeding, sputum smear and enlargement of the testicles in girls and penis, and early sexual behavior in boys), may include other endocrine disruptions, including hyperthyroidism, over-growth hormones, Cushing’s syndrome and panic disorders.
MAS-related malignancies are uncommon because the potential malignant changes in FD lesions occur in less than 1% of MAS cases (3).
2. Case Presentation
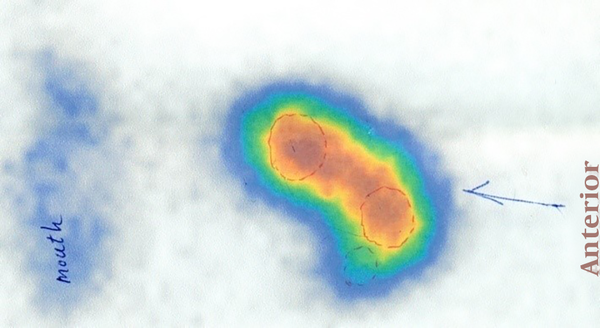
A 1.21-meter-high 8-year-old boy with a weight of 21.5 kg, a head circumference of 55 cm and puberty tanner stage of one first presented to the physician in 2013 at the age of 4 with the chief complaint of recurrent femoral fractures and with a history of hyperthyroidism for the last two years as well as several admissions in Firouzgar Hospital in Tehran, Iran for femoral fractures, although he did not have any significant family history. Physical examinations revealed cutaneous Café -au-lait spots and multiple thyroid nodules in the right and left lobe of the thyroid fig. After he was admitted to the orthopedic ward at the age of 5, the fracture and dislocation were fixed using spica casts, and the biopsy of the femur lesion suggested pathologic femoral fractures. Pathology reports confirmed FD and ruled out MAS. The whole-body scan was then performed, and given the patient’s history, the findings were in favor of PFD involving both orbitals, the skull base, both parietal bones, both temporal bones, the maxilla and mandible, left humerus, left radius, left acetabular roof, left femur, left tibia and left talus bone. The thyroid ultrasound performed in 2015 also revealed four heterogeneous solid masses with 16-, 17-, 20- and 20-mm microcytic regions in the left lobe and two 7- and 10-mm masses in the right lobe without a cervical adenopathy. The next year, TSH was measured as < 0.005 mIU/mL, free T4 as 21.8 pmol/L, T4 as 16.5 Ug/dL, T3 as 4.2 nmol/L and T-uptake as 1. The thyroid scan performed in 2015 suggested multinodular goiters with two prominent warm nodules in the upper pole of the left lobe and isthmus. The level of Ca was also found to be 9.97 mg/dL, P to be 4.2 mg/dL, AST 24 U/L, ALT 26 U/L, ALP 783 U/L and PTH 154.4 pg/mL. Moreover, the echocardiography and dynamic MRI of pituitary were normal (Figures 1 - 4).
3. Discussion
FD is a rarely skeletal malformation due to the mutation in the GNAS1 gene located on the long arm of chromosome 20 at position 13.3 (2).
FD is classified into two forms, namely monostotic and polyostotic. The monosodic form is more common and less symptomatic, although the polymyostetic form is less common and is associated with excessive endocrinopathy, which mainly includes hyperthyroidism and PP (4), as well as Café-au-lait spots that constitute MAS (1).
In this case, PFD causes fetal resection of the pathologic fractures, although it can show itself with pain, deformity and walking abnormalities (5).
FD can be detected using X-rays and used less bone biopsy (6). Café-au-lait spots are usually the first manifestation of a disease that occurs soon or after birth. Thyroid ultrasound and fungi and biochemical/hormonal studies can detect repeated endocrinopathies (1).
Although no uncontrolled study confirms that treatment with hypophosphatemia reduces fracture or improves pain, the observation of treated patients suggests that treatment can improve the results. Hypophosphatemia can be treated in the same way that other FGF23-mediated phosphate wasting disorders are treated and include the use of phosphate and active vitamin D (calcitriol or alfacalcidiol) (3).
The usual sign is an increase in the velocity of growth. However, if GH is too much in association with PP, clinical signs of increased growth rates can be hidden. Almost all GH patients are overly dependent on FD/MAS with high prolactin levels (7).
The results of the OGTT can be equivocal in subtle diseases, especially in young children. Frequent overnight samplings, i.e. every 20 minutes, can be helpful in these difficult cases. Children with excessive GH lack any intervals when the GH value is less than 1 ng/mL (1).
Excessive GH treatment in FD/MAS is almost exclusively restricted to medical treatment. Due to the massive extension of the skull base with FD, which includes the termination of the sinus spinach, the traditional transfenoid approach to the pituitary is impossible or very difficult. The surgical treatment of excessive GH in FD/MAS normally requires a complete hypophysectomy, i.e. a treatment that can be probably best postponed to young adulthood. Radiation is rarely considered an acceptable approach, given that doses of radiation therapy in FD are associated with an increase in malignant transformation (8).
3.1. Conclusions
Given that MAS clinically manifests later in the course of recurrent periods of PP and cyst formation, careful clinical observations and the follow up of the patients are essential for the diagnosis of MAS. The association of primary hyperparathyroidism with FD/MAS is questionable, as hyperparathyroidism did not present a molecularly-driven association. Parathyroid neoplasms do not have an activating mutations in Gsα, which causes hyperparathyroidism or a parathyroid adenoma.