1. Background
Cardiovascular diseases are the leading cause of mortality across the world. According to statistics, 30% of deaths (approximately 17.3 million deaths per year) and 330 million disabilities per year are caused by cardiovascular diseases (1). The prevalence of heart failure due to cardiovascular diseases has been reported to be 5.8 million per year in the United States and 23 million in the world (2). Moreover, the associated five-year mortality has been reported to be higher than 75%, which is a major health concern after the first hospitalization (3).
Cardiovascular diseases are a major cause of mortality in Iran, which impose significant costs on the healthcare system of the country each year. According to the statistics in Iran, the prevalence of coronary artery disease and the associated mortality is on the rise. In 2001, 317 and 116,000 patients died due to cardiovascular diseases in Iran per day and year, respectively (4). Despite the advancement in invasive treatments such as coronary artery bypass grafting (CABG) and angioplasty, the mortality rate of cardiovascular diseases remains high in the patients.
Exercise-based cardiovascular rehabilitation (CR) could reduce cardiovascular mortality by 25% - 50% as an important component of the comprehensive program for the secondary prevention of cardiac diseases (5). In general, CR could decrease cardiovascular mortality with targeted efforts focused on physical exercise, lipid control, hypertension control, and smoking cessation (4). However, use of rehabilitation services is less common compared to the expected rate, and various data in the United States are indicative of the participation of only 31% of the patients undergoing CABG in CR programs. This rate has been estimated to be less than 15% in Iran, and a major cause of this issue is the lack of proper knowledge regarding the beneficial therapeutic effects of CR (5). It is also notable that heart failure caused by cardiac surgeries has been overlooked in CR programs (6, 7). Therefore, it is essential to determine the influential factors in the prognosis of these patients.
Heart failure is often induced by ischemia and myocardial infarction, and ischemia caused by the process of atherosclerosis has been recognized as a multistage inflammatory disease. Several environmental and hereditary factors affect the involvement of inflammatory cytokines, such as obesity, diabetes, and fat deficiency (8). In this regard, the most commonly assessed inflammatory markers include interleukin 6 (IL-6) and high‐sensitivity C‐reactive protein (hsCRP) (9, 10). CRP is produced by hepatocytes and is regulated by IL-6, and these agents are found in the endothelium of the atherosclerotic plaques, acting based on the changes in access to nitric oxide and leading to the onset and progression of atherosclerosis through the increased adhesion of inflammatory cells to the endothelium (11). Several studies have indicated that increased cytokines (especially IL-6) could severely modify the cardiac function, thereby damaging myocytes. Furthermore, increased plasma IL-6 levels are significantly associated with left ventricular dysfunction and play a pivotal role in the progression of cardiac failure. Given the importance of these markers in the pathophysiology of cardiac failure, the positive effects of exercise training have been highlighted in various populations, which result in diminishing the effects of the mentioned factors on cardiovascular diseases (12).
The international studies in this regard have demonstrated the effects of CR on hsCRP and IL-6 (12-14), proposing contradictory findings (15-20). Moreover, similar research has been performed at the Cardiac Rehabilitation Center of Imam Ali Hospital in Kermanshah, Iran, which has been mainly focused on exercise performance and lipid profiles.
2. Objectives
The present study aimed to evaluate the effects of CR on cardiac function (e.g., ejection fraction and diastolic function) and hsCRP and IL-6 as inflammatory markers to indicate the prognosis of cardiac failure. We attempted to determine whether eight weeks of aerobic exercises could influence the cardiac function and inflammatory markers in male patients with heart failure following CABG.
In Iran, most cardiac patients return to everyday life following cardiac surgeries and refer to the hospital again shortly due to irreparable complications (e.g., heart failure and myocardial infarction) due to the lack of control of the predisposing factors (e.g., sedentary state, increased lipid profile, diabetes, and obesity), which are directly correlated with inactivity. At this stage, re-treatment is often extremely difficult and even impossible. The current research also aimed to evaluate the effects of aerobic exercises on cardiac function and inflammatory markers of IL-6 and hsCRP, which play a key role in the complications and prognosis of the severity of cardiac failure.
3. Methods
This study was conducted on 20 male patients with heart failure aged 50 - 60 years, who were admitted to Imam Ali Hospital in Kermanshah, Iran and had undergone GABG in the past eight weeks. The patients had contractile performance of less than 50%. They were selected and divided into two groups of 10. The first group included the patients with a sedentary state who were not willing to perform the RC program (control), and the second group included the patients who performed aerobic exercises (intervention). After admission and counseling, written informed consent was obtained from the participants, and they received a complete examination by a cardiologist.
The inclusion criteria of the study were as follows: (1) no smoking habits, (2) no orthopedic complications or other disease preventing participation in the research, (3) stable cardiac state, (4) absence of pain and high-risk arrhythmia, and (5) consumption of similar medications. The exclusion criteria were the emergence of symptoms or new diseases, voluntary withdrawal from the study, and absence in the exercise sessions for more than two sessions.
On the first day, the patients were fully examined, and their vital signs and primary echocardiographic findings were recorded after 20 minutes of rest in a seated position. Afterwards, blood samples were collected in the fasting state to evaluate the levels of IL-6 and hsCRP, followed by the coding, centrifugation, and freezing of the samples. The mentioned stages and final echocardiography were repeated in both groups after the intervention, and the blood samples were separately assessed using the IL-6 ELISA kit (Diaclone Co., made in France) and hsCRP ELISA kit (Boditech Co., made in Korea) for each hormone in a specialized laboratory.
The aerobic exercise protocol consisted of 24 exercise sessions (three sessions per week), and session included warm-up (10 minutes; stretching moves and brisk walking), followed by 30 minutes of running on a treadmill (COSMOS, Germany) at the intensity of 60% - 70% the maximum heart rate and cool-down (10 minutes; walking on the treadmill) (6).
3.1. Sample Population
The sample population included 20 male patients aged 50 - 60 years, who were admitted to Imam Ali Hospital in Kermanshah due to cardiac failure. The patients had ejection fraction of less than 50% and had undergone CABG within the past eight weeks. The patients were randomly selected and divided into the intervention and control groups (10 per each).
3.2. Statistical Analysis
Data analysis was performed in the PRISM software using descriptive statistics to estimate the mean values, paired and Independent t-test to compare the mean values in the case of the normal distribution of the data, and Wilcoxon test for the data with non-normal distribution.
4. Results
4.1. Descriptive Results
Table 1 shows the mean age and height of the patients in the intervention and control groups. Considering the lack of changes in these variables after the intervention, the study groups were compared using Independent t-test. The results of the Kruskal-Wallis test indicated a significant difference between the groups in terms of the exercise level after the intervention. Moreover, the results of Mann-Whitney U test indicated significant differences between the group training and telemdicine groups (P = 0.001), group training and control groups (P < 0.0001), and telemedicine and control groups (P = 0.003) in terms of the exercise level after the intervention (Table 3).
| Variable | Control | Intervention | Total | P Value |
|---|---|---|---|---|
| Age, y | 55.7 ± 5.539 | 54.8 ± 7.193 | 55.25 ± 6.265 | 0.757 |
| Height, cm | 169.7 ± 5.229 | 170.2 ± 6.321 | 169.95 ± 5.652 | 0.849 |
Table 2 shows the mean variables and standard error of the mean (SEM) of the intervention and control groups. These variables could change due to the effects of the intervention and were evaluated after the intervention.
| Group | Pretest | Posttest |
|---|---|---|
| Left ventricular ejection fraction (LVEF) | ||
| Aerobic exercises | 40.5 ± 6.433 | 49 ± 5.164 |
| Control | 43 ± 3.496 | 45.5 ± 1.581 |
| IL-6 | ||
| Aerobic exercises | 3.712 ± 2.134 | 1.678 ± 0.8604 |
| Control | 4.588 ± 3.177 | 3.698 ± 2.091 |
| hsCRP | ||
| Aerobic exercises | 1.79 ± 1.687 | 0.7496 ± 0.5651 |
| Control | 1.949 ± 0.9 | 2.069 ± 0.8715 |
Table 3 shows the differences in the mean variables after the intervention. At this stage, Paired t-test and multivariate analysis were applied for the statistical analysis and estimation of the adjusted P value, respectively. P value could be used when only one variable is assessed; however, we had several variables in the present study, which necessitated the use of adjusted P value to reduce analysis error level. The mean differences were considered significant if the adjusted P value was less than 0.05. Additionally, the Wilcoxon test was applied for the analysis of the data with non-defined t and abnormally distributed degree of freedom (df) (Table 3).
| Variables | Mean Difference | SD of Mean Difference | 95% Confidence Interval of Difference Lower Upper | t | df | P Value | Adj. P Value |
|---|---|---|---|---|---|---|---|
| LVEF | 8.5 | 4.74 | 0.0039 | 0.0094 | |||
| IL-6 | -2.03 | 1.51 | 0.002 | 0.03 | |||
| hsCRP | -1.04 | 1.339 | -1.998 - 0.8265 | 2.457 | 9 | 0.0363 | 0.075 |
4.2. Inferential Results
4.2.1. Effect of Eight Weeks of Aerobic Exercises on Cardiac Systolic Function
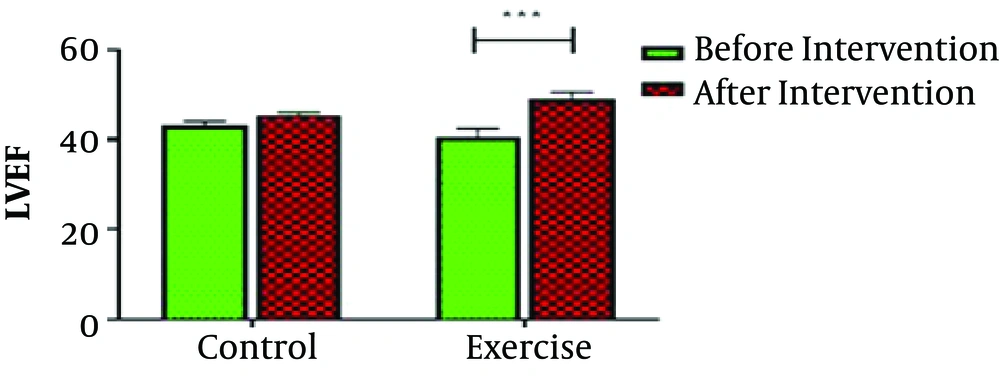
After determining the left ventricular ejection fraction (LVEF) level in the patients, the PRISM software was used to evaluate LVEF after eight weeks of the intervention, and no significant changes were observed in the LVEF of the control group (P < 0.05). However, the variable significantly increased after eight weeks of aerobic exercises (P = 0.0039) (Figure 1).
4.2.2. Effect of Eight Weeks of Aerobic Exercises on Cardiac Diastolic Dysfunction
Table 4 shows the difference in the diastolic dysfunction of the control subjects before and after the intervention. The obtaiend results were indicative of no significant changes in this regard (P > 0.05) (Table 4).
| Group | Pretest, No. (%) | Posttest, No. (%) | P Value |
|---|---|---|---|
| Intervention | 7 (70) | 7 (70) | 1 |
| Control | 8 (80) | 8 (80) | 1 |
4.2.3. Effects of Eight Weeks of Aerobic Exercises on IL-6 and hsCRP
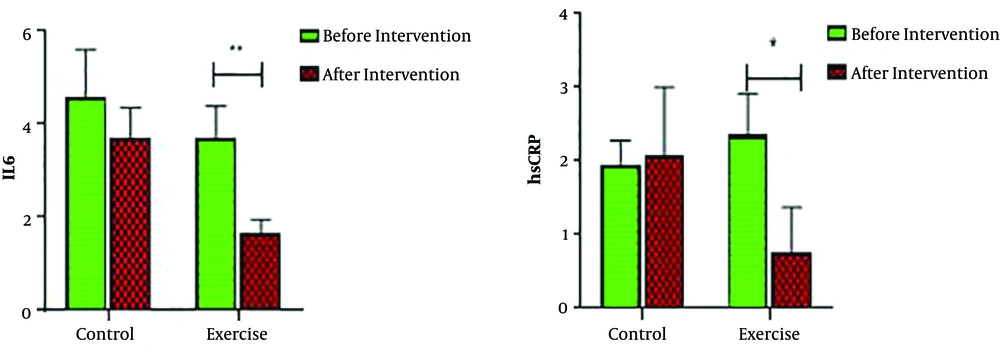
After determining the level of IL-6 in both groups, the variable was evaluated using the PRISM software, and no significant changes were observed in IL-6 level in the control group (P < 0.05). However, IL-6 significantly decreased after eight weeks of aerobic exercises (P = 0.002). Evaluation of the hsCRP level in the study groups showed no significant changes in this regard in the control group after eight weeks of aerobic exercises (P < 0.05). Nonetheless, hsCRP significantly decreased after eight weeks of aerobic exercises (P = 0.036) (Figure 2).
5. Discussion
Exercises could be an opportunity for patients to participate in CR programs as they are cost-efficient and appealing. In addition, CR could be implemented as multilateral programs to enhance the mental health and functional capacity of patients with cardiovascular diseases, who could apply this technique as a complementary program for disease management after diagnosis. Several studies have been focused on the effects of special rehabilitation exercises, while there is a lack of consensus regarding the severity, duration, and types of CRs. Moreover, researchers have investigated various exercise protocols in detail (e.g., aerobic exercises, endurance training, and their combination) in order to further recognize the health benefits of physical exercise (21).
As is illustrated in Figure 1, no significant changes were observed in the LVEF of the healthy control group, while LVEF significantly increased in the intervention group after eight weeks of aerobic exercises. In other words, the aerobic exercises significantly improved the systolic function of the patients, which is in line with the results obtained by Basati et al. and Belardinelli et al. (16, 20).
Evaluation of the diastolic function in the present study indicated no significant difference between the intervention and control groups in this regard, which is consistent with the study by Golabchi et al., which was conducted on cardiac patients following myocardial infarction. In the mentioned study, lengthy physical exercise was recommended to improve the effects (15-20). Inconsistent with our findings, Edelman et al. reported the improved diastolic function of the subjects following endurance training (17). The discrepancy between the aforementioned studies might be due to the difference in the age of the subjects in the study groups since diastolic function is age-dependent (1), progressing with increased aged in an irreversible manner.
As is depicted in Figure 2, the IL-6 analysis demonstrated the significant reduction of this variable in the intervention group, while no significant changes were denoted in the control group. Moreover, our findings demonstrated no significant changes in the hsCRP levels in the control group, while hsCRP significantly decreased in the intervention group after eight weeks of aerobic exercises, attesting to the effectiveness of aerobic exercise in the reduction of inflammatory factors. Our findings in this regard are in line with the results obtained by Beckie et al. (12). However, the only difference was that the mentioned study was performed on patients with coronary artery disease, while the current research was conducted on the male patients with cardiac failure after CABG. Therefore, our results demonstrated that the reduction of IL-6 was associated with the decreased causes of atherosclerosis.
In a meta-analysis in this regard, Sadeghi et al. evaluated 15 articles, all of which reported the reduction of hsCRP after rehabilitation for three, 3 - 8, and more than eight weeks (18). On the other hand, Jorgensen et al. reported no reduction in the IL-6 and hsCRP levels after an eight-week rehabilitation program, while 12 weeks of the rehabilitation program could decrease both these markers (19). The difference between the mentioned study and our research was the assessment of the patients after CABG since undergoing surgery could excessively increase inflammatory markers. Therefore, longer periods of aerobic exercises were associated with the more significant reduction of these markers.
5.1. Conclusions
According to the results, the reduction of inflammatory markers could improve cardiac function and muse be considered indispensable to treatment and prevention. Therefore, it is recommended that efforts be made to develop this issue in all cardiovascular treatment centers and further longitudinal investigations be conducted on larger sample sizes.
5.2. Research Indications
It is strongly recommended that further longitudinal investigations be conducted on larger sample sizes.