1. Introduction
Lower limb injuries are prevalent in a wide range of sports and outdoor activities (e.g., football, parkour, horse-riding, cycling, skiing, hockey, baseball, lawn tennis, volleyball, kabaddi, long and high jumps, and discus and javelin); they often require urgent care and surgical intervention (1).
The surgery and postoperative immobilization can lead to several complications, e.g., altered kinetics and kinematics, abnormal joint range of motion (ROM), joint stiffness (2), power and strength, cross-sectional area of muscles (2), and reduced joint moment (2). These issues are particularly pronounced in cases of Achilles tendon rupture and severe shank injuries, which can result in long-term stiffness and reduced mobility. The impact of such complications on an athlete's performance and overall well-being is significant. A study showed that 2-6 years after Achilles rupture repair, the tendon has more stiffness, and no elongation causes deficits in plantar flexion moment production. These data support the claim that post-rupture tendon regeneration leads to the production of a tissue that is functionally unlike a non-injured tendon (3). Conversely, severe injuries of the shank demand a below-the-knee cast, which alters ankle biomechanics, especially when worn for a long time (4). It prevents plantarflexion after heel contact and dorsiflexion after midstance. It is reported that biomechanical changes (including alterations in plantar flexion and ankle angles during gait) contribute to frontal and sagittal plane pelvic tilt (5). Dorsiflexor muscles are strongly prone to reduced strength, i.e., 28% in 40-day immobilization in a weight-bearing position (6).
To date, numerous surgical and conservative interventions have been studied for the management of postoperative complications with the aim of improving patient outcomes while minimizing harm during the healing process. In assessing rehabilitation options, a variety of exercises and physiotherapy interventions have been evaluated, including but not limited to stretching (7), which has been found to help restore normal ROM, while myofascial release using a foam roller on the shank has proven effective in reducing gastrocnemius stiffness and increasing dorsiflexion ROM. Strength (7) training aids in regaining muscle power and normal moment production (8). Graston's (9) technique has demonstrated the ability to reduce muscle and tendon stiffness. Combining multiple techniques has shown promise in achieving superior results, as evidenced by improved outcomes when vibration (10) or heating (11) is used in conjunction with stretching or Instrument-Assisted Soft Tissue Mobilization (IASTM) combined with electrotherapy (12).
While various interventions and rehabilitation techniques have been explored to address these challenges, there is a need for comprehensive studies that assess the efficacy of combined interventions in managing postoperative complications, especially in rare conditions. This case study focuses on a 41-year-old female athlete with a complex history of tibia, fibula, and calcaneus fractures, as well as Achilles tendon rupture, resulting in decreased muscle strength, limited ankle ROM, and excessive stiffness in the right foot. Given the rarity of this condition, no published studies have assessed the combination of interventions used in this study for rehabilitation in similar cases. Therefore, this case study aims to provide valuable insights into managing postoperative complications, specifically addressing balance, muscle strength, pain, quality of life, and ankle ROM. By examining the unique challenges faced by this individual and the effectiveness of a combination of interventions, we aim to contribute to the advancement of postoperative rehabilitation for similar rare conditions.
2. Case Presentation
2.1. Case Description
A 41-year-old female athlete who has been exercising since the age of 10 and her right shank (facture of tibial, fibula, and calcaneus and Achilles tendon rupture) was broken in a big jump at the age of 34 and had gone through several surgeries and complications (13 surgeries). The patient has been capable of walking after 3.5 years (at the age of 37.5). The patient had 2 cm of leg length discrepancy due to reduced heel fat pad and ankle joint interarticular space, reduced muscle strength, and ankle dorsiflexion ROM. Thus, she uses an orthosis under the right heel. Also, she had a stiff ankle and MTPs in all dimensions (age: 41 years, height: 1.68 m, mass: 59 kg, body mass index (BMI): 20.9, leg length: Right: 84.5 cm and left: 86.5 cm). The participant continued to do daily workouts (including swimming and fitness training) and did not make any changes to the exercise routine. The effect of interventions was assessed from Dec 2022 until Mar 2023. The experiments reported in the manuscript were performed in accordance with the ethical standards of the Helsinki Declaration. This study was approved by the Research Ethics Committees of the Faculty of Physical Education and Sport Sciences, Tehran University (IR.UT.SPORT.REC.1401.045). Written informed consent was obtained from the participant for publication of this study and any accompanying images.
2.2. Questionnaires
SF-36 (13), Achilles Tendon Rupture Score (ATRS) (14), Foot And Ankle Ability Measure (FAAM) (15), and Foot and Ankle Outcome Score (FAOS) (16) questionnaires were answered at the beginning of each stage by the participant. The Visual Analog Scale (VAS) was answered during the balance test pre- and post-test.
2.3. Static and Dynamic Single-Leg Stability
The Biodex Balance SD System (BBS; Biodex Medical System Inc., Shirley, NY, USA) was used to measure static and dynamic single-leg balance. The participant was asked to stand stationary on the BBS platform with her arms crossed over her chest and maintain visual focus on the liquid crystal display. The participant was instructed to stand with the right leg, and the left leg was flexed at 90° (17). We adopted the instructions used in a previous study (17).
Dynamic postural stability was assessed for single-leg stance on level 10. The participant was barefoot in a quiet laboratory, and the device screen was covered to minimize visual compensation, wherein she performed 3 trials of 20 seconds each for the right leg, with a 1-minute rest period between each trial.
2.4. Single-Leg Balance Path Length and Area
Static balance was measured while the participant stood on a foot pressure instrument (FDM-S; Zebris Medical GmbH, Weitnau-Seltmans, Germany) with the other limb in 30 of hip flexion and 45 of knee flexion and hands on hips. She was instructed to “stand as still as possible.” The participant performed 3 practice trials, followed by 3 successful 10-second trials with eyes open and 1-minute rest between trials. Failed trials in which the participant moved out of the test position were repeated (18).
2.5. Isokinetic Measurements
The foot of her test limb was firmly strapped to the dynamometer footplate. The lateral malleolus was aligned with the axis of rotation of the dynamometer head, and, using the lateral femoral condyle and the greater trochanter, the knee was positioned in a statically flexed position (10°; goniometer).
2.6. Passive Dorsiflexion Stiffness
The non-weight-bearing dorsiflexion ROM was measured following instructions used by Whitting et al. 2013 (19). Passive dorsiflexion stiffness was calculated by measuring the slope of the torque-angle curve generated for 1° to 6° dorsiflexion (20).
2.7. Isokinetic Plantarflexion and Dorsiflexion Testing
The participant was able to do the test only at 180°/s; thus, isokinetic plantarflexion and dorsiflexion testing was performed at 180°/s, which was the only speed that the participant was able to do the test, recorded at 1000 Hz. During test contractions, the participant was instructed to move her ankle through her full ROM as fast as possible, as well as to push and pull as hard as possible in each direction. Strong verbal encouragement was provided throughout testing. To ensure similar contraction times between different velocities, she performed 10 isokinetic repetitions.
3. Intervention
Interventions were delivered by a registered physiotherapist (HM) and instructor (FKH). The program consisted of 3 sessions per week for 12 weeks; the participant warms up for 5 minutes, moving the ankle in 3 planes of movement. Two interventions were prescribed, i.e., IASTM techniques based on the manual for the Graston technique and Faradic electrotherapy. The interventions were applied on separate days alternatively. One day electrotherapy on tibialis anterior, gastrocnemius muscles and foot soles. Myofascial release (8), friction massage (21), and Graston technique using GT5, GT6 and GT2 on calf muscles (22), Achilles tendon, sole of the foot and on the spots with adhesions on the other day. Electrotherapy was used on the same day of the participant's personal exercise. For electrotherapy, we used a device named Beurer EM 49 Digital TENS/EMS. The impulse was 250-µs duration, and the frequency was 25 to 50 Hz. We increased the time of each intervention to 2-3 minutes every 2 weeks whenever the participant was ready and reported no pain or inconvenience after each first session of increased time and pressure.
4. Discussion
This case study aimed to manage postoperative complications in a patient with excessive ankle stiffness, addressing balance and muscle strength, pain, quality of life, and ankle sagittal ROM. The patient progressed well through the phases of her rehabilitation and had favorable outcomes with regard to increased function and decreased pain during the balance task, muscle strength, and balance. The present results showed that the interventions could improve balance and ankle muscle strength and increase questionnaire scores.
4.1. FAAM, SF-36, ATRS, and FAOS
Questionnaires were re-assessed at the beginning of each phase of the protocol. Laboratory and clinical tests were done pre- and post-intervention. The subject was able to meet all of her protocol timelines and short-term protocol goals prior to advancing to the next phase. She demonstrated improved outcomes. Additionally, the subject reported no pain, tightness, or limitations on day 2 of her deployment.
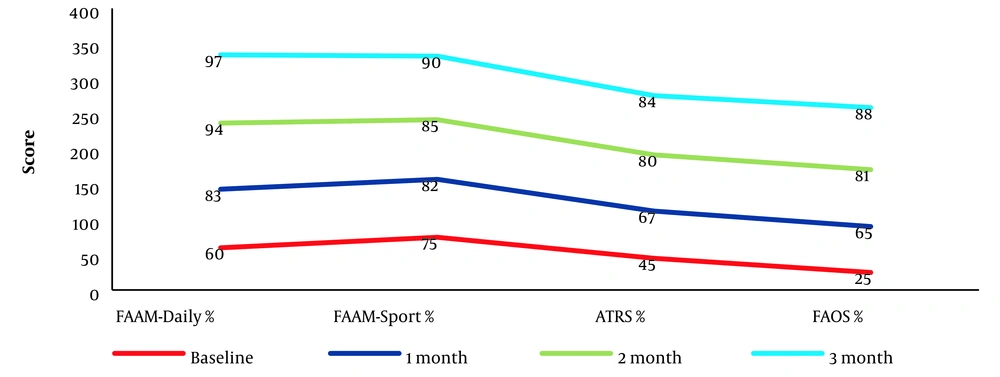
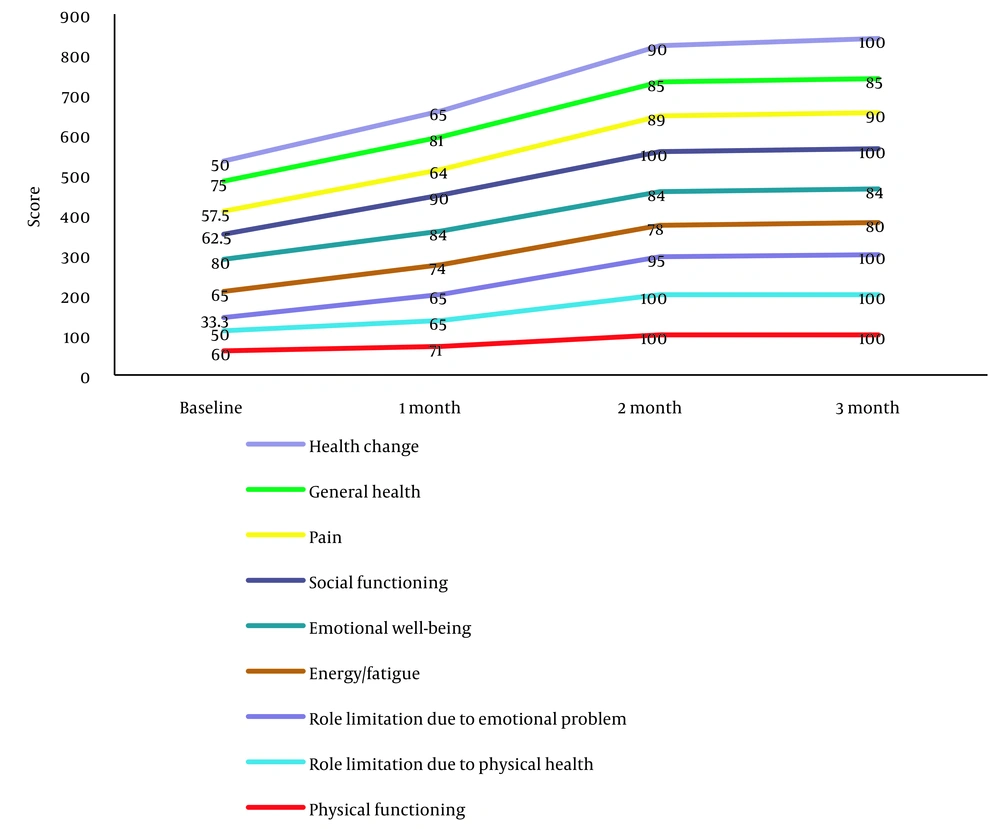
The scores of FAAM, ATRS, FAOS, and all domains of the SF-36 were improved after intervention (Figures 1 and 2). The primary objective of this intervention was to enhance mobility and function in patients with musculoskeletal injuries, and the observed improvements align with previous research, indicating the potential benefits of IASTM and electrotherapy on these measures. This is thought to be due to the improvements in balance and muscle strength. Both interventions can help reduce pain and inflammation, improve circulation, and enhance tissue healing. Additionally, IASTM can break down scar tissue and adhesions, while electrotherapy can facilitate muscle activation.
Consistent with the present study, previous studies have demonstrated that IASTM improved ROM in a collegiate football player following 7 weeks of IASTM and physical therapy (23). In another study, the quality of life increased after a 1-year follow-up of postoperative rehabilitation in a patient with a trimalleolar ankle fracture (24). Schaefer and Sandray reported that IASTM increased FAAM, FAAM Sport, and ROM in ankle instability patients (25). However, the findings of some studies suggest that these interventions may not lead to significant improvements in all cases. Other researchers have noted that optimal treatment protocols may vary depending on the specific injury and patient characteristics.
4.2. Balance
The stability index increased. Path length decreased by 35.5%, and path area decreased by 90% (Table 1). Given the patient's history of decreased ROM and muscle strength, these measurements allowed us to quantify the specific changes in balance control, providing a comprehensive picture of the patient's functional status. This information is essential for evaluating the impact of interventions on weight distribution and postural stability.
| Variables | Static | Dynamic | ||
|---|---|---|---|---|
| Biodex | Pre | Post | Pre | Post |
| Overall stability index | 3.5 | 4.3 | 1.4 | 1.8 |
| Anterior-Posterior stability index | 2.1 | 3.1 | 0.7 | 1.4 |
| Medial-Lateral stability index | 2.4 | 3 | 1.1 | 1.2 |
| Foot pressure | Pre | Post | ||
| Path Length mm | 398.73 | 287.93 | ||
| Area mm.mm | 159.13 | 83.63 | ||
Results of Stability Measurements
Static and dynamic balance scores increased, and path length and area decreased in the patient. Patients with musculoskeletal disorders often experience decreased stability due to reduced normal ROM and muscle strength. To assess the potential for increased balance and stability, we specifically aimed to measure both static and dynamic stability in our study. IASTM has been shown to increase joint ROM, and electrotherapy improves muscle activity and strength, indirectly influencing balance. Nakagawa and Petersen suggested that the reduction of the ROM of ankle joints caused a change in the compensatory movements of the hip joint and trunk movement by restricting balance and functional ability (26). The talocrural joint, which has a normal dorsiflexion ROM of 20° and 30° to 50° of plantar flexion (27), is closely related to postural control and functional capacity (28) and correlates with balance ability (29). Moreover, gastrocnemius muscles play a key role in maintaining balance, with the tibialis anterior muscle being stimulated during sway toward the anterior direction of the body (30). Our findings are consistent with earlier observations, showing that IASTM improves anterior reach in postural stability (31) and static balance (32), and electrotherapy results in greater balance, especially during the eyes-closed condition (33). Exercise with electrotherapy promotes the activation of the network that mediates proprioception and balance, may reduce spasticity, gait, and functional activity (34), and may decrease postural sway in the elderly (35).
4.3. Ankle Isokinetic Measurement
Isokinetic outcomes for both plantarflexion and dorsiflexion concentric/eccentric (con/ecc) and ecc/con are presented in Table 2. Peak torque/body weight increased by 24.3% and 27.3% and 31% and 150% for plantar flexors and dorsiflexors con/ecc and ecc/con, respectively. Total work increased by 76% and 27.3% and 9% and 30.7% for plantar flexors and dorsiflexors con/ecc and ecc/con, respectively. ROM increased by 79% and 55.5% for con/ecc and ecc/con, respectively.
| Variables | 180°/s | |||
|---|---|---|---|---|
| Plantarflexion | Dorsiflexion | |||
| Baseline | Post | Baseline | Post | |
| CON/ECC | ||||
| Peak Torque N-M | 27.4 | 34.1 | 35.9 | 45.7 |
| Peak TQ/BW % | 46.4 | 57.7 | 60.8 | 77.4 |
| Total Work J | 42.4 | 74.4 | 45.6 | 99.2 |
| ROM | 16.3 | 29.2 | ||
| ECC/CON | ||||
| Peak Torque N-M | 18.5 | 24.2 | 9.8 | 24.4 |
| Peak TQ/BW % | 31.3 | 41 | 16.6 | 41.4 |
| Total Work J | 16.6 | 18.1 | 12.4 | 17.2 |
| ROM | 15.5 | 24.1 | ||
Results of Ankle Isokinetic Tests
IASTM and electrotherapy increased dorsiflexion and plantarflexion peak torque, total work, and ROM after the 12-week intervention. By increasing ROM, the muscle will be at its optimum length to produce maximum torque in the patient with excessive ankle stiffness. Our results are consistent with previous findings, indicating that IASTM increases isokinetic muscle strength (36). Combining IASTM and electrotherapy can lead to greater improvements in outcomes. The evidence suggests that both IASTM and electrotherapy can lead to improvements in dorsiflexion and plantarflexion outcomes; by combining these treatments, clinicians may be able to achieve even greater improvements in these outcomes. Also, Kim et al. (12) investigated the effects of combining IASTM and electrotherapy on back pain and motor function, showing significant improvements after the combined treatment.
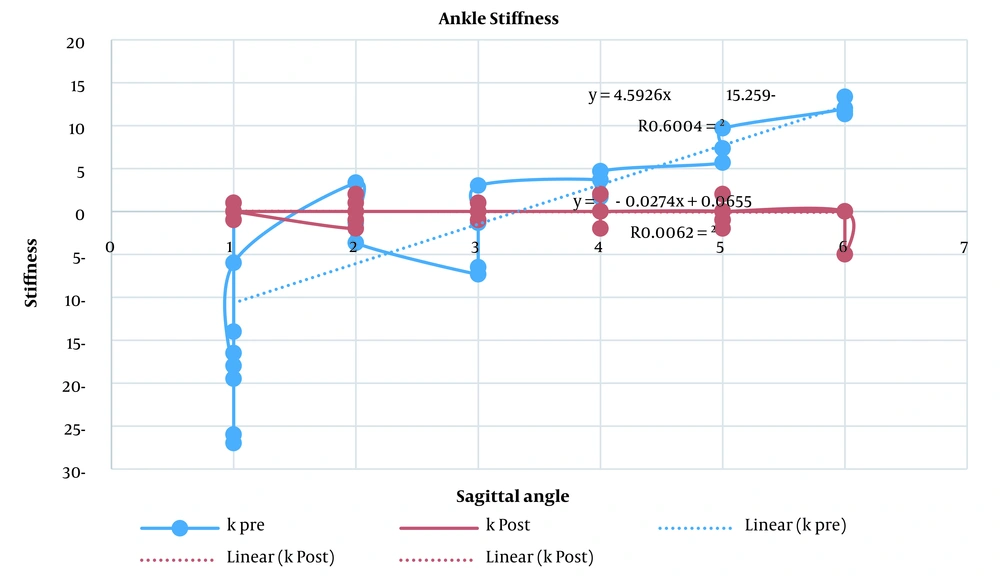
4.4. Ankle Passive Stiffness
Peak passive stiffness decreased by 273% after 12-week interventions (Figure 3). Our study found a great decrease in talocrural joint peak stiffness during passive dorsiflexion/plantarflexion due to the 80% increase in ankle sagittal plane ROM. These results further support the idea of Kim et al. (36), reporting that IASTM is the best soft tissue mobilization technique to reduce passive joint stiffness in individuals with hamstring shortness. A study conducted by Ikeda et al. (37) investigated the effect of IASTM on musculoskeletal properties. Their results showed that the dorsiflexion ROM significantly increased, and ankle joint stiffness significantly decreased. However, peak passive torque and muscle stiffness did not change.
In addition, Achilles tendon stiffness has been strongly correlated with ankle dorsiflexion stiffness (38), possibly due to the fact that the Achilles tendon is the largest tendon in the human body (39); therefore, the largest tendon offering resistance during ankle dorsiflexion. In this regard, IASTM was performed on the shank, Achilles tendon, and sole of the foot. While limited passive dorsiflexion ROM may alter ankle kinematics or potentially increase plantar-flexor muscle-tendon unit (MTU) strain during weight-bearing tasks, high or low dorsiflexion stiffness can impact injury potential by different mechanisms. Such stiffness can affect the MTU's overall joint stiffness and, therefore, influence its function and injury risk by influencing the stiffness of adjacent structures, like muscles, fascia, or tendons. Measures of passive joint stiffness can provide insight into the ability of the passive structures of the MTU to resist stretch or deformation under a tensile load. Joint stiffness may affect MTU strain-type injury potential by allowing the MTU to either strain too far under a given load or by protecting some passive structures within an MTU at the expense of transferring load more readily to others (19). Low joint stiffness may result in the deformation of some passive structures to injurious lengths, while high joint stiffness may not absorb sufficient strain energy via the Achilles tendon to prevent other structures, such as the muscle fibers, from incurring excessive and injurious strains (40).
4.5. Conclusions
This case study demonstrated that a 12-week program consisting of IASTM and electrotherapy can have a positive impact on balance, muscle strength, torque, ROM, and quality of life in a patient with Achilles tendon contracture. The combination of these 2 interventions improved static and dynamic balance and muscle strength in the affected leg. These findings have important implications for physical therapists and other health care providers, as they suggest that this combination of interventions may be an effective treatment approach for patients with similar conditions. However, further research is necessary to confirm these findings and determine the optimal duration and intensity of treatment required to achieve these results.
Limitations of this case study include reporting on only 1 fit female patient with 30 years of regular exercise history, which may limit external validity. Inactive or overweight patients may have different outcomes. It is unclear whether IASTM or electrotherapy alone can lead to outcome improvements. Also, measuring asymmetries between sides is important to study injury-induced changes. Unilateral chronic ankle injury affects the kinematic parameters of the uninjured ankle and leads to morbidity on the contralateral side. Therefore, rehabilitation protocols should be planned on both sides. Non-weight-bearing dorsiflexion stiffness measures ankle flexibility differently than weight-bearing and may have different implications for injury potential. Future studies should measure stiffness during gait and jumping. Moreover, the participant could only perform the isokinetic test in 180 °/s. Thus, aerobic exercise should be added to the future plan.