1. Background
Cerebral palsy (CP) is a nonprogressive disorder affecting the development of movement and posture, leading to activity limitations in the activity in the developing fetus or infant (1). The prevalence of CP is approximately 2 to 2.5 per 1000 live births (2). Cerebral palsy is classified based on muscle tone and the type of movement disorder, which results from brain damage, into spastic (60 - 70%), dyskinetic or athetoid (20 - 30%) and ataxic (5 - 10%) forms (3). Additionally, it is categorized by the affected body regions as hemiplegia, diplegia and quadriplegia (2).
Spasticity is a common outcome of CP (4), leading to delayed postural muscle activity in affected children compared to their typically developing peers. This impairment also includes issues with muscle sequencing and increased co-activation of agonist and antagonist muscles at a joint, reducing balance (1). Balance disorders pose significant challenges for children with spastic diplegic cerebral palsy (SDCP), causing difficulties in gaining and maintaining stability (5), transferring, daily life activities, participation and increasing the likelihood of falls (3).
Children with CP have abnormal muscle tone and postural control (6), directly affecting their functional balance (7). Due to the numerous issues associated with reduced balance control, providing an effective rehabilitation program is essential for developing the child’s mobility skills and preventing non-use sequelae, such as bone deformities, contractures, and obesity (8). Research shows that common interventions in rehabilitating children with CP help improve their balance (9). Based on a systematic review of the evidence for all interventions in CP by Novak et al. (as cited by Merino-Andres), physical training has demonstrated positive effects on muscle strength, aerobic capacity, and energy expenditure thereby reducing a sedentary lifestyle (10). Physical training focuses on balance components such as muscle tone, range of motion, muscle strength, and neuromuscular integration (11).
Selected exercises from the National Academy of Sports Medicine (NASM) approach include four stages: Myofascial inhibition, lengthening, activation and integration (12). This exercise protocol is comprehensive and covers all balance components. Myofascial inhibition inhibits hyperactive muscle fibers and reduces spasms. The second phase, lengthening, aims to increase muscle length and range of motion. The third phase, activation, strengthens weak and underactive muscles. The fourth phase, integration, aims to improve the functional capacity of the human movement system by increasing neuromuscular control in multi-planes (12). Neuromuscular control is directly related to balance (13).
2. Objectives
According to the systematic process that NASM exercises follow and the indicators they consider, the present study aims to investigate the effect of eight weeks of NASM exercises and compare them with usual and common therapeutic interventions on the functional balance of children with SDCP.
3. Methods
3.1. Subjects
The study involved 38 children (21 boys and 17 girls) aged 4 to 10 years with SDCP aged 4 to 10 years. Participants were selected from three occupational therapy clinics in Tehran and Karaj (Tavanyab, Hasti, and Tanin). Inclusion criteria required the absence of fixed lower limb deformities (e.g., bow legs or knock knees), no acute hearing or vision problems (issues correctable with aids were acceptable), no surgeries in the last six months, and no active seizures during the same period. Participants were randomly assigned into an intervention group (n = 19) and a control group (n = 19). The experimental group's mean age was 7.65 ± 2.10 years, while the control group's mean age was 6.44 ± 1.82 years. The study procedures were explained to parents, and written informed consent was obtained.
3.2. Apparatus and Task
3.2.1. Modified Ashworth Scale
The Modified Ashworth Scale (MAS) is the most widely used scale for manually grading spasticity (14). Ansari et al. (15) confirmed its reliability in Persian with intra-examiner and inter-examiner reliability. Spasticity is assessed through passive movement of both lower limbs while the child is supine, with the head in the midline. The test is repeated thrice, and the average score is recorded (7). The MAS scoring is as follows (16):
0 = Normal muscle tone.
1 = Slight increase in muscle tone, manifested as a catch and release, with minimal resistance at the end of the range of motion during flexion and extension.
+1 = Brief increase in muscle tone, manifested as a cramp followed by brief resistance, through less than half of the range of motion.
2 = Increased muscle tone, observed through most of the range of motion, but joint movement remains easy.
3 = Significant increase in muscle tone making passive movement is difficult.
4 = joint stiffness and rigidity prevent a complete passive range of motion.
3.2.2. SPARCLE Test
This test assesses intelligence level using a form completed by families based on the SPARCLE project’s injury form. IQ is expressed according to ICD -10, where an IQ of 50 to 70 indicates a mild learning disorder, and below 50 indicates a severe learning disorder (17, 18).
3.2.3. Pediatric Balance Scale
The Pediatric Balance Scale (PBS) is a valid assessment tool for evaluating children's balance. Its validity and reliability were confirmed by Franjoine et al. (19). Its reliability in Persian was also confirmed, with high inter-examiner (ICC = 0.985, P < 0.001) and intra-examiner (ICC = 0.994, P < 0.001) reliability (20). The PBS includes 14 items across 5 levels, assessing activities a child should perform safely and independently at home, school, and in the community. Scoring ranges from 0 to 4, with zero indicating inability and 4 indicating complete independence (7).
3.3. Procedure
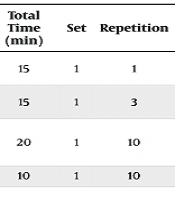
Before implementing the interventions, the PBS was used to evaluate both control and experimental groups. The interventions lasted eight weeks, with two weekly sessions of 60 minutes each. At the end of the study, the PBS was evaluated again. The experimental group received selected exercises based on the NASM approach in four stages: Inhibition, lengthening, activation, and integration. All four stages were performed on the child in each session (12) (Table 1).
| Stages | Exercise/Muscle Group | Total Time (min) | Set | Repetition | Duration of Each Repetition |
|---|---|---|---|---|---|
| Inhibition | Hip flexor, hip adductor, hip internal rotator, knee flexor, ankle plantar flexor | 15 | 1 | 1 | Apply pressure for 90 seconds to each muscle group. |
| Increase in length | Static stretching exercises; hip flexor, hip adductor, hip internal rotator, knee flexor, ankle plantar flexor | 15 | 1 | 3 | Thirty seconds |
| Activation | Isolated strengthening exercises; hip flexor, hip extensor, hip adductor, hip abductor, hip internal rotator, hip external rotator, knee flexor, knee extensor, ankle plantarflexor, ankle dorsiflexor | 20 | 1 | 10 | Two seconds of maintaining the isometric contraction at the end of the range of motion and 4 seconds of maintaining the eccentric contraction |
| Integration | Squats with a wall ball, jumping with both feet forward, step ups | 10 | 1 | 10 | - |
The control group received common rehabilitation interventions, including neurodevelopmental treatment (NDT) focusing on techniques to improve postural control and balance.
3.4. Data Analysis
Intra group changes were accessed using a dependent t-test, and one-way ANCOVA was used to compare groups. All statistical analysis were performed using SPSS version 24, with a significance level of P ≤ 0.05.
4. Results
The results show that there is no significant difference between the ages of the research groups in the pre-test (P > 0.05). The results of the ANCOVA indicated that after controlling for the effect of the pre-test, there is no statistically significant difference between the adjusted mean of the functional balance of the intervention and control groups (Tables 2 and 3).
| Variable | Pre-test | Post-test | Adjusted Post-test | Δ% |
|---|---|---|---|---|
| Functional balance | ||||
| Common intervention | 27.7 ± 4.43 | 31.84 ± 4.29 | 36.19 ± 1.25 | 4.105 ± 1.420 |
| NASM exercises | 37.05 ± 4.02 | 42.42 ± 3.99 | 38.06 ± 1.25 | 5.368 ± 1.05 |
Abbreviation: NASM, National Academy of Sports Medicine.
a Data are expressed as mean ± SE.
| Sources | Sum of Squares | df | Mean Square | F | P-Value | Effect Size |
|---|---|---|---|---|---|---|
| Functional balance | ||||||
| Pre-test | 10739.138 | 1 | 10739.138 | 369.943 | 0.000 | 0.914 |
| Group | 31.141 | 1 | 31.141 | 1.073 | 0.307 | 0.030 |
| Error | 1016.020 | 35 | 29.029 | |||
| Total | 65211.000 | 38 |
The results of the dependent t-test showed that the mean functional balance in the both groups increased significantly from pre-test to post-test (Table 4).
| Groups | Pairwise | Differences | df | t | P-Value | ||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Standard | 95% CI Minimum | 95% CI Maximum | ||||
| Common intervention | |||||||
| Pre-test\post-test | -4.10526 ± 6.19045 | 1.42019 | -7.08896 | -1.12156 | -2.891 | 18 | 0.010 |
| NASM exercises | |||||||
| Pre-test\post-test | -5.36842 ± 4.58513 | 1.05190 | -7.57838 | -3.15846 | -5.104 | 18 | 0.000 |
Abbreviation: NASM, National Academy of Sports Medicine.
5. Discussion
The NASM training protocol is comprehensive, incorporating muscle restraint techniques, stretching exercises, strengthening exercises, and neuromuscular exercises. The aim of the present study was to investigate the effect of eight weeks of NASM exercises and compare them with common therapeutic interventions on the functional balance of children with SDCP. Our findings showed that NASM exercises have a greater effect on improving functional balance in children with SDCP compared to common interventions.
Applying slow, steady pressure stimulates mechanoreceptors, which send information to the central and autonomic nervous systems. The central nervous system responds by altering skeletal muscle tone (reducing excessive tension), while the autonomic nervous system adjusts overall muscle tone, improves fluid dynamics (to reduce adhesions), and regulates the tone of smooth muscle cells in the fascia (12). Static stretching mechanically affects the viscoelastic components of neuromyofascial tissue (21), increasing muscle and connective tissue elasticity (lengthening) and joint range of motion (12). Enhancing lower extremity muscle strength positively impacts functional activities and flexibility (1). Dynamic coordinated movement improves the functional capacity of the human movement system by increasing multiplane neuromuscular control, achieved through exercises that involve the cooperation of the body’s stabilizing and moving muscles (12). Together, these factors contribute to improved balance, as demonstrated in our study, which found that NASM exercises are more effective in enhancing balance.
The findings of this research align with the studies by of Szturm et al. (8), who found that game-based exercises are more effective than common interventions for improving balance in children with CP. The results are consistent with those of Merino-Andres et al. (10), and Cho and Lee (1). Merino-Andres et al. found that a strength training program positively affects muscle strength, balance, gait speed, and gross motor function without increasing spasticity in children and adolescents with CP (10). Cho and Lee’s study suggests that functional progressive resistance exercise is feasible and beneficial for improving muscle tone, dynamic balance, and functional ability in children with CP (1).
Biomechanical changes in children with CP, such as hip and knee flexion, additional axial rotation of the tibia, plantar flexion in the ankle, and central nervous system defects like spasticity, cause balance control disorders (22). Research suggests that muscle weakness is prevalent in children with CP, with the affected limbs being significantly weaker and even the unaffected sides demonstrating reduced strength compared to typically developing children. Reduced muscle strength is positively correlated with functional limitations. Enhancing muscle strength in individuals with CP has been shown to improve walking ability (23). Physical therapy exercises reduce spasticity in flexor muscles and stretch extensor muscles, enhancing the child's balance maintenance ability (24). Strengthening the trunk, hip, and ankle muscles through exercise therapy reduces excessive fluctuations and improves balance (24). Another study found that increasing ankle muscle control improves balance in children with CP (22). Recent studies show that muscle tone, range of motion, and strength directly influence functional balance (7), and neuro-muscular control is directly related to balance (13).
Selected exercises from the NASM approach target movement components affecting balance and have improved balance. These exercises reduce muscle tone (first stage: Myofascial inhibition), increase range of motion (second stage: Lengthening), increase muscle strength (third stage: Activation), and enhance neuromuscular control (fourth stage: Integration), improving balance and posture control in children with SDCP.
However, the findings of the present research contrast with studies by Mirakhori et al. (22) and Borges et al. (25). Mirakhori et al. reported significant balance improvements in girls with hemiplegic CP through virtual reality training using Xbox (22). Borges et al. studied 40 children with CP using a horse riding simulator, reporting significant balance improvement in favor of intervention group (25). In these studies, a substantial difference was observed between the intervention and control groups. However, in the present study, no significant difference was found. This discrepancy may be attributed to the tools used for measuring balance and the engaging, game-like nature of Xbox-based interventions and horse-riding simulators.
It is suggested that when working with children with CP, the intervention should be engaging and playful, aligning with their interests and play environment. A limitation of the research was the lack of gym equipment in occupational therapy clinics for the strengthening exercises related to the activation phase of NASM exercises, which were instead performed using weight cuffs.
Finally, the study highlights the effectiveness of the NASM training protocol in improving functional balance in children with SDCP compared to common therapeutic interventions. The NASM approach, which incorporates techniques like myofascial inhibition, stretching, strengthening, and neuromuscular integration, was found to significantly enhance muscle tone regulation, range of motion, strength, and neuromuscular control. These improvements positively influenced balance and posture control. While both NASM exercises and traditional interventions increased functional balance, NASM showed a larger effect size, underscoring its superiority. The study suggests integrating playful and engaging elements into interventions to sustain children’s interest. A limitation was the lack of gym equipment for certain exercises, which were adapted using weight cuffs. Despite this, NASM exercises proved to be a highly effective approach for enhancing balance in children with SDCP.