1. Background
Cardiovascular diseases, with 17 million deaths per year, have been known as the leading cause of death in the world (1). Cardiovascular diseases include diseases affecting the blood supply to the heart, brain and peripheral areas of the body. It has been reported that these diseases are the first cause of death in Iran accounting for 40% of deaths (2), and the most important cause of death in Kerman province (accounting for 32.9% of all deaths) (3).
An important challenge in the treatment of cardiovascular disease is following treatment plans and prescribed medications (4). Most of the patients with chronic diseases abandon or ignore the recommended treatment regimen because they are either tired of long-term treatment or frustrated with the definitive treatment (5). Non-adherence to a treatment regimen is defined as “the degree of mismatch between individuals’ behavior and health or treatment recommendations”. Several factors such as patients’ personal characteristics, physician-patient relationship, and health care system affect adherence to the treatment regimen (6). Medication non-adherence rate has been reported to be 30 - 76% in different studies (7, 8). Numerous barriers such as prolonged drug use, inability to buy drugs and side effects of drug use have been reported as the most important factors of non-adherence to a drug regimen (9).
Non-adherence to treatment plans may lead to serious consequences, including recurrence and disability progression, need to immediate treatment and hospitalization (4) limits the effectiveness of preventive strategies, and leading to associated cardiovascular complications (7).
Drug use behavior is highly complex and personal (10). Individuals interpret information based on their own beliefs, and such experience ultimately influence their behavior (11). Therefore, the consequences of health behavior (e.g., drug use) result from rational decisions based on all available information. The Health Belief Model (HBM) is one of the first theories to be developed for health-related behaviors. According to this model, the likelihood that an individual will participate in a recommended health practice is essentially based on individual perceptions (12). Various studies have investigated the predictive role of the dimensions of the HBM on medication adherence (13-16).
Results of the study entitled “Self-care training based on HBM via Telegram”, showed that training via sending messages on Telegram significantly improved all constructs of HBM in diabetic patients (17). Also, education based on HBM improved medication adherence in hypertensive patients (18) and diabetic patients (19). However, the results of one study showed that the intervention based on the HBM had no effect on medication adherence in patients with diabetes, chronic kidney disease and systolic hypertension (20).
Given the evidence of adverse adherence of cardiovascular patients to the prescribed medication regimen and the role of education based on the HBM on adherence to the treatment regimen on the one hand and the contradictory results of some other studies (18), on the other hand, the question arises “Can HBM-Based education improve medication adherence in cardiovascular patients?”.
2. Objectives
Therefore, this study was conducted to investigate the effect of HBM-based education medication adherence of cardiovascular patients.
3. Methods
This quasi-experimental study conducted from March 20, 2020 to August 22, 2020 after receiving code of ethics.
3.1. Participants
The samples consisted of 45 patients with cardiovascular diseases discharged from the critical care unit (CCU) of Ali Ibn Abitalib Hospital in Rafsanjan, in Southeast of Iran. To determine the sample size, we used the formula for comparison of two independent groups’ means. Considering the confidence level of 95%, the test power of 80% and mean and standard deviation of performance reported by Ramanath et al. (21), the sample size was calculated to be 22 patients for each group. With regards to the survey dropout, finally, 25 participants were selected for each group.
In this study, after explaining the objectives of the research to the participants, patients who met the inclusion criteria were selected by adopting a convenience sampling method and after completing the written consent form, the patients were assigned into two groups of intervention (receiving education) and control (without intervention) by simple randomization. For this purpose, as many as 50 cards in two colors were placed in a box and each patient selected one of these cards from the box; he/she was then assigned to one of the groups.
Inclusion criteria were as follows: being over 40 years, being able to read and write, suffering from one of the cardiovascular diseases such as atrial fibrillation, myocardial infarction, congestive heart failure, hypertension and acute coronary syndrome, the confirmation of cardiovascular disease by a cardiologist, not participating in an earlier/simultaneous similar educational intervention, having access to a smartphone and the ability to work with WhatsApp Messenger. The patients were excluded from the study if they did not wish to continue participating in the study or if they did not participate in online interviews for more than a week, or if they were admitted to a hospital, or if they underwent any acute change in their disease status.
3.2. Tools
To collect data, demographic characteristics questionnaire (age, gender, duration of suffering from cardiovascular disease, BMI and type of cardiovascular disease), Morisky’s 8-item Medication Adherence Scale and researcher-made questionnaire based on HBM constructs were used. Morisky’s 8-item Medication Adherence Scale was used to assess the patients’ performance on medication adherence. This scale has seven two-point options (yes = 0, no = 1) and a five-point option (never = 1, rarely = 0.75, sometimes = 0.5, often = 0.25 always = 0.00). Each response of medication adherence received a score of 1 and each response of medication non-adherence received a score of zero. To measure the total score of the questionnaire, the scores of all items of the questionnaire were added. The overall score range was between zero and eight. Score of less than 6 was considered as poor medication adherence, from 6 to < 8 as moderate adherence and equal to 8 as good adherence.
Morisky et al. have reported the questionnaire’s Cronbach’s alpha to be 83% (22). In the study conducted by Moharamzad et al. in hypertensive patients, Cronbach’s alpha coefficient of Morisky questionnaire was reported as 0.679 (23). In the present study, this questionnaire has acceptable internal consistency with overall Cronbach’s alpha coefficient as 0.726.
Another research tool of this study was researcher-made questionnaire based on the constructs of the HBM. The items of questionnaire were designed based on reviewing the existing texts. The questionnaire consisted of five subscales as follow: Perceived sensitivity, perceived severity, perceived benefits, perceived self-efficacy and perceived barriers. In order to confirm the scientific reliability and calculate the content validity ratio (CVR) and content validity index (CVI), the questionnaire was provided to ten experts in this field. In total, as many as 6 questions had a content validity ratio index of less than 0.62 (based on Lawshe table) and a content validity index of less than 0.79; these questions were omitted. The final questionnaire included 28 questions. Questions 1 - 4 are related to perceived sensitivity, 5 to 12 were perceived severity, 13 to 16 are related to perceived benefits, 17 to 24 are related to perceived self-efficacy, and questions 24 to 28 are related to perceived barriers. Scoring was based on a 5-point Likert scale from 1(strongly disagree) to 5(strongly agree). Scores of each dimension were calculated based on the total number of questions. Higher score indicates a better condition in each subscale.
To determine the reliability, the questionnaire was provided to ten eligible patients. Cronbach’s alpha coefficient for the whole questionnaire was 0.76 and in the subscales it was as follows: perceived sensitivity (0.77), perceived severity (0.69), perceived benefits (0.76), perceived self-efficacy (0.70), and perceived barriers (0.77).
Questionnaires were completed by all the participants with similar time intervals. Participants in the intervention and control groups completed the HBM questionnaire before and three months after the intervention. While the Morisky’s 8-item Medication Adherence Scale was completed three times as follows: before intervention, one month after the intervention and three months after the intervention.
In the intervention group, the researchers made a list of the cell phone numbers of all the patients and joined them on a WhatsApp group. In addition to patients, all members of the research team were present in the groups. Before starting the education, the questionnaires were designed in “Google Drive” and its link was provided to the patients through WhatsApp group. The required instructions on how to complete the questionnaires were provided on the group and it was emphasized that they complete the questionnaires on time. The patients who had difficulty accessing the link and completing the questionnaire were instructed and guided via telephone. After completing the questionnaires, the educational course for the intervention group started. The educational content was developed in order to promote medication adherence based on the constructs of the HBM in the form of 5 educational topics. The educational content includes: (a) perceived sensitivity (explaining the likelihood of negative consequences and the risks of medication non-adherence), (b) perceived severity (explaining serious negative consequences in the client’s eyes and mentioning some objective examples), (c) perceived benefits (trust in the benefits of the proposed methods for reducing the risk or worsening of the disease, the relative effectiveness of the known options available, determining the behaviors to be performed, (d) perceived barriers (correcting one’s beliefs about actual and possible costs of a new behavior, difficulty, being painful and unpleasant, clearing up the possible misunderstandings, and providing incentives with successful examples), (e) cue to action (internal and external cues such as the media-physicians-family and friends) and (f) self-efficacy (reassuring the person that he or she has the ability to pursue a particular behavior). To do this, some steps are required to be taken, which include dividing complex behavior into small, practical and feasible steps, encouraging and reassuring, and reducing stress.
The time for presenting the educational materials was determined after coordination and agreement with all members of the group. Each session consisted of two parts: an offline part and an online one. The materials related to the offline sessions include video and PDF files were uploaded to the group every Monday at 9 pm. The participants were asked to send a message indicating they receive and study the educational content. Moreover, they were asked to write down their questions and experiences about the uploaded content in a notebook. On Thursdays, every week from 6 to 8 pm, the group would open and participants would share their experiences online and ask questions, and members of the research team would answer all their questions about the topics presented. During the intervention, members of the research team continuously checked the WhatsApp group and answered possible questions and gave necessary instructions to the patients. The patients of the intervention group were emphasized not to provide the group link to anyone and also to refrain from sharing the content before the end of the educational course.
No intervention was conducted in the control group and they received routine care during the study.
3.3. Ethical Approval
This study was approved with the permission of the Rafsanjan University of Medical Sciences Ethics Committee with the number (IR.RUMS.REC.1398.119). The study began after providing necessary permits to the chairman of Ali Ibn Abitaleb Hospital and the relevant authorities. First, patients who met the inclusion criteria were selected and participants signed an informed consent form. The questionnaires had no name or any identifying marks. Necessary explanations were provided to the participants about the aims and methods of the present study, and they were also assured that their information would remain confidential and that they could leave the study at any time. The educational materials (PDF files and audio files) given to the control group at the end of the study in order to comply with ethical principles.
Data analysis was conducted using SPSS V-23. We used descriptive statistics such as frequency and, mean ± standard deviation for the qualitative and quantitative variables respectively. To compare individual characteristics in the two group’s independent t-test, chi-squared test and Fisher’s Exact Test were used. The data from the Morisky’s Medication Adherence scale, were analyzed by repeated measures analysis of variance. To conduct intra-group comparison in terms of dimensions of the HBM questionnaire, paired t-test was applied. Finally, to conduct inter-group comparison, independent t-test was used. The Kolmogorov-Smirnov test was used to test the normality of data distribution. Significance level in all tests was considered to be 0.05.
4. Results
In this study, as many as 45 patients with cardiovascular disease participated in two groups of control (22 patients) and intervention (23 patients). The results indicated that the two groups did not differ significantly in terms of age, marital status and income. The results of comparisons of other demographic characteristics are given in Table 1.
Based on the results of Kolmogorov-Smirnov test, scores of the Medication Scale as well as the various dimensions of the HBM questionnaire before and after the intervention had a normal distribution.
| Variables | Groups | P-Value | |
|---|---|---|---|
| Control | Education | ||
| Duration of disease | 38.5 ± 3 | 36.4 ± 3.3 | 0.823 |
| Age | 50.84 ± 8.55 | 50.34 ± 8.35 | 0.851 |
| Maritalstatus | 0.491 | ||
| Single | 2 (9) | 4 (17.4) | |
| Married | 20 (91) | 19 (82.6) | |
| Income | 0.783 | ||
| > 30 million Iranian Rial | 18 (81.81) | 17 (73.91) | |
| 30 - 50 million Iranian Rial | 4 (18.19) | 6 (26.08) | |
| Insurance coverage | 0.328 | ||
| Yes | 22 (100) | 22 (95.7) | |
| No | 0 (0.00) | 1 (4.3) | |
| Sex | 0.624 | ||
| Male | 18 (81.8) | 19 (82.6) | |
| Female | 4 (18.2) | 4 (17.4) | |
| Education | 0.53 | ||
| Less than diploma | 4 (18.2) | 5 (21.7) | |
| Diploma and higher | 18 (81.8) | 18 (78.3) | |
| Antiplatelet drugs use | 0.534 | ||
| Yes | 17 (77.3) | 17 (73.9) | |
| No | 5 (22.7) | 6 (26.1) | |
| Glucose-lowering medications | 0.334 | ||
| Yes | 10 (45.5) | 8 (34.8) | |
| No | 12 (54.5) | 15 (65.2) | |
| Antihyperlidemi a drug use | 0.104 | ||
| Yes | 14 (63.6) | 9 (39.1) | |
| No | 8 (36.4) | 14 (60.9) | |
Comparison of the Demographic Characteristics Between Education and Control Groups in Cardiovascular Patients a
The results of comparing the mean score of medication adherence in the two groups over time, indicated that there was a significant difference between the two groups three months after intervention (P = 0.001). There was no statistically significant difference between groups, before intervention and one month after the intervention. Also, the intra-group comparison showed that the mean score of medication adherence at different times in the education group, was different and significantly improved three months after the intervention (P = 0.006), while no difference was seen in the control group (P = 0.665) (Table 2).
| Group, Mean ± SD | P-Value | ||
|---|---|---|---|
| Education | Control | ||
| Time of Assessments | |||
| Baseline | 5.18 ± 0.39 | 5.15 ± 0.36 | 0.964 |
| One month after the intervention | 5.29 ± 0.28 | 5.15 ± 0.29 | 0.710 |
| Three months after intervention | 6.63 ± 0.26 | 5.29 ± 0.16 | 0.001 |
| F | F (1,22) = 9.127 | F (1,21) = 0.193 | |
| P-value | 0.006 | 0.665 | |
Comparison of Medication Adherence in Education and Control Groups in Cardiovascular Patients During the Study (Inter-group, Intra-group Comparison)
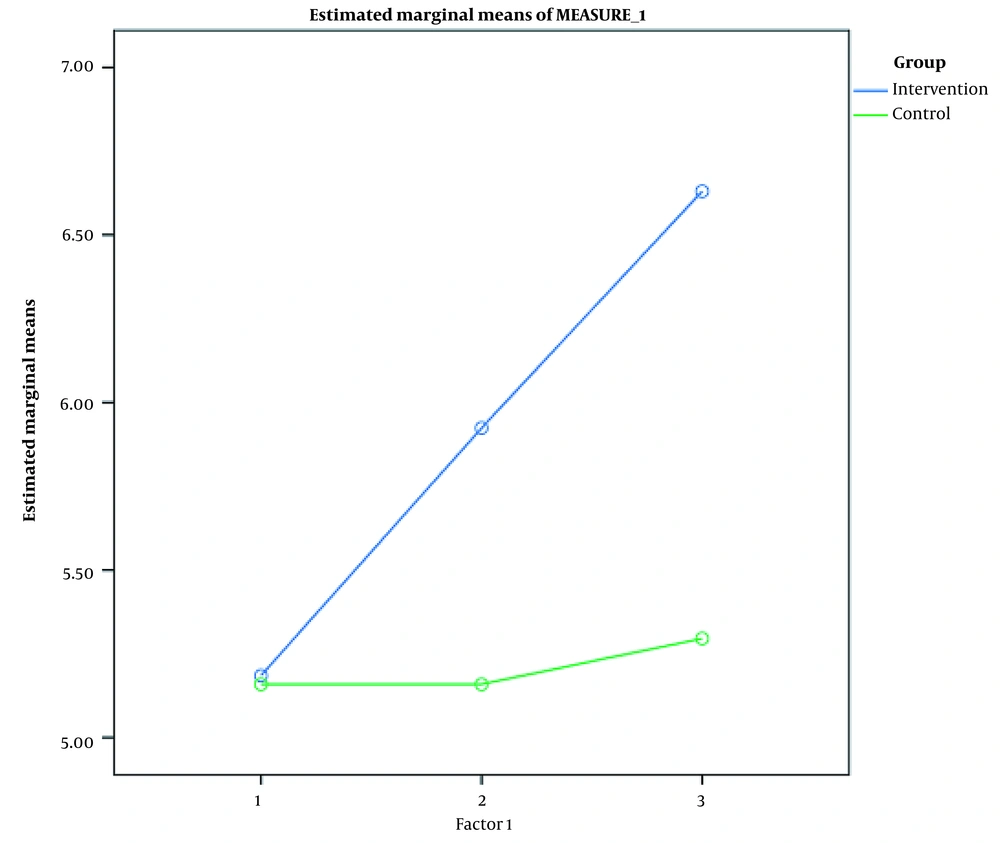
In order to compare the mean score of medication adherence in the two groups over time, two-way analysis of variance with repeated measures was used. The results of the interactive effect (interaction of group and time) indicated that there is a significant difference between the mean scores of the two groups over time (P = 0.049). Investigating the effect of group, indicated that there was a significant difference between the mean scores of medication adherence between the two groups (P = 0.042), while the mean scores of medication adherence over time also had a significant difference (the effect of time, P = 0.014) (Figure 1).
The results of independent t-test showed that the mean scores of the dimensions of the HBM including perceived sensitivity, perceived severity, perceived benefits and perceived barriers in the pre-education stage were not significantly different between the intervention and control groups (P > 0.05). Three months after the intervention, the mean score of perceived benefits (P = 0.023), perceived self-efficacy (P = 0.001) and perceived barriers (P = 0.014) was significantly different between the two groups and increased in the intervention group. In the intra-group comparison, the results of paired t-test showed that the mean score of all dimensions of the HBM increased significantly in the intervention group while they remained unchanged in the control group (Table 3).
| Health Belief Model Constructions | Groups, Mean ± SD | P-Value* | |
|---|---|---|---|
| Control | Education | ||
| Perceived susceptibility | |||
| Before the intervention | 14.31 ± 3.8 | 14.05 ± 1.36 | 0.747 |
| After the intervention | 14 ± 4.14 | 15.3 ± 4.81 | 0.337 |
| P-value** | 0.719 | 0.277 | |
| Perceived severity | |||
| Before the intervention | 28.68 ± 4.46 | 29.34 ± 2.22 | 0.568 |
| After the intervention | 30 ± 6.3 | 30 ± 7.19 | 0.080 |
| P-value** | 0.548 | 0.028 | |
| Perceived benefits | |||
| Before the intervention | 12.9 ± 1.41 | 12.78 ± 2.2 | 0.822 |
| After the intervention | 16 ± 2.94 | 18 ± 2.74 | 0.023 |
| P-value** | 0.00 | 0.001 | |
| Perceived self-efficacy | |||
| Before the intervention | 23.68 ± 5.32 | 24.04 ± 3.26 | 0.784 |
| After the intervention | 23.13 ± 5.36 | 29 ± 6.36 | 0.001 |
| P-value* | 0.200 | 0.000 | |
| Perceived barriers | |||
| Before the intervention | 11.13 ± 2.67 | 12.52 ± 1.92 | 0.054 |
| After the intervention | 10.36 ± 2.76 | 12.86 ± 3.72 | 0.014 |
| P-value* | 0.067 | 0.069 | |
5. Discussion
The results of the present study, which aimed to determine the effect of HBM-based education on medication adherence in cardiovascular patients, indicated that the medication adherence score, three months after the education, improved significantly in the intervention group. Perceived self-efficacy, perceived benefits, and perceived barriers three months after the education were significantly higher in the intervention group than that of the control group. The literature review showed that, there is a range of effects of education based on the HBM on medication adherence and some of the constructs of the model. A HBM-based educational intervention, including 8 one-hour training sessions, twice a week, significantly increased the medication adherence of the elderly with high blood pressure in the intervention group (18). The results of the study conducted in 2018, which is similar to the present study in terms of method and educational method used, indicated that self-care training based on the HBM via Telegram in diabetic patients, significantly promoted all constructs of HBM compared to the pre-intervention status. In their study, researchers provided Self-care training for one month using text message, podcast, video and info graphic (17). Also, a HBM-based education in diabetic patients increased the patient’s post-intervention performance in terms of medication adherence as well as perceived sensitivity, perceived benefits, self-efficacy and cue to action (internal and external) (19). The findings of the similar study have also indicated that HBM-based educational intervention significantly increased performance in the field of medication adherence in the intervention group and increased the mean score of all constructs of the HBM including perceived sensitivity, perceived intensity, perceived benefits, and perceived barriers (19). In another study on 72 Patients with AIDS, three educational sessions based on the expanded HBM, significantly improved the adherence to antiretroviral therapy and perceived severity. Other constructs of HBM remained unchanged (24).
These studies are consistent with our study in terms of changes in self-efficacy, perceived benefits, and perceived barriers constructs. On the other hand, results of these studies are not consistent with our findings in terms of perceived sensitivity and perceived severity (17, 19, 24). This difference can be attributed to issues such as the population studied, the tools used, the type and duration of the intervention.
Evidence suggests that drug-taking behavior is highly complex and personal (10), based on individuals beliefs (11). Therefore, health behaviors such as drug use result from rational decisions that are based on all available information (12). The positive effects of educational intervention on medication adherence can be explained through increasing the self-efficacy dimension, which directly affecting the behavior of drug use. Also improved perceived benefits and reduced perceived barriers affect the patients’ medication adherence. The relationship between the dimensions of the HBM and medication adherence has been emphasized. For example perceived benefits and perceived self-efficacy significantly predict adherence to the antihypertensive medication regimen (14). Also adherence to medication was higher in the elderly who had higher levels of perceived severity, perceived sensitivity, and perceived benefits (15). In a systematic review, 93% of the 29 articles surveyed mentioned perceived barriers as the strongest predictors of medication adherence (13). Higher levels of perceived sensitivity, perceived severity and perceived barriers were significantly associated with the degree of medication non-adherence in patients with hypertension. While higher levels of perceived benefits and cues to action were associated with higher medication adherence (16). In the study conducted on patients with hypertension in Indonesia, there was a statistically significant relationship between medication adherence and perceived sensitivity to the effects of hypertension and its severity, benefits of medication adherence and barriers to drug adherence (25). However, the results of the study on the effect of HBM-based intervention on medication adherence to antihypertensive drugs showed that intervention had no effect in 80 diabetic patients with renal complications (the intervention n = 39 and usual care n = 41). In their study, the education with a psychological and motivational approach were provided in the form of a 20-minute DVD, including the way hypertension affects one’s body, the necessity, benefits and safety of prescribed drugs, and important points to help patients’ medication adherence. Moreover, home care and telephone calls were provided for the patients with the aim of creating incentives for the use of drugs. Follow-up was done at intervals of 3, 6, and 9 months after the intervention (20). This finding is not in line with the results of the present study. In this study, the pill count method was used to measure drug adherence. The authors state that given the changes in the type and dose of drugs used during the study, the drug adherence calculated on this basis was not reliable and this can be one of the reasons for having different results. Also, differences in the research sample, type of intervention and duration of follow-up can play a role in this difference.
In this study, medication adherence was measured by self-report method using a questionnaire; this can be regarded a limitation. Therefore, it is recommended that in future studies, a combination of several methods be used to evaluate medication adherence. Moreover, in this study, most of the patients were middle-aged and literate; the required caution must be taken in generalizing the results to adolescent and young patients or illiterate people. Given the importance of improving medication adherence in chronic diseases, it is suggested that other studies be conducted using new technologies on the Internet in different patients and different age groups.
In previous studies, the variables of age, duration of drug use, concomitant use of antiplatelet drug and duration of disease have been mentioned as determinants of medication adherence (16, 26). One of the strengths of the current study was that the two groups did not differ in terms of these variables, so the changes in the dependent variable can be attributed the effect of the educational intervention.
5.1. Conclusions
According to the results of the present study, it can be concluded that by implementing the HBM-based educational intervention, a significant difference was created on medication adherence of cardiovascular patients. Given the ability to implement, simplicity, and cost-free education based on the HBM in patients with cardiovascular disease, the use of this method has a positive and significant effect on increasing medication adherence and patient perception (perceived sensitivity, perceived severity, perceived benefits and perceived barriers). It can be thus concluded that it improves and promotes the health of cardiovascular patients. Thus, by using a HBM-based educational intervention the process of medication adherence of cardiovascular patients may be facilitated and the quality of their care may be improved as well.