1. Background
Nurses are the first point of contact in hospitals. The impact of nursing care on patient outcomes has been highlighted in a vast body of literature (1, 2). However, studies have shown that some aspects of nursing care are neglected (2, 3). Missed nursing care has been described as either an act of doing something wrong or an omission or delay in whole or in part (3, 4). Missed care has been identified to occur when nurses have to perform multiple tasks concurrently. It is proposed that inadequate staffing results in experiencing a shortage of time and, therefore, the absence of some nursing activities, leading to unfavorable patient outcomes (5). The increased nursing staffing and improved skills have been associated with lower mortality rates, fewer adverse events, and shorter stays in acute care hospitals (6-8).
It is interesting to note that high rates of missed nursing care are also associated with adverse outcomes for nurses, which may increase the intention to abandon and turnover and reduce job satisfaction (6). Literature reviews have revealed that missed nursing care is a global issue. However, missed care frequency and elements differ from country to country (4, 9). Studies conducted in Brazil and the United States have demonstrated that 14% - 69% of all medication errors were attributed to nursing care omissions (2, 10). In a study conducted in the United States, missed nursing care showed a prevalence of 10%-27% (11). Also, in a survey in 12 European countries, an average of 3.6 of 13 nursing tasks was undone (6). The reasons for this phenomenon can also differ based on the environment and resources of the country’s health systems (1). In a study in England, nursing care activities were reported to be frequently missed in general medical or surgical wards. The most prevalent omissions were “developing or updating nursing care plans” and “talking and comforting the patients” (12). Some studies from various nations have recorded the common nursing care omissions as follows: Emotional or psychological support, evaluation of newly admitted patients, documenting nursing care, assessing the efficacy of medications, turning patients, and mouth care (2, 7, 13).
During the COVID-19 pandemic, the number of patients cared for, patient/nurse ratio, days of nurses’ absence due to sick leave, nurses’ workload, and overtime work hours increased. The nursing staff was relocated, or new colleagues were added to the ward. The maintenance of personal hygiene, using protective gear, and contact restrictions changed the work environment and communication or interaction with patients or others. Also, psychological issues, such as stress, anxiety, depression, and emotional exhaustion, were enhanced (14-18). These conditions may affect omitting or postponing nursing activities or change its causes. A comparison study in Jordon revealed that missed nursing care significantly increased during the COVID‐19 pandemic (19), while research in Sweden showed that the extent of missed nursing care did not differ compared to the pre-pandemic sample (16). Thus, to manage the quality of care and prevent the recurrence of missed nursing care throughout these situations, identifying the extent of missed care and factors contributing to impairing nurses’ clinical performance is needed.
2. Objectives
This study aimed to investigate the prevalence of missed nursing care, its causes, and its relation with some factors (i.e., nurses’ occupational stress and demographic, staffing, and organizational characteristics) in non-emergency wards of adult medical centers during the COVID-19 pandemic in Rasht, Iran.
3. Methods
This cross-sectional study was approved by the Ethics Review Board of Guilan University of Medical Sciences (code: IR.GUMS.REC.1399.325). The data were collected from January to March 2021 in Rasht City during the COVID-19 pandemic. The number of confirmed new cases was 10 to 24 per 100 000 people, and the overall epidemic trend was increasing.
The study population included all nurses working in educational and medical centers in Rasht City. Inclusion criteria were working as a nurse in the non-emergency departments of adult hospitals and having at least a bachelor’s degree with 6-month work experience in the relevant department. Those working as nursing students or passing their internship and nurses who were unwilling to participate were excluded.
Based on the estimation of 44% of missed care reported in previous studies (10), considering a 95% CI and estimation error of 6% and 15% for compensating missing data, the required sample size was 326 nurses. Nurses were randomly selected from the list of nurses working in all 7 educational-medical centers (i.e., Razi, Poursina, Shafa, Alzahra, Heshmat, Velayat, and Amir-Al-Momenin) in Rasht City. A simple random sampling method with an online random number generator (https://www.random.org/integer-sets) was used. The number of nurses selected from each hospital was proportional to the number of hospital beds.
Standard questionnaires of missed nursing care (MISSCARE), expanded nursing stress scale (ENSS), and a questionnaire consisting of demographic, work schedules, and staffing information were used. To the best of our knowledge, the association between missed nursing care and specific nurses’ occupational stress has not been investigated in previous research.
The MISSCARE questionnaire was published in 2009 by Kalisch et al. (10). The first part of the questionnaire included 24 mandatory and routine nursing cares. Each nurse had to choose one of the Likert-type items from 1 to 5 as “never,” "infrequently," "sometimes," "often," and "always" for missing each nursing task regarding the frequency of missed care in their ward, either by ward staff or himself/herself. The second part included 17 common causes related to the reasons for missed care, with 4-choice Likert-type answers from 1 to 4 as "no cause for not doing it," "trivial cause," "moderate cause," and "major cause." The nurse should choose one of the options as to how much the reason mentioned was effective in not providing nursing care in the previous work shift (i.e., it expressed the importance of the mentioned reason). Higher summed scores indicate a more compelling reason. The Persian version of the questionnaire was approved by Chegini et al. (1). The validity of the questionnaire was confirmed by a panel of 9 nursing specialists (including 3 nursing faculty members, 2 head nurses, and 4 ward nurses) with a content validity index of 0.82 and a content validity ratio of 0.79. Also, to assess the reliability, the questionnaire was completed by 15 nurses, and Cronbach alpha coefficients were obtained at 0.85 and 0.73 for 2 parts of the questionnaire, respectively.
A standard questionnaire, ENSS, was used to measure occupational nursing stress (19). This questionnaire included 57 stressful situations in 9 subscales (death, conflict with physicians, inadequate emotional preparation, problems with colleagues and supervisors, workload, uncertainty about treatment, patients, families, and discrimination). According to the frequency of experience of the desired situation, participants choose one of the following options: “0 = this situation does not include me,” “1 = I have no stress at all,” “2 = sometimes I have stressed,” “3 = I am often stressed,” and “4 = I am very stressed.” Higher total scores state higher occupational stress. The internal consistency of the subscales was reported to be from 0.65 to 0.88, and the overall internal consistency of the instrument was reported to be 0.96 (19). The Persian version of the questionnaire has been used in research in Iran. The validity and reliability of the questionnaire have been confirmed in different studies (20, 21). In this study, to assess the instrument reliability, the questionnaire was completed by 15 clinical nurses twice, with a time interval of 2 weeks. The intra-cluster correlation coefficient of the test-retest was obtained as 0.87, and the Cronbach alpha coefficient was obtained as 0.97 and 0.95 in the 2 measurements, confirming the questionnaire’s reliability.
After obtaining the necessary permits, an envelope consisting of the questionnaire with explanations about the study objectives, confidentiality of the information, and the authority to participate in the survey was given to the selected participants after obtaining written informed consent. The nurses completed the questionnaires during their break time.
Frequency (percentage), median or mean (SD), and range or 95% CI were reported to describe the data. Simple and multiple logistic regressions were performed to explore the associated variables with missed care occurrence. Care was considered missed when it was reported that it was occasionally, frequently, and always missed. A stepwise backward likelihood ratio procedure controlling for hospital variables was used in multiple logistic regression. All tests were performed at a significant level of 0.05 using SPSS version 21 (SPSS Inc, Chicago, IL, USA).
4. Results
A total of 326 nurses were included in the study. The mean age was 37 years (SD, 8.5), and 95% were female. The demographic and work characteristics of the participants are shown in Table 1. The median number of hospital beds was 139 (range 52 - 273).
| Characteristic | No. of Participants (%) |
|---|---|
| Gender | |
| Female | 310 (95) |
| Male | 16 (5) |
| Age (y), mean ± SD (median, range) | 36.7 ± 8.5 (38, 22 - 58) |
| 20 - 29 | 88 (28) |
| 30 - 39 | 97 (30) |
| 40 - 49 | 111 (35) |
| 50 ≥ | 22 (7) |
| Education | |
| Bachelor’s degree | 290 (90) |
| Master’s degree | 32 (10) |
| Marital status | |
| Single | 100 (31) |
| Married | 222 (68) |
| Divorced/widowed | 2 (1) |
| Job position in the ward | |
| Nurse | 291 (89) |
| Head nurse | 35 (11) |
| Years of experience in the role, mean ± SD (median, range) | 12.2 ± 7.5 (13, < 1 - 41) |
| < 5 | 90 (28) |
| 5 – 15 | 123 (38) |
| > 15 | 108 (34) |
| Years of experience on the ward, mean ± SD (median, range) c | 6.8 ± 5.5 (5, < 1 - 26) |
| < 2 | 46 (15) |
| 2 – 5 | 117 (38) |
| > 5 | 147 (47) |
| Work shift | |
| Day | 73 (22) |
| Day and evening | 22 (7) |
| Night | 10 (3) |
| Rotating | 219 (68) |
| Number of shifts worked in the last month, mean ± SD (median, range)a | 21 ± 5.3 (22, 5 - 50) |
| Extra hours worked in the last month | |
| ≤ 30 hours | 156 (50) |
| > 30 hours | 157 (50) |
| Number of days/shifts absent in the past 2 months | |
| 0 | 219 (68) |
| 1 | 12 (4) |
| ≥2 | 90 (28) |
| Type of employment contract | |
| Fixed-term contract | 38 (12) |
| Permanent | 178 (56) |
| Candidate of permanent | 11 (4) |
| Temporary | 89 (28) |
| Type of ward | |
| Internal | 215 (66) |
| Surgical | 46 (14) |
| ICU | 63 (19) |
| Number of patients cared for, mean ± SD (median, range) c | 8.9 ± 7 (7, 1 - 35) |
| Nursing occupational stress, mean ± SD (median, range) | 1.6 ± 0.59 (1.6, 0 - 4) |
Regarding the missed care in each shift, 99 nurses (31%; 95% CI, 26 - 36) believed that all activities were never missed or rarely missed, while 221 (69%; 95% CI, 64 - 74) reported that at least 1 aspect of nursing care was occasionally, often, or frequently missed. The median number of care activities reported as missed on each shift was 4 out of 25 (95% CI for median, 2 - 4).
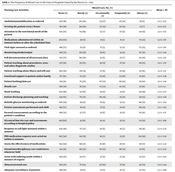
Frequency distributions of the type of care missed by nurses are shown in Table 2. All care activities are perceived to be missed occasionally and not often or frequently. Most nursing care activities, which were reported as frequently, often, or occasionally missed, were as follows: “attend interdisciplinary care conferences whenever held” reported by 151 (46%) of the nurses, “patient bathing/skincare” reported by 46%, “mouth care” reported by 45%, “emotional support to the patient and/or family” reported by 42%, and “turning the patient every 2 hours” reported by 43%.
| Nursing Care Activities | Missed Care, No. (%) | Mean ± SD | ||||
|---|---|---|---|---|---|---|
| Never (1) | Rarely (2) | Occasionally (3) | Frequently (4) | Always (5) | ||
| Ambulation/mobilization as ordered | 123 (38) | 84 (26) | 54 (17) | 47 (14) | 18 (6) | 2.2 ± 1.25 |
| Turning the patient every 2 hours | 90 (28) | 96 (29) | 75 (23) | 42 (13) | 23 (7) | 2.4 ± 1.22 |
| Attention to the nutritional needs of the patient | 154 (47) | 63 (19) | 22 (7) | 37 (11) | 50 (15) | 2.3 ± 1.52 |
| Medications administered within 30 minutes before or after the scheduled time | 202 (62) | 29 (9) | 11 (3) | 11 (3) | 73 (22) | 2.2 ± 1.67 |
| Vital signs assessed as ordered | 186 (57) | 35 (11) | 17 (5) | 13 (4) | 75 (23) | 2.3 ± 1.67 |
| Monitoring intake/output | 166 (51) | 60 (19) | 19 (6) | 12 (4) | 67 (21) | 2.2 ± 1.59 |
| Full documentation of all necessary data | 122 (37) | 99 (30) | 21 (6) | 22 (7) | 62 (19) | 2.4 ± 1.51 |
| Patient teaching about procedures, tests, and other diagnostic studies | 127 (39) | 83 (25) | 30 (9) | 37 (11) | 49 (15) | 2.4 ± 1.47 |
| Patient teaching about illness and self-care | 146 (45) | 69 (21) | 27 (8) | 31 (10) | 53 (16) | 2.3 ± 1.51 |
| Emotional support to patient and/or family | 117 (36) | 73 (22) | 52 (16) | 53 (16) | 31 (10) | 2.4 ± 1.36 |
| Patient bathing/skincare | 101 (31) | 75 (23) | 67 (21) | 50 (15) | 33 (10) | 2.5 ± 1.34 |
| Mouth care | 100 (31) | 78 (24) | 75 (23) | 42 (13) | 31 (10) | 2.5 ± 1.3 |
| Hand washing | 154 (48) | 52 (16) | 35 (11) | 21 (6) | 62 (19) | 2.3 ± 1.57 |
| Patient discharge planning and teaching | 131 (40) | 70 (21) | 46 (14) | 35 (11) | 44 (13) | 2.4 ± 1.44 |
| Bedside glucose monitoring as ordered | 190 (59) | 36 (11) | 18 (6) | 12 (4) | 68 (21) | 2.2 ± 1.63 |
| Patient assessments performed each shift | 185 (57) | 41 (13) | 17 (5) | 14 (4) | 69 (21) | 2.2 ± 1.63 |
| Focused reassessments according to the patient’s condition | 166 (51) | 57 (17) | 21 (6) | 21 (6) | 61 (19) | 2.2 ± 1.57 |
| IV/central line site care and assessments according to hospital policy | 193 (60) | 31 (10) | 14 (4) | 12 (4) | 74 (23) | 2.2 ± 1.68 |
| Response to call light initiated within 5 minutes | 154 (48) | 75 (23) | 18 (6) | 16 (5) | 58 (18) | 2.2 ± 1.52 |
| PRN medication requests were acted on within 15 minutes | 163 (50) | 60 (19) | 16 (5) | 21 (6) | 64 (20) | 2.3 ± 1.59 |
| Assess the effectiveness of medications | 142 (44) | 68 (21) | 31 (10) | 29 (9) | 56 (17) | 2.4 ± 1.52 |
| Attend interdisciplinary care conferences whenever held | 94 (29) | 80 (25) | 70 (22) | 46 (14) | 35 (11) | 2.5 ± 1.33 |
| Assist with toileting needs within 5 minutes of request | 161 (50) | 54 (17) | 27 (8) | 27 (8) | 55 (17) | 2.3 ± 1.54 |
| Skincare/wound care | 138 (43) | 75 (23) | 32 (10) | 37 (11) | 42 (13) | 2.3 ± 1.44 |
| Adequate surveillance of patients | 198 (61) | 28 (9) | 13 (4) | 10 (3) | 75 (23) | 2.2 ± 1.68 |
The Frequency of Missed Care in the Units of Hospitals Stated by the Nurses (n = 326)
On the other hand, activities such as “medications administered as ordered within the scheduled time,” “bedside glucose monitoring as ordered,” and “patient assessments performed each shift” were the most rarely missed item.
The most important reason for missed care was “human resources,” followed by “material resources” and “communication” (Table 3).
| Reason | Reason for Missed Care, No. (%) | Mean ± SD | |||
|---|---|---|---|---|---|
| Not a Reason (1) | Minor (2) | Moderate (3) | Significant (4) | ||
| Human resources - overall | 3.3 ± 0.64 | ||||
| Inadequate number of staff | 18 (6) | 10 (3) | 69 (21) | 229 (70) | 3.6 ± 0.80 |
| Urgent patient situations (e.g., a worsening condition) | 35 (11) | 33 (10) | 122 (38) | 134 (41) | 3.1 ± 0.97 |
| Unexpected rise in patient volume and/or acuity in the unit | 15 (5) | 20 (6) | 90 (28) | 201 (62) | 3.5 ± 0.81 |
| Inadequate number of assistive personnel (e.g., nursing assistants, techs, unit secretaries, etc.) | 16 (5) | 21 (6) | 95 (29) | 192 (59) | 3.4 ± 0.82 |
| Heavy admission and discharge activity | 21 (6) | 27 (8) | 115 (35) | 163 (50) | 3.3 ± 0.87 |
| Emotional or physical exhaustion | 16 (5) | 45 (14) | 104 (32) | 161 (49) | 3.3 ± 0.87 |
| Interruptions/multitasking | 21 (6) | 47 (14) | 124 (38) | 134 (41) | 3.1 ± 0.89 |
| Material resources - overall | 3.0 ± 0.84 | ||||
| Medications are not available when needed | 32 (10) | 76 (23) | 119 (37) | 97 (30) | 2.9 ± 0.96 |
| Supplies/equipment are not available when needed | 22 (7) | 59 (18) | 128 (40) | 115 (35) | 3.0 ± 0.92 |
| Supplies/equipment are not properly functioning when needed | 22 (7) | 68 (21) | 129 (40) | 105 (32) | 3.0 ± 0.92 |
| Communication/teamwork - overall | 2.8 ± 0.71 | ||||
| Unbalanced patient assignments | 28 (9) | 47 (14) | 129 (40) | 122 (37) | 3.1 ± 0.93 |
| The inadequate hand-off from the previous shift or sending unit | 38 (12) | 96 (30) | 124 (38) | 66 (20) | 2.7 ± 0.93 |
| Other departments did not provide the care needed (e.g., physical therapy did not ambulate) | 27 (8) | 99 (31) | 145 (45) | 53 (16) | 2.7 ± 0.84 |
| Lack of backup support from team members | 25 (8) | 70 (21) | 145 (44) | 86 (26) | 2.9 ± 0.88 |
| Insufficient support from the team leader | 45 (14) | 90 (28) | 107 (33) | 84 (26) | 2.7 ± 1.00 |
| Tension or communication breakdowns with other ancillary/ support departments | 29 (9) | 87 (27) | 120 (37) | 90 (28) | 2.8 ± 0.93 |
| Tension or communication breakdowns within the nursing team | 39 (12) | 91 (28) | 117 (36) | 79 (24) | 2.7 ± 0.96 |
| Tension or communication breakdowns with the medical staff | 31 (10) | 76 (23) | 125 (38) | 94 (29) | 2.9 ± 0.94 |
| The nursing assistant did not communicate that care was not done | 37 (11) | 89 (27) | 126 (39) | 74 (23) | 2.7 ± 0.94 |
| Caregiver off the unit or unavailable | 63 (19) | 79 (24) | 120 (37) | 64 (20) | 2.6 ± 1.01 |
| Performing tasks out of the nurse’s duties and responsibilities | 25 (8) | 59 (18) | 113 (35) | 129 (40) | 3.1 ± 0.94 |
| Excessive documentation and duplicate recording | 25 (8) | 33 (10) | 103 (32) | 165 (51) | 3.3 ± 0.92 |
| Inadequate supervision of nursing assistants | 50 (15) | 84 (26) | 123 (38) | 69 (21) | 2.6 ± 0.98 |
| Lack of cues or reminders | 41 (13) | 101 (31) | 130 (40) | 54 (17) | 2.6 ± 0.91 |
Reasons for Missed Nursing Care Stated by the Nurses (n = 326)
Nurses stated that “inadequate number of staff,” “unexpected rise in patient volume and/or acuity on the unit,” “inadequate number of assistive and/or clerical personnel,” “heavy admission and discharge activity,” “emotional or physical exhaustion,” and “excessive documentation and duplicate recording” were the most important reasons for the missed care.
Based on the simple logistic regression results, the job position of nurses in the ward (P = 0.001), total years of experience in nursing (P < 0.001), shift work schedule (P < 0.001), extra hours worked in the month (P = 0.025), and nursing occupational stress (P = 0.004) were significant predictors of missed care (Table 4). However, controlling for hospital effects, only shift work schedule and occupational nursing stress remained independent predictors in the multiple logistic regression model. Nurses working on day shifts significantly reported 4.5 times lower missed care than those with rotating shift schedules (P < 0.001). Also, increasing each level of occupational stress (in the range of 0 to 4) was associated with a 2.12-fold increase in the likelihood of missed care (P = 0.003).
| Characteristic | Missed Care, No. (%) | Simple Logistic Regression | Multiple Logistic Regression a | ||
|---|---|---|---|---|---|
| OR (95% CI) | P Value | Adj. OR (95% CI) | P Value | ||
| Gender | |||||
| Male | 13 (81) | 2 (0.56 - 7.18) | 0.288 | ||
| Female | 208 (68) | 1 | |||
| Age (y) | |||||
| 20 - 29 | 64 (74) | 2.28 (0.84 - 6.2) | 0.107 | ||
| 30 - 39 | 73 (77) | 2.71 (1 - 7.39) | 0.051 | ||
| 40 - 49 | 67 (61) | 1.27 (0.49 - 3.33) | 0.620 | ||
| 50 ≥ | 11 (55) | 1 | |||
| Education | |||||
| Master’s degree | 23 (74) | 1.32 (0.57 - 3.07) | 0.518 | ||
| Bachelor’s degree | 196 (69) | 1 | |||
| Marital status | |||||
| Married | 145 (67) | 0.7 (0.41 - 1.18) | 0.182 | ||
| Single/divorced/widowed | 75 (74) | 1 | |||
| Job position in the ward | |||||
| Nurse | 205 (72) | 3.26 (1.58 - 6.73) | 0.001 | ||
| Head nurse | 16 (46) | 1 | |||
| Total experience (y) | |||||
| < 5 | 70 (79) | 3.16 (1.67 - 5.97) | < 0.001 | ||
| 5 - 15 | 94 (77) | 2.88 (1.62 - 5.1) | < 0.001 | ||
| > 15 | 56 (54) | 1 | |||
| Experience on the unit (y) | |||||
| < 2 | 35 (76) | 1.71 (0.80 - 3.65) | 0.166 | ||
| 2 - 5 | 82 (73) | 1.47 (0.86 - 2.52) | 0.163 | ||
| > 5 | 95 (65) | 1 | |||
| Work shift | |||||
| Day | 32 (46) | 0.27 (0.15 - 0.47) | < 0.001 | 0.22 (0.11 - 0.42) | < 0.001 |
| Day and evening | 15 (68) | 0.66 (0.25 - 1.70) | 0.389 | 0.59 (0.2 - 1.75) | 0.345 |
| Night | 7 (70) | 0.72 (0.18 - 2.87) | 0.638 | 0.67 (0.14 - 3.16) | 0.611 |
| Rotating | 166 (76) | 1 | 1 | ||
| Number of shifts worked in the month | 1.03 (0.98 - 1.09) | 0.222 | |||
| Extra hours worked in the month | |||||
| ≤ 30 hours | 95 (63) | 0.57 (0.35 - 0.93) | 0.025 | ||
| > 30 hours | 118 (75) | 1 | |||
| Number of days/shifts absent in the past 2 months | 1.01 (0.96 - 1.07) | 0.705 | |||
| Type of employment contract | |||||
| Fixed-term contract | 29 (76) | 0.95 (0.39 - 2.33) | 0.907 | ||
| Permanent | 108 (62) | 0.49 (0.27 - 0.88) | 0.017 | ||
| Candidate of permanent | 7 (64) | 0.52 (0.14 - 1.94) | 0.326 | ||
| Temporary | 68 (77) | 1 | |||
| Type of unit | |||||
| Internal | 143 (68) | 0.94 (0.51 - 1.74) | 0.851 | ||
| Surgical | 33 (72) | 1.12 (0.48 - 2.59) | 0.788 | ||
| ICU | 43 (69) | 1 | |||
| Number of patients cared for | 1.02 (0.98 - 1.06) | 0.453 | |||
| Nursing occupational stress | 1.88 (1.22 - 2.90) | 0.004 | 2.12 (1.28 - 3.52) | 0.003 | |
The Relationship of Missed Nursing Care with Demographic and Occupational Factors by the Simple and Multiple Logistic Regressions (n = 326)
5. Discussion
In this study, a sample of a large number of nurses from small to medium size general/surgical medical and educational centers completed the MISSCARE questionnaire. It was revealed that 69% of nurses missed at least 1 nursing care activity per shift. This finding is in line with that of a pre-pandemic study conducted in Iran, demonstrating that 72% of the nurses commonly miss at least 1 essential aspect of nursing care in the medical-surgical ward per shift (1). Studies performed during the COVID-19 pandemic in Sweden and the Philippines reported that missed nursing care was about the same as before the pandemic (14, 15). The reasons stated as nurses’ management to adapt to the situation and the lower level of dependency of most COVID-19 patients than ordinary patients (16). However, a study in Jordan revealed more missed nursing care during the pandemic (22). Differences in nurses’ characteristics or outbreaks factors (such as nurse/patient ratio) may lead to this different result. In line with the result of the present study, in Ethiopia and Sweden, 74% of nurses reported that they commonly missed at least 1 aspect of nursing care (12, 23). However, a study conducted in Korea showed a higher rate of missed nursing care (84%) (3).
The present study reported that the median number of missed care items reported on each shift was 4 out of 25 (16%); in another study in Iran, it was 2.57 out of 24 (1). A study in Korea revealed that of the 24 nursing care items, 10 had a prevalence of 50% and higher missed care (5). Also, a study in Jordan showed that the frequency of missed nursing care increased during the COVID‐19 pandemic (32.6% vs 22.8%) (22). The different results may be due to a higher ratio of patients per nurse, perceived sufficiency of nurse staffing, roles of nurses and nurse assistants, and different factors related to the COVID-19 outbreak.
The most missed items in the present study were “attending interdisciplinary care conferences,” “patients’ skin and mouth care,” “emotional care and support to the patients,” and “turning patients every 2 hours”. These results are consistent with previous studies (1, 23-25). In another Iranian study, nurses reported “attending interdisciplinary care conferences” as the most omitted item (24). Accordingly, the inappropriate timing of the meetings was suggested as a possible reason (24). Nurses’ non-participation in training classes may lead to a lack of up-to-date information. It is argued that nurses’ non-formal education, short courses, and conferences can contribute to high-quality patient care (24). Only a slight difference in missed nursing activities was reported in comparison between pre and during the COVID-19 pandemic in Sweden (16). It was reported that the “response to call light initiated within 5 minutes” was missed more, and “setting up meals for patients who feed themselves” and “mouth care” were missed less than pre-pandemic (16). These differences were explained by the use of contact precautions that delay responding, as well as more independent patients who do not need assistance with daily living activities (16). A study determined that basic care interventions were the most significant missed care that patients stated in the United States (7). As such, it was identified that mouth care was missed 50.3% of the time, followed by missed ambulation, getting patients up to a chair, and bathing (7). The reason for missed care in this area could be that nurses do not prioritize them due to massive workloads or the low complexity of their conditions, or perhaps they assume that patients or their families can do this basic care independently (26).
Consistent with our finding, in another study in Iran, 64% of nurses omitted “emotional support to patients and family” (1). It seems that care activities related to the most acute physical needs (pain, surveillance, and medication) are prior, while psychosocial activities, which require more time, receive lower priority (23). Similarly, according to a European study conducted in 12 countries, nurses who missed talking or comforting reported a lack of autonomy and a huge workload (25). Also, a study demonstrated that many patients experienced difficulties in talking about their anxiety with nurses and were not satisfied with the emotional support they provided (27). Nurses are commonly referred to as an important source of psychological support for patients and their families during periods of illness and crisis (28). It could be essential to offer patients emotional support and comfort to help them better manage their condition and procedure. It is well known that healthcare professionals significantly impact patients by persuading them to share their feelings and emotions and aiding them in making decisions about their health promotion. Patients seek human contact in times of crisis (28). A previous survey suggests that patients rely on emotional health care support more than their families (7). However, another research on missed nursing care indicated the most frequently missed items as follows: “ambulation of the patients,” “attendance at care conferences,” “mouth care,” “timely medication administration,” and “turning patients” (10). Differences between studies may be due to differences between setting and sample size.
The most important reasons for missed care reported by nurses were human resources, material resources, and communication. Most previous studies have also reported that inadequate nursing staff is the most frequent reason (1, 3, 10, 17). Reasons for the lack of nursing staff are considerable workload, demographic alterations in the workforce, required clinical proficiency, and the demands for nurses in other sections (1). It is well established that nursing care is often omitted during increased workload, and low staffing is one of the primary contributing factors to this issue. The number of nurses is often 2-fold: The decline in the number of nurses in relation to the number of patients and the reduction in the number of experienced employees (29). As the lack of nursing staff has been identified as a substantial challenge for health systems, establishing effective policies to promote organizational settings to increase the nurses’ professional skills and competency is needed (1). Based on a previous systematic review, these effective policies consist of changes to payment terms, emergency recruitment, and nursing residency programs (30). Regarding “material resources,” our results are in line with previous studies conducted in 2009, 2011, and 2017, showing that nurses mentioned some inadequate material sources as a significant factor of missed nursing care (10, 31). It has been recommended that the availability of medications avoid extra delays in providing pharmacological treatments, contributing to the continuation of care (26).
In the multiple logistic regression analysis, work shift schedules and occupational stress were significant predictors of missed care. It seems that unpredictable shift schedules, increased workloads due to seasonal variations in patients in shift planning, and job-related psychological stress highly contribute to the frequency of nursing care omissions. A study in Spain showed that personal and professional feelings, stress control, and positive thinking were related to the perception of quality of care during the pandemic (23). Occupational stress can result in leaving the job, conflicts between co-workers, health disorders, job dissatisfaction, reduced creativity, reduced correct and timely decisions, feelings of inadequacy and depression, reduced energy and work efficiency, and poor nursing care (20, 21). Job-related stress levels are considered in education, health care, and social service sectors, and women are more likely to report high-stress amounts. As women dominate the nursing profession, this finding is worrisome. Accordingly, well-planned intervention programs that include individual and organizational-led prevention measures are expected to prevent burnout and improve mental health (32). In the present study, nurses with a day shift schedule reported lower missed care than nurses with a rotating shift schedule. In a study in Australia, predictors of omitted nursing care aspects consisted of shift type, nursing resources, communications between health professionals, workload amount, and the nurses’ satisfaction with their job (31). In contrast to our findings, a study in the United States identified that missed care was more reported on day shifts than on night shifts (10). Differences between studies could be due to differences in the work environment, available nursing resources, team communications, workload, COVID-19 pandemic situation, the total number of patients treated, and the patients’ length of stay.
Although the study consisted of a large number of nurses randomly selected from multiple hospitals and units, it had some limitations that could affect the generalizability of the findings. The use of nurses’ reports about their missed care in this study may be affected by social desirability. For future studies, patient reports, and direct observation may be provided additional valuable measures. Also, recording details of health system characteristics or patient-related factors may help explain some differences in the frequency of missed care or causes that were not included in this study.
5.1. Conclusions
Our findings highlight the importance of attention to missed nursing care and factors associated with poor nursing care, especially in crises. Raising the awareness of health care managers and nurses on the reasons that influence missed nursing care helps to better understand the costs and risks associated with missed care and provides more detailed guidance on identifying strategies to reduce their occurrence.