1. Background
The position of the mother during labor and birth is a crucial factor that directly impacts the health of both the mother and the fetus. Various positions, including sitting, lithotomy, lying on the side, lying on the back, kneeling, and squatting, can be adopted during the second stage of labor (1). Among these positions, kneeling is considered the most easily accessible (2). The hands and knees position is a horizontal form of the kneeling position, where the mother places her knees on the ground, leans her trunk forward, and rests her hands on the floor or bed (1). This position is classified as one with a mobile sacrum (3). The hands and knees position is comfortable for mothers and enables them to move their pelvis in various directions, such as up/down, left/right, or even rotate it. This movement facilitates the adjustment of the fetus’s head with the pelvis by allowing for the rotation of the fetus’s head and modifying the occiput transverse and posterior (OT-OP) position and asynclitism (1). Additionally, it is claimed that this position reduces pressure on the umbilical cord, improves the fetus’s heart rate pattern, alleviates back pain and muscle spasms, reduces pressure on the back and pelvic muscles, helps with releasing shoulders in the case of shoulder dystocia, relieves symptoms of hemorrhoids, and facilitates easier vaginal examinations (1, 4).
Previous studies have conducted comparisons between maternal and fetal outcomes of different kneeling positions and the supine position, yielding conflicting results. In one study, the mean duration of the second stage of labor was found to be shorter by approximately 16.90 minutes in nulliparous and multiparous parturients in the kneeling position compared to the supine position (RR-2.275). The incidence of second-degree tears in nulliparous mothers in the kneeling position was significantly higher than in the supine position (RR 4.191), while no significant difference was observed between primiparous and multiparous mothers. There was no significant difference in the frequency of Apgar scores above 7 at the fifth minute between the two groups (RR 1.2772). However, the rate of NICU hospitalization was significantly lower in the kneeling group compared to the supine group (2). In another clinical trial, mothers were divided into three groups: Hands and knees, squatting, and lithotomy positions during the second stage of labor. The results showed no statistically significant differences among the groups in terms of the average duration of the second stage of labor, the degree of perineal tears, and the average Apgar score at 1 - 5 minutes (5). In a separate study, mothers were placed in three positions: Lithotomy, kneeling, and sitting from the beginning of the second stage of labor. The duration of the second stage of labor was shorter in the kneeling group compared to the lithotomy group (6).
Despite the World Health Organization’s warning about the risks associated with the lithotomy position for labor and the evidence supporting the positive effects of non-supine positions such as hands and knees on maternal and fetal outcomes, the lithotomy position remains the most commonly used position for childbirth (7). Unfortunately, in Asian countries, the kneeling position is rarely used during labor due to a lack of knowledge and skills among midwives and obstetricians (8). Despite receiving education on non-supine positions, midwives and obstetricians do not routinely apply them in the clinic. Although various labor positions are taught to mothers in labor preparation classes, these positions are not recommended by midwives and obstetricians during the actual labor, resulting in mothers routinely giving birth in the supine position (7).
On the other hand, one of the key objectives of midwives and obstetricians in Iran is to increase the rate of physiological birth and reduce the rate of cesarean sections. Non-supine positions during labor and birth are considered one of the most beneficial and effective techniques for achieving physiological birth (9). However, there have been limited studies worldwide comparing maternal and neonatal outcomes between the lithotomy position and the hands and knees position. Furthermore, in Iran, no study has yet compared maternal and neonatal outcomes, specifically between the hands and knees position and other positions.
2. Objectives
The present study aimed to compare the maternal and fetal outcomes between the lithotomy and hands and knees childbirth positions in both primiparous and multiparous women.
3. Methods
3.1. Study Design
The present study was a two-group single-blind randomized clinical trial with a parallel design, where information was collected from the studied groups.
3.2. Participant and Setting
The present study was conducted on 72 parturient women who were referred to selected hospitals in Isfahan, Iran, for childbirth. The hospitals included Asgarieh, Shahid Beheshti, Hazrat-e-Zahra in Zeinabieh, and Motahhari in Fooladshahr, and the study period was from December 2021 to March 2022. These hospitals were chosen based on their high referral rates and included university-affiliated, charity, and private hospitals.
3.3. Inclusion and Exclusion Criteria
The inclusion criteria for this study were as follows: Having a history of at least one term vaginal birth, having a term and live singleton fetus in cephalic presentation without any disorders, not receiving oxytocin during the first stage of labor, successfully passing the first stage of birth physiologically, estimated fetal weight between 2500 and 4000 grams using Johnson’s rule (10), no contraindications for vaginal birth, cervical dilation of approximately 8 cm, previous experience of birth in the lithotomy position, absence of prior cesarean section or uterine surgery, absence of any significant medical or psychological conditions, no severe pregnancy complications during the current pregnancy (such as severe preeclampsia or placental abruption), normal physical and psychological condition during labor, no use of epidural analgesia or other medicinal pain relief methods, and no physical limitations that would hinder the mother from assuming the intended labor position (such as knee or wrist pain). The exclusion criteria for this study included the presence of a compromised fetal heart rate pattern during labor or birth, the need for instrumental delivery or cesarean section, and the mother’s voluntary withdrawal from participation or her willingness to change her labor position.
3.4. Sample Size Calculation
Based on a similar study (11), the required sample size for each group was calculated to be 32, which was increased to 36 to account for a 10% dropout rate. This calculation considered a 95% confidence level, 80% power, and an estimated standard deviation of 0.7 for each variable.
3.5. Randomization
For recruitment, the names of the settings were written on cards and placed in sealed pockets. One pocket was randomly selected each day, and sampling was done using a convenient method, which means that every woman who met the inclusion criteria and was referred to the hospital for childbirth was enrolled in the study. To allocate participants randomly to the groups, each participant selected a sealed, non-transparent pocket out of the 90 prepared pockets. Forty-five pockets contained a questionnaire and checklist with code 1 (lithotomy group), and the other 45 contained a similar questionnaire and checklist with code 2 (hands and knees group). To ensure randomization concealment, 45 pockets were assigned to each group. Sampling continued until each group reached a minimum of 36 participants. Instead of using the terms “lithotomy” and “hands and knees,” codes 1 and 2 were written to achieve blinded statistical analysis.
3.6. Measurements and Data Collection
The primary outcomes of the study included the duration of the active phase of the second stage of labor (the second stage of delivery is divided into two phases: The latent phase starts at full dilation and ends at pushing. The active phase starts with pushing and ends at the birth of the newborn. The active phase was characterized by involuntary pushing in the second stage of labor) (1), the total duration of the second and third stages of labor, the occurrence of shoulder dystocia, the amount of bleeding during the third and fourth stages of labor, the difference in hemoglobin and hematocrit levels at 6 hours after birth and at the time of hospitalization, the degree of perineal tears, the neonate’s Apgar score, the need for neonatal resuscitation and its level, and the need for neonatal hospitalization. No secondary outcomes were evaluated.
Data for the present study were collected through observation, examination, interviews, and the completion of a researcher-made questionnaire. The questionnaire consisted of three parts. The first part collected information on the participants’ demographic characteristics, including the mother’s age, occupation, education, and place of residence. The second part focused on the fertility characteristics of the parturient woman and the characteristics of the neonate, such as the number of pregnancies, deliveries, abortions, live children, gestational age, neonate’s weight, fetus’ weight based on the Johnson criterion, head circumference, and the position of the fetus’ head at the time of birth. The third part included data on maternal and fetal outcomes.
Time was measured using a chronometer in all deliveries. Initially, this device was calibrated, and its accuracy was assessed every morning. The amount of bleeding was measured using a researcher-made graded drape consisting of thick plastic with a bent bottom, pressed and shaped into a triangular form, graded in terms of cc in a single center. Hemoglobin and hematocrit levels were routinely measured during hospitalization and 6 hours after birth, and the relevant information was extracted from the participants’ medical records. The Apgar table is a standardized tool with proven validity and reliability in multiple scientific sources (12, 13).
3.7. Procedures
Initially, as a pilot study, the researcher planned to carry out five births alongside the questionnaire, measure and record the variables of the five mothers, and identify potential issues. It should be noted that the information from these five mothers was not included in the statistical analysis. Following a thorough evaluation of the patient’s medical history and assessment of their eligibility, written informed consent was obtained for their participation in the study. The researcher utilized the Johnson rule to estimate and record fetal weight. The researcher conducted all the births and personally measured and recorded the outcomes using the same questionnaire. The participants were enrolled in the study once their cervix was dilated to 8 cm and were subsequently monitored and supervised. For laboring women who were expected to assume the lithotomy position, they were positioned on the lithotomy bed after full dilation of the cervix, with their thighs and knees bent and open. The head of the bed was elevated to 30 degrees, and during contractions, the mother was allowed to straighten her legs as desired. In the hands and knees group, mothers were positioned with their palms resting on a regular bed and their legs kneeling on the bed after full dilation of the cervix. In both positions, mothers were given the option to lie on their side of the bed between contractions if desired. The questionnaire recorded the following times: Full dilation, the onset of spontaneous pushing, fetal birth, placental delivery, and one-hour post-birth. In cases involving shoulder dystocia and fetal resuscitation, the necessary measures taken to address the issue and the final outcomes were also documented in the questionnaire. The neonate’s recovery level was observed and documented in the questionnaire. In both positions, following birth, the researcher attended to the neonate and cut the umbilical cord within the first minute. After the umbilical cord was cut, the mother was positioned on her back, and the neonate was placed on her chest. A graded drape with a collection tank was placed beneath the mother’s buttocks, remaining there for the first hour after placental delivery. This allowed for the measurement and recording of the amount of blood collected in the tank during the third and fourth stages of labor (from the time of fetal birth until one hour after placenta delivery). Following the birth of the placenta, all participants received routine oxytocin administration (20 units intravenously in Ringer’s solution).
If deemed necessary, an episiotomy incision was performed. Following placental delivery, the researcher examined the perineum to assess the extent of tearing and subsequently performed the necessary repairs. The neonate’s Apgar score was determined by the researcher using the Apgar table at both the first minute and fifth minute after birth. Within the first hour after birth, the neonate’s weight was measured using a digital scale (Laica). The researcher compared the hemoglobin and hematocrit levels at the time of hospitalization with those 6 hours after birth, noting the difference in the questionnaire.
3.8. Data Analysis
In the current study, data were analyzed using descriptive statistics (mean, standard deviation, ratio, and frequency distribution) as well as inferential statistics with SPSS 16 (IBM, Armonk, NY, United States of America). The Mann-Whitney test was employed to compare numerical qualitative variables, while the independent t-test was used for quantitative variables with a normal distribution. Fisher’s exact and chi-square tests were used to analyze qualitative variables. The Kolmogorov-Smirnov test was conducted to assess the normality of data distribution. A significance level of less than 0.05 was set.
3.9. Ethical Considerations
The study was conducted in accordance with the ethics code IR.MUI.NUREMA.REC.1400.086, approved by the ethics committee of the Isfahan University of Medical Sciences. Additionally, it was registered and approved on the Iranian Registry for Clinical Trials website with the code IRCT20091001002531N5.
Prior to commencing the study, participants were provided with information regarding the objectives and methodology of the research, and written informed consent was obtained. Participants were assured that they had the option to withdraw from the study at any point without any adverse effects. They were also guaranteed full care and access to medical services regardless of their decision to continue or discontinue their participation.
4. Results
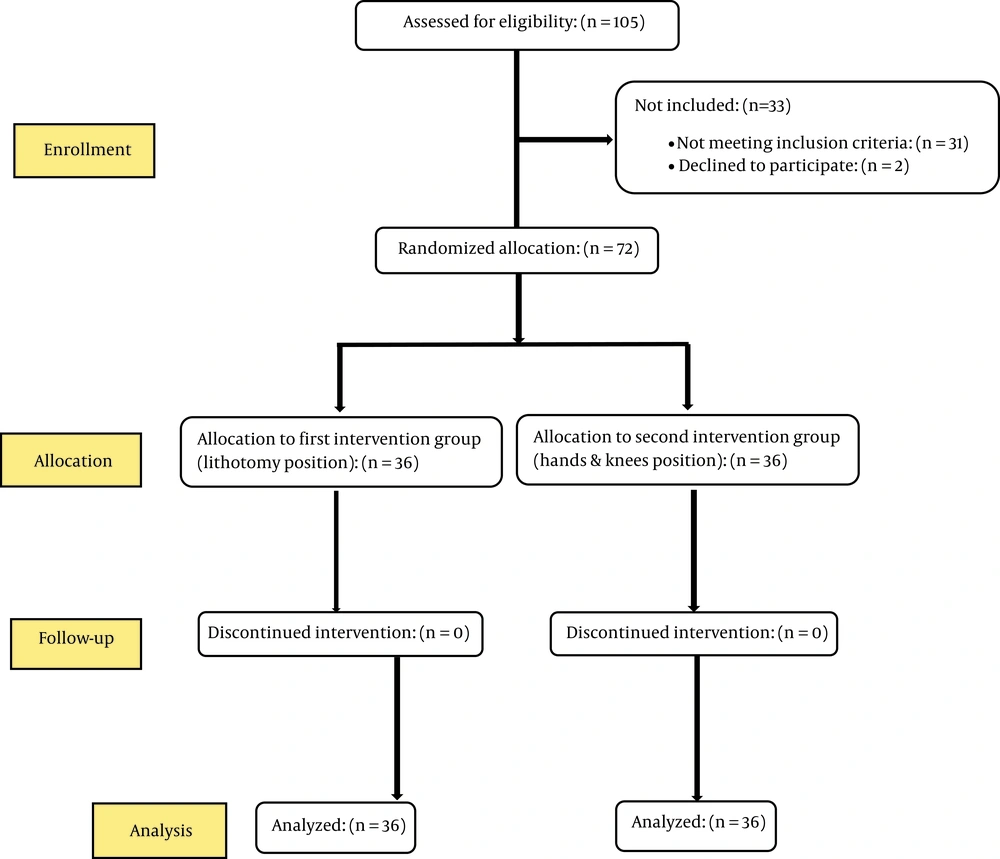
In this study, analysis was conducted on 36 mothers in each group (Figure 1). There were no significant differences observed between the two groups in terms of demographic characteristics, including age, occupation, educational level, and place of residence of the mothers, as well as fertility characteristics such as the mean number of pregnancies, number of vaginal deliveries, number of live children, gestational age, and frequency of previous abortions. Additionally, no significant differences were found between the groups in fetal and neonatal characteristics, including the mean weight of the fetus according to the Johnson rule, neonate’s weight, neonate’s circumference, and frequency of the fetus’ head position at the time of birth (P > 0.05) (Tables 1 and 2).
| Variables | Lithotomy | Hands and Knees | Statistical Test | P-Value c |
|---|---|---|---|---|
| Mother’s age (y) | 28.44 (4.34) | 28.58 (4.76) | t = 0.13 | 0.90 |
| Number of pregnancies | 2.81 (0.58) | 2.86 (0.54) | t = 0.42 | 0.67 |
| Number of vaginal deliveries | 1.72 (0.45) | 1.75 (0.43) | t = 0.26 | 0.79 |
| Number of live children | 1.64 (0.49) | 1.69 (0.47) | t = 0.49 | 0.62 |
| Gestational age (w) | 38.97 (0.88) | 38.95 (1.55) | t = 0.04 | 0.97 |
| Educational level | Z = 0.66 | 0.51 d | ||
| Illiterate | 12 (33.30) | 14 (38.90) | ||
| Elementary school | 10 (27.80) | 11 (30.60) | ||
| Guidance school | 4 (11.10) | 3 (8.30) | ||
| Diploma | 9 (25) | 7 (19.40) | ||
| University | 1 (2.80) | 1 (2.80) | ||
| History of abortion | 0.50 e | |||
| No | 33 (91.70) | 32 (88.90) | ||
| Yes | 3 (8.30) | 4 (11.10) | ||
| Place of residence | χ2 = 0.53 | 0.46 f | ||
| Urban | 24 (66.70) | 21 (58.30) | ||
| Rural | 12 (33.30) | 15 (41.70) |
a Values are presented as No. (%) or mean ± SD.
b All the mothers in both groups were housewife.
c Independent t-test
d Mann-Whitney
e Fisher’s exact test
f Chi-square test
| Variables | Lithotomy | Hands and Knees | Statistical Test | P-Value b |
|---|---|---|---|---|
| Estimated fetal weight in labor according to the Johnson formula (gr) | 3356.81 (280.47) | 3442.36 (344.14) | t = 1.16 | 0.25 |
| Neonate’s weight at birth (gr) | 3189.03 (291.96) | 3313.61 (339.03) | t = 1.67 | 0.10 |
| Neonate’s circumference (cm) | 34.58 (0.86) | 34.78 (2.55) | t = 0.44 | 0.66 |
| Fetus’ head position in the labor | 0.50 c | |||
| Posterior occiput | 1 (2.80) | 0 (0.00) | ||
| Anterior occiput | 35 (97.20) | 36 (100) |
aValues are presented as No. (%) or mean ± SD.
b Independent t-test
c Fisher’s exact test
No significant difference was observed between the two groups in terms of the mean duration of the active phase of the second stage of labor, the total duration of the second stage of labor, the duration of the third stage, the amount of bleeding during the third and fourth stages, the difference in hemoglobin and hematocrit levels at the time of hospitalization and 6 hours after birth, Apgar scores at the first and fifth minutes after birth, frequency of shoulder dystocia, the degree of perineal tears and episiotomy, neonate’s need for hospitalization, and neonate’s need for resuscitation (P > 0.05) (Tables 3 and 4).
| Neonatal Outcomes | Lithotomy | Hands and Knees | Statistical Test | P-Value b |
|---|---|---|---|---|
| Occurrence of shoulder dystocia | 0.50 | |||
| Yes | 1 (2.8) | 0 (0) | ||
| No | 35 (97.2) | 36 (100) | ||
| Need for neonatal resuscitation | 0.50 | |||
| Yes | 1 (2.8) | 0 (0) | ||
| No | 35 (97.2) | 36 (100) | ||
| Need for neonate’s hospitalization | 1 | |||
| Yes | 1 (2.8) | 1 (2.8) | ||
| No | 35 (97.2) | 35 (97.2) | ||
| First-minute Apgar | 8.94 (0.33) | 9 (0) | t =1 | 0.32 c |
| Fifth-minute Apgar | 10 (0) | 10 (0) | 1 c |
a Values are presented as No. (%) or mean ± SD.
b Fisher’s exact test
c Independent t-test
| Maternal Outcomes | Lithotomy | Hands and Knees | Statistical Test | P-Value b |
|---|---|---|---|---|
| Duration of the active phase of the second stage (min) | 7.17 (3.05) | 7.25 (3.11) | t = 0.11 | 0.91 |
| The total duration of the second stage (min) | 10.58 (3.40) | 10.67 (4.14) | t = 0.09 | 0.93 |
| Duration of the third stage (min) | 5.42 (1.70) | 5.03 (0.97) | t = 1.19 | 0.24 |
| Amount of bleeding during the second and third stages (cc) | 403.33 (70.02) | 429.44 (81.10) | t = 1.46 | 0.15 |
| Hemoglobin difference between the time of hospitalization and 6 hours after birth(mg/dL) | - 0.56 (0.07) | - 0.72 (0.12) | t = 1.14 | 0.26 |
| Hematocrit difference between the time of hospitalization and 6 hours after birth | - 1.39 (0.18) | - 1.94 (0.24) | t = 1.83 | 0.07 |
| Perineal tears degree | Z = 0.56 | 0.58 c | ||
| No tear | 18 (50.00) | 19 (52.80) | ||
| First-degree tear | 15 (41.70) | 17 (47.20) | ||
| Second-degree tear | 3 (8.30) | 0 (0.00) |
a Values are presented as No. (%) or mean ± SD.
b Independent t-test
c Mann-Whitney
5. Discussion
The current study aimed to compare maternal and fetal outcomes between two birth positions (lithotomy and hands and knees) among hospitalized women at selected hospitals in Isfahan in 2021.
5.1. Duration of the Second and Third Stages of Labor
The study results revealed no significant statistical difference between the two groups regarding the mean duration of the active phase of the second stage of labor and the total duration of the second and third stages of labor. In both groups, all deliveries were conducted physiologically without synthetic oxytocin, with the researcher present providing full support. Previous research suggests that the presence of a consistent supporter during birth can reduce the duration of labor (14), as it helps alleviate the mother’s stress and pain and prevents the release of cortisol and adrenaline, which can potentially delay the birth process (1). This could potentially explain the lack of significant difference in the mean duration of labor stages between the two groups in the present study. This finding aligns with the results of a clinical trial that found no significant difference in the mean duration of the second stage of labor among three different labor positions: lithotomy, squatting, and hands and knees (5). In contrast, a semi-experimental study observed a faster fetal birth in the second stage of labor in 70 out of 73 cases in the upright labor position (where mothers were upright during the first stage of labor and then assumed the hands and knees position during the second stage of labor), compared to 19 out of 77 cases in the supine labor position; this difference was statistically significant (P < 0.001) (15). The results of the present study contradicted the findings of the mentioned study. In the mentioned study, the researchers maintained an upright position for the mothers throughout the entire first stage of labor, which had a positive impact on resolving asynclitism and facilitating better alignment of the fetus with the pelvis, potentially leading to a shorter duration of the second stage of labor (1). Another semi-experimental study found that positions allowing for a flexible sacrum resulted in a shorter mean duration of the second stage of labor compared to positions with a non-flexible sacrum (P < 0.000) (16). The results of the present study were inconsistent with the aforementioned study, as mothers in the present study were allowed to choose their preferred labor position from the beginning of the active phase. Opting for their preferred labor position may have also contributed to a reduction in maternal stress (1). Furthermore, a systematic review demonstrated that the mean duration of the second stage of labor was 21.12 minutes shorter in positions with a flexible sacrum compared to positions with a non-flexible sacrum (P < 0.001) (17). The results of the present study were inconsistent with the findings of the mentioned study. This discrepancy in results can be attributed to different definitions of the beginning of the second stage. For instance, some studies defined the start of the second stage as the onset of pushing (active phase of the second stage), while others considered it as the occurrence of 10 cm dilation during the physical examination of the mother. Additionally, variations in positions and mothers’ parity across different studies should be taken into account (17, 18). Notably, the hands and knees position is characterized by a mostly horizontal alignment of the line between the third and fourth vertebrae, resembling a horizontal kneeling position where gravity plays a lesser role in the fetal delivery process (19).
5.2. Shoulder Dystocia
The frequency of shoulder dystocia did not exhibit a significant difference between the two groups. The results of the present study were not consistent with those of another study, which indicated that placing parturient women in the hands and knees position during the second stage of labor significantly reduced the likelihood of shoulder dystocia compared to the lithotomy position (P = 0.04) (4). However, the results of the present study were inconsistent with the aforementioned study. It is not reasonable to directly compare the results of the mentioned study with the present study due to different inclusion criteria. In the present study, one of the inclusion criteria was that the estimated fetal weight should be less than 4000 grams. As fetal weight is an important factor in the occurrence of shoulder dystocia, the probability of shoulder dystocia was low in both groups (12). On the other hand, in the mentioned study, a fetal weight of less than 4000 grams was not among the inclusion criteria. Despite the neonates’ normal weight in both groups in the present study, one case of shoulder dystocia occurred in the lithotomy group, which was resolved using the McRoberts maneuver and applying suprapubic pressure.
5.3. Bleeding
The mean amount of bleeding during the third and fourth stages of labor and the difference in hemoglobin and hematocrit scores between the time of hospitalization and 6 hours after birth did not exhibit a statistically significant difference between the two groups. It is important to note that induced labor is considered a risk factor for postpartum bleeding, whereas, in physiological birth, the amount of bleeding is within the physiological range (20, 21). In the present study, both groups experienced physiological birth. The results of the present study were consistent with those of a clinical trial, which indicated no significant difference in the amount of bleeding between the supine position and the hands and knees position. Additionally, no cases of bleeding exceeding 1000 mL were observed in either group. However, the mentioned study did not provide explanations regarding the method used to measure the amount of bleeding, raising concerns about the validity of the data (4). Additionally, another study found no significant difference in the amount of bleeding exceeding 500 mL between upright and supine positions (15). The results of the present study were consistent with the findings of the mentioned study. However, in a separate study, the amount of postpartum bleeding was higher in upright positions compared to supine positions (P = 0.002). The results of the present study were inconsistent with the results of the mentioned study. To explain this difference, it is important to consider the variety of positions studied (22). Furthermore, the method of measuring the amount of bleeding varies among different studies. Positions that align with gravity, such as sitting or squatting, may result in increased postpartum bleeding due to the greater impact of gravity, faster progression of labor stages, increased pressure on the perineum, and more perineal damage. However, in the hands and knees position during the second stage of labor, the reduced effect of gravity, the possibility of perineal support by the labor assistant, and decreased pressure on the perineal area may lead to decreased perineal damage and, consequently, reduced postpartum bleeding as well (23).
5.4. Degree of Perineal Tears
Episiotomy was not performed for any participants in either group, and there were no third- or fourth-degree tears. The frequency distribution of perineal tears based on their degree showed no significant difference between the two groups. In the present study, none of the participants in either group received oxytocin. The use of oxytocin is a risk factor for an increase in perineal damage (24). It is possible that the absence of oxytocin administration contributed to the absence of severe perineal damage in the present study. Previous studies have demonstrated that spontaneous pushing and allowing mothers to choose their preferred labor positions can reduce the risk of perineal damage (25, 26). The results of the present study were consistent with those of a semi-experimental study, which found no significant difference in the application of episiotomy or the frequency of first- and second-degree perineal tears between upright positions (where mothers were in an upright position during the first stage of labor and in a hands and knees position during the second stage) and the supine position. Furthermore, no cases of third- or fourth-degree tears were observed (15). Also, in another study, no significant relationship was observed between positions with a flexible sacrum and the occurrence of tears requiring repair or anal/rectum sphincter tear. In positions with a flexible sacrum, the need for episiotomy was lower compared to other groups (P < 0.01) (27). The results of the present study were consistent with the mentioned study. On the contrary, in a different study, the frequency of no perineal tear and first-degree tear was higher in the hands and knees group compared to the supine group (P < 0.001). However, the frequency of second-degree tears was significantly lower in the supine group compared to the hands and knees group (P < 0.001). The results of the present study were inconsistent with the mentioned study. The researchers of the mentioned study claimed that the improvement of perineal blood supply was the reason for the decreased occurrence of second-degree tears in the hands and knees group (4). In the mentioned study, unlike the present study, different midwives/obstetricians were involved in the deliveries, and the varying skill levels of these practitioners could have influenced the results. Additionally, in the mentioned study, the hands and knees position involved raising the bed’s head by 30 to 60 degrees. In contrast, in the present study, the mothers maintained a completely horizontal position with their shoulders and hips at the same level during hands and knees positions. The results of the present study were different from those of a semi-experimental study where the frequency of perineal damage was lower in positions with a flexible sacrum compared to positions with a non-flexible sacrum (P < 0.05) (16). The results of the present study contradicted the mentioned study. In both the control and intervention groups, mothers were assigned from the beginning of the active phase of labor. Upright positions have been shown to improve blood supply to the pelvis (1). Upright positions such as sitting, squatting, and upright kneeling can shorten the duration of the second stage of labor, resulting in a faster delivery of the fetus through the birth canal. This reduced duration may increase the risk of a perineal tear due to less time for tissue stretching and traction. Conversely, lying on the side and hands and knees positions, which do not expedite the second stage of labor, allow mothers to freely move their pelvis, minimize external pressure on the perineum, provide better access for the labor assistant to support the perineum, and reduce the pressure on the perineum, thereby decreasing the risk of damage (23).
5.5. Apgar
First and fifth-minute Apgar scores did not differ significantly between the two groups, as both groups in the present study underwent physiologic birth with no significant variation in the duration of the second stage of labor (1). These findings align with those of a clinical trial that reported no significant difference in asphyxia and neonate’s Apgar score between hands and knees and supine positions (4). Conversely, a semi-experimental study indicated a significant difference in the first-minute Apgar score between upright positions (where mothers were positioned upright during the first stage of labor and in hands and knees position during the second stage) and supine positions. The supine group had a lower Apgar score of less than 7 compared to the upright group (P = 0.018). However, there was no significant difference in the fifth-minute Apgar score between both groups (15). The results of the present study were inconsistent with the results of the previous study regarding the first-minute Apgar score. To explain this difference, it should be noted that in the previous study, the intervention group’s mothers maintained an upright position during the active phase of the first stage and throughout the second stage of labor. A semi-experimental study demonstrated a lower frequency of Apgar scores of less than 7 in positions with a flexible sacrum compared to positions with a non-flexible sacrum (P < 0.05) (16). The results of the present study were inconsistent with the results of the previous study.
5.6. Neonatal Resuscitation and The Neonate’s Need for Hospitalization
The frequency of the need for neonatal resuscitation and hospitalization showed no significant difference between the two groups in the present study. The results of the present study were consistent with a systematic review that indicated no significant difference between upright and supine positions regarding the need for neonate hospitalization in NICU (18). On the other hand, a clinical trial reported a significantly lower rate of hospitalization in the NICU in the kneeling position group compared to the supine position group (P = 0.016) (2). The results of the present study were inconsistent with this study. Theoretically, reducing pressure on the inferior vena cava and aorta during labor would enhance blood supply to the uterus, potentially improving neonatal and fetal outcomes (12).
5.7. Limitations and Strengths
One limitation of the present study was that participants in the hands and knees group had variations in their positions during the second stage, including lying on their side between contractions, which could have influenced the results. However, from an ethical standpoint, it was not feasible to enforce a strict hands and knees position for the entire duration. Another inherent limitation was the lack of blinding for the evaluator.
The strengths of the present study included the study design, which was a randomized clinical trial that allowed for the evaluation of various outcomes. Additionally, all births were physiologically performed by the same midwife, ensuring consistency in the delivery process.
5.8. Conclusions
There were no significant differences between the two groups in terms of the mean duration of the active phase of the second stage of labor, the total duration of the second and third stages of labor, the amount of bleeding during the third and fourth stages of labor, the difference in hemoglobin and hematocrit levels between 6 hours after birth and the time of hospitalization, the first and fifth-minute Apgar scores, the frequency of shoulder dystocia, the degree of perineal tears and episiotomy, the neonate’s need for hospitalization, and the need for neonatal resuscitation. The maternal and fetal outcomes observed in the hands and knees position were comparable to the routine position used in hospitals in Iran, lithotomy. Therefore, midwives and mothers can choose the hands and knees position without concerns.