1. Background
Since December 2019, the world has encountered a new infectious disease called coronavirus which has quickly spread worldwide. On January 30, 2020, the World Health Organization declared a public health emergency of international concern (1). High workload, limited access to personal protective equipment, grief over the death of colleagues, the worry about being infected and transmitting the infection to their family, over-enthusiastic media news, and feeling inadequately supported were the causes of adverse psychological consequences (2-4). Moreover, social stigmatization is a significant issue among frontline healthcare workers (5). The sudden role change from a healthcare provider to a confirmed or suspected coronavirus disease 2019 (COVID-19) patient causes healthcare professionals frustration, helplessness, and adjustment problems (6).
With the spread of infectious diseases, especially COVID-19, healthcare workers are vulnerable to mental health problems. A review study showed that healthcare workers experienced significant stress, anxiety, and depression due to the COVID-19 pandemic (2). A study has demonstrated the prevalence rates of depression (74.1%), anxiety (89.7%), and stress (54.9%) in the Iranian nurses who provided care to patients with COVID-19 (7). Additionally, another study among Iranian nurses has shown that anxiety, stress, and depression scores increased significantly during the first wave of the COVID-19 epidemic compared to before COVID-19 (8).
Healthcare workers have been experiencing a persistent burden of psychological distress that can have adverse consequences for health systems during this public health crisis (9). They suffer adverse psychological consequences during the pandemic and in the long term (10). A study has indicated that nurses experience burnout, traumatic stress, anxiety, and depressive symptoms even 1 to 2 years after the outbreak (11). The National Health Commission issued a notice on February 15, emphasizing the significance of psychological interventions and support for medical staff (12). Maintaining the mental health status of medical staff is essential for better control of the pandemic (13). Psychological programs should be implemented immediately to manage mental healthcare for healthcare workers on the frontline against COVID-19 (14). Since the nurses have more workload and more risk of exposure (staying longer in the ward and providing direct care to the patients), they have a higher risk of developing symptoms of anxiety or depression (15).
Logotherapy is based on the belief that pain and suffering are an inseparable part of life, and when the individual finds meaning in suffering, it will no longer be annoying (16, 17). One of the fundamental desires of humans and the basic driving force of life is to find meaning and purpose that relieve individuals of their suffering and bring spiritual well-being (18, 19). On the other hand, among the many forms of coping described by Lazarus and Folkman, meaningful and positive reappraisal structure is particularly prominent (20). Through meaning-based coping, stressful events can be reconstructed as benign, valuable, or beneficial (20). Due to the long-term stressful situation for those on the front lines of the fight against the COVID-19 pandemic, the availability of meaning-based resources will help manage such stress successfully (21).
Significant evidence shows that culture and context impact the diagnostic and treatment process (22). Many studies showed that culture significantly affects attention, perception, thinking and attributing, cognition, motivation, interpersonal behavior, and group dynamics (23, 24). In Iranian culture, Maulana Jalaluddin Balkhi Rumi took effective steps in the path of self-knowledge. Rumi’s thoughts can noticeably influence how individuals deal with problems. Rumi’s thoughts will enhance meaning-based coping.
On the other hand, metaphors and allegories are very important in Iranian culture in conveying concepts. Metaphors and stories help transform therapeutic information into a form that is easy to remember, is applicable in everyday life at relevant moments, and provides valuable guidance (25). Empirical evidence has indicated that patients’ self-management skills were improved using metaphor in a solution-focused approach (26). The fact that Rumi conveys his most profound thoughts with metaphors and allegories more than other philosophers motivated the researchers to use the works of this prominent philosopher.
2. Objectives
This study aimed to evaluate the effectiveness of Logotherapy Based on Rumi’s Thoughts (LBRT) in anxiety, depression, and distress of frontline nurses during the COVID-19 pandemic.
3. Methods
3.1. Research Design and Setting
This quasi-experimental study was conducted on the frontline nurses of Imam Khomeini and Fatemeh Zahra hospitals, Mazandaran, Iran, during the COVID-19 pandemic 2020, using a pre-test-post-test design and a 2-month follow-up period. The reason for selecting these two hospitals was that these centers are references for medical referrals for COVID-19. Moreover, they are the main educational and medical centers of the Mazandaran University of Medical Sciences, Mazandaran, Iran, and provincial referral centers. Each hospital was assigned to one group (Imam Khomeini Hospital to the intervention group and Fatemeh Zahra Hospital to the control group) to avoid sharing concepts between the intervention and control groups. The study population was selected through the convenience sampling method. The inclusion criteria included working on the front lines as a nurse during the COVID-19 pandemic.
On the other hand, the exclusion criteria were (1) severe mental disorders, (2) having suicidal thoughts, (3) recent psychological intervention, and (4) absence from more than two sessions. The individuals were screened by telephone to determine eligibility for the study. In line with the related literature (27, 28), 32 nurses were selected in this study and placed in two intervention and control groups. The intervention group received LBRT; however, the control group received no treatment. Online services were used in this study because, during the COVID-19 pandemic, online mental health services facilitated the development of public emergency interventions (15).
3.2. Sampling and Data Collection
The nurses interested in participating in this study received information about the study. After obtaining written informed consent from the participants, the online survey link was sent to them. This survey included a demographic form and questionnaires assessing depression, anxiety, and distress. After completing the pre-test, the link to the 90-minute online class was sent to them. Due to the unpredictable conditions during the COVID-19 pandemic, each session was recorded and sent to participants to review. After eight sessions of intervention and 2 months, the link to the post-test and follow-up questionnaires was sent to the participants. The study staff was always available to answer questions about the problem of accessing the online class by phone. The person analyzing the data was outside the treatment team and was not aware of the participants’ intervention.
3.3. Research Tools
Instruments for this study included the sociodemographic questionnaire, Impact of Event Scale-Revised (IES-R), and Hospital Anxiety and Depression Scale (HADS). The socio-demographic data included age (in year), gender (male/female), educational level (undergraduate/postgraduate), and marital status (married/unmarried).
Hospital Anxiety and Depression Scale (HADS): The questionnaire consists of two subscales, one related to depression and the other to anxiety. Each subscale includes 7 items with a 4-point sequential response format. Scores range from 0 to 21 on each subscale, with higher scores indicating higher levels of anxiety or depression. The internal consistency was 0.92 and 0.88 for the anxiety and depression subscales, respectively. Moreover, Cronbach’s alpha was 0.87 and 0.81 on the anxiety and depression subscales, respectively (29). In Iran, the scale had acceptable validity and reliability (Cronbach’s alpha of 0.78 and 0.86 for anxiety and depression, respectively) (30). In some studies, the HADS was used for evaluating nurses’ anxiety and depression (31, 32).
Impact of Event Scale-Revised (IES-R): Lai et al. assessed the distress of healthcare workers exposed to the coronavirus by the IES-R (33). This questionnaire was developed by Weiss and Marmar (1997) based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria to diagnose post-traumatic stress disorder (PTSD). This questionnaire consists of 22 items, and its purpose is to assess the components of mental helplessness in the face of specific life events (i.e., avoidance, intrusion, and hyperarousal). The answers are based on a Likert scale rating from 0 to 4 in the order of never, sometimes, often, and extremely. This scale includes three subscales for avoidance (8 items), intrusive thoughts (7 items), and hyperarousal (7 items). Generally, higher overall scores on this scale indicate higher mental helplessness and vice versa. In Iran, this scale was translated into Persian by Sharif Nia (34). The Cronbach’s alpha coefficients for each of the three domains were high (range: 0.84 - 0.93) (34).
3.4. Intervention
Logotherapy Based on Rumi’s Thoughts was designed by Norouzi et al. (35-37). It was originally designed for the psychological well-being and adjustment of the elderly (36); however, this study targeted the challenges of nurses during COVID-19. The intervention consisted of eight 90-minute sessions held twice a week. A summary of these sessions can be observed in Table 1. The participants were instructed to report on the applicability and effectiveness of the techniques taught in each session during relevant moments in their daily lives as part of their home practice.
| Session Topic | The Summary of the Session | Assignment |
|---|---|---|
| 1- Sense of source | (1) Attention and focus on the sense of source, (2) self-monitoring, (3) comparison of the mother-child relationship with the relationship between God and man based on the story of Abbas and his Mother (sense of source), (4) interpretation and analysis of two ghazals of Rumi | According to the story of “Abbas and his Mother” and the interpretation of Rumi’s two ghazals, write your thoughts, body sensations, and feelings in 10 lines by focusing on the call to prayer or the church bell or ... |
| 2- Self-regulation | (1) Interpretation of the allegory “Chinese and Romans in Painting”, (2) interpretation of the allegory “Wheat Warehouse”, (3) interpretation of the allegory “Thistles and the person who uproots them”, (4) interpretation of the allegory “The simile of the world to the furnace of the bathroom”, (5) knowing one’s abilities and interests and setting goals for them, (6) knowing one’s positive and negative features and setting goals for them | According to Rumi’s allegories about self-regulation, be aware of your sufferings, reappraise situations, and regulate your thoughts, behaviors, and emotions again. Moreover, list your positive and negative features, interests, abilities, and goals (3 items each), and regulate them again. |
| 3- Acceptance | (1) Based on the allegories of “The old man and the Doctor” and “The Mystic and Priest,” accept the current situation, (2) the importance of wisdom maturity, (3) the strategy of problem-solving based on attitude change | List 10 specific problems in your personal and professional life for which you have not yet found a solution and have no choice but to accept them. Furthermore, for each of them, write an attitude change that would lead to the appropriate acceptance. |
| 4- Assimilation of suffering and making meaning | (1) Shifting attention from suffering to meaning causes happiness, (2) addressing meanings leads to better assimilation of suffering, (3) experiencing suffering must lead to giving birth to thoughts, (4) the main suffering is the inability to have the correct perception of the present moment, (5) be patient in suffering in order to think more effectively | You might have been focusing on your suffering for a long time. It is better to shift your focus from suffering to somewhere else. Focus on the meanings of your life. Each of you must be able to extract your meanings and focus on them.List at least 20 meanings you feel relaxed and happy about by addressing them. |
| 5- Dhikr and meditation (mindfulness) | (1) Dhikr is like an anchor that makes the path of mindfulness possible, (2) regulating emotions by focusing on the dhikr and the present moment, (3) clarity of self-awareness by focusing on the present moment, (4) prayer is the best form of dhikr, meditation, (5) interpretation of allegory “The naked man and the bee” | According to the story “Abbas and his Mother” and the interpretation of an allegory of Rumi, achieve a correct understanding of the moment without judgment by focusing on the dhikr and the present moment and report in 10 lines. |
| 6- Death anxiety and making meaning | (1) Accepting and coping with anxiety related to illness and death, (2) meaningful reappraisal of death anxiety, (3) a developmental understanding of death anxiety, (4) death does not mean annihilation, (5) death is the secret of creation, (6) what has one not done that she/he would like to do for her/himself and others before dying? (7) interpretation of allegory “Conversation between Moses and God” | According to the story “Abbas and his Mother,” Abbas’s mother is dead, but she left a lasting impression on Abbas’s attitude and life, and Abbas always remembers her kindness. Try to analyze for yourself: What traces can I leave during hours, days, weeks, and months? What have I not done that I would like to do for myself and others before I die to be satisfied?So in 10 lines, try to report what you want to do before you die and do it with commitment. |
| 7- Patience and tolerance in suffering | (1) The main purpose of life is not to escape from suffering but to find meaning in suffering through patience, (2) in the path of patience, better thinking and self-control happens, (3) interpretation of allegory “Qazvini tattooing”, (4) interpretation of the story “Loghman and David” | You might have various physical, mental, and emotional problems and sufferings constantly occupying your attention. Be patient in the face of suffering and think about the meaning you get from it. Report what comes to your mind after thinking in 10 lines. |
| 8- Gratitude | (1) Gratitude, growth, and maturity, (2) the importance of gratitude to individuals, (3) gratitude to oneself, (4) gratitude to God and the universe, (5) interpretation of Rumi’s poems about gratitude | According to the interpretation of Rumi’s poems about gratitude, thank 10 individuals who have done something for you by accepting all the conditions. |
Summary of the Intervention
3.5. Ethical Considerations
The Ethics Committee of Mazandaran University of Medical Sciences approved the current study with the code IR.MAZUMS.REC.1399.428. Additionally, the IRCT code is IRCT20091220002898N13. The purpose of the study was explained to the participants, and informed consent was obtained from the participants. The anonymity and confidentiality of the data were ensured.
3.6. Data Analysis
The data were analyzed using repeated-measures one-way analysis of variance (ANOVA). Inferential statistical analyses were performed using SPSS software 25 (Statistical Package for Social Sciences Version 25).
4. Results
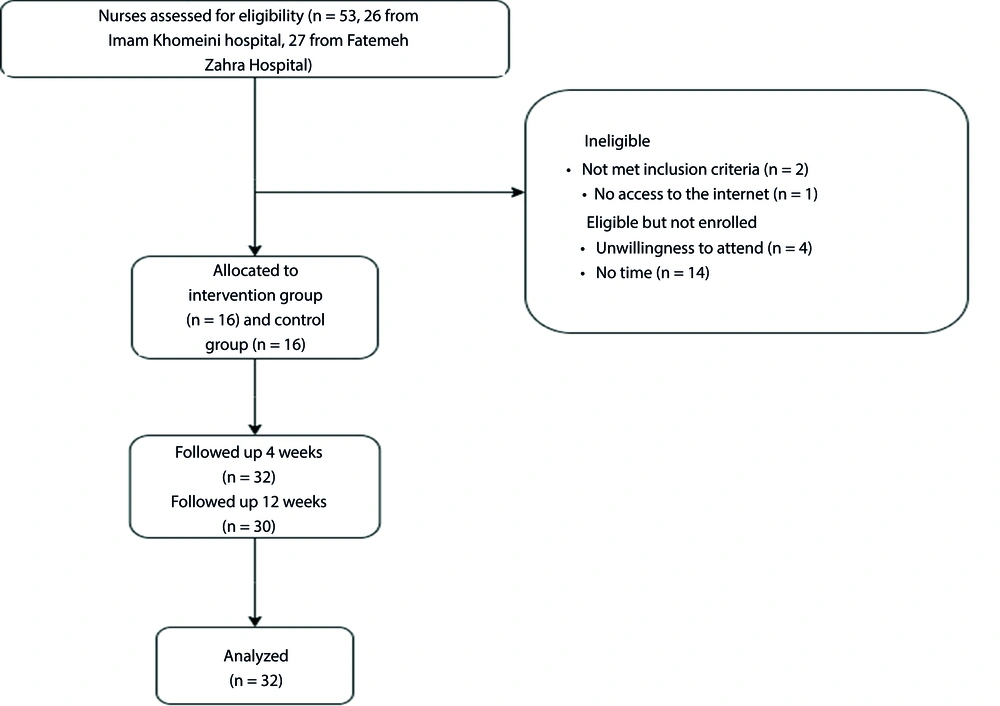
After screening 53 nurses, 32 (16 from Imam Khomeini Hospital and 16 from Fatemeh Zahra Hospital) were assigned to the intervention and control groups (Figure 1). Fourteen nurses were eligible but not enrolled due to their long working hours and lack of time. Most of the participants were 25 - 35 years (56.25%), female (84.37%), married (68.75%), and with an undergraduate educational level (81.25%), as shown in Table 2.
| Characteristics | Total (N = 32) | Intervention Group (n = 16) | Control Group (n = 16) |
|---|---|---|---|
| Age, y | |||
| 25 - 35 | 18 (56.25) | 6 (37.5) | 12 (75) |
| 36 - 45 | 12 (37.5) | 8 (50) | 4 (25) |
| > 45 | 2 (6.25) | 2 (12.5) | 0 (0) |
| Gender | |||
| Male | 5 (15.63) | 1 (6.25) | 4 (25) |
| Female | 27 (84.37) | 15 (93.75) | 12 (75) |
| Marriage | |||
| Married | 22 (68.75) | 12 (75) | 10 (62.5) |
| Unmarried | 10 (31.25) | 4 (25) | 6 (37.5) |
| Educational level | |||
| Undergraduate | 26 (81.25) | 13 (81.25) | 13 (81.25) |
| Postgraduate | 6 (18.75) | 3 (18.75) | 3 (18.75) |
Demographic Characteristics of Study Participants a
Table 3 shows the pre-test, post-test, and follow-up mean of anxiety, depression, and distress for the two groups. For the pre-test, post-test, and follow-up, a repeated-measures one-way ANOVA was employed to compare the mean scores from the control and intervention groups. As observed in Table 3, the results indicated an extremely significant difference in depression and anxiety at 4 and 12 weeks (P < 0.001). In the anxiety subscale, the results revealed a significant difference at 4 and 12 weeks (P = 0.011). In addition, there was a significant difference in the depression subscale at 4 and 12 weeks (P = 0.001). In contrast, the results showed no significant difference in distress at 4 and 12 weeks (P = 0.322).
| Outcome Measure | Total (n = 32) | Control Group (n = 16) | Intervention Group (n = 16) | P-Value | η2 | Correlation Among Repeated Measures (Effect Size [r]): Power | ||
|---|---|---|---|---|---|---|---|---|
| Interaction | Time | Group | ||||||
| HADS | ||||||||
| Anxiety | 0.634 (42): 0.99 | |||||||
| Baseline | 7.46 ± 3.49 | 7.46 ± 3.99 | 7.46 ± 3.04 | 0.011 | 0.484 | 0.152 | 0.149 | |
| 4 weeks | 6.80 ± 3.93 | 8.53 ± 4.01 | 5.06 ± 3.08 | |||||
| 12 weeks | 7.20 ± 3.90 | 8.06 ± 4.33 | 6.33 ± 3.35 | |||||
| Depression | 0.001 | 0.195 | 0.122 | 0.217 | ||||
| Baseline | 7.23 ± 3.69 | 6.80 ± 4.07 | 7.66 ± 3.35 | |||||
| 4 weeks | 6.00 ± 4.83 | 8.13 ± 5.44 | 3.86 ± 2.99 | |||||
| 12 weeks | 6.56 ± 4.51 | 8.00 ± 4.73 | 5.13 ± 3.92 | |||||
| Total | < 0.001 | 0.192 | 0.117 | 0.242 | ||||
| Baseline | 14.70 ± 6.63 | 14.26 ± 7.53 | 15.13 ± 5.84 | |||||
| 4 weeks | 12.80 ± 8.28 | 16.66 ± 8.80 | 8.93 ± 5.71 | |||||
| 12 weeks | 13.76 ± 7.75 | 16.06 ± 8.65 | 11.46 ± 6.19 | |||||
| IES-R | 0.322 | 0.298 | 0.254 | 0.040 | 0.780 (0.20): 0.95 | |||
| Baseline | 37.03 ± 17.23 | 38.66 ± 17.32 | 35.40 ± 17.60 | |||||
| 4 weeks | 34.46 ± 15.61 | 39.13 ± 15.94 | 29.80 ± 14.29 | |||||
| 12 weeks | 34.16 ± 16.60 | 37.53 ± 17.70 | 30.80 ± 15.28 | |||||
Differences in the Scores of Anxiety, Depression, and Distress Between Two Groups Based on Pre-test, Post-test, and Follow-up a
5. Discussion
The present study investigated the effectiveness of LBRT in anxiety, depression, and distress among frontline nurses during the COVID-19 pandemic. This study revealed that LBRT significantly reduced depression and anxiety in frontline nurses after the intervention and 2-month follow-up compared to those without intervention. However, distress in frontline nurses did not improve significantly after the intervention and 2-month follow-up, compared to the control group. Moreover, based on the verbal reports of the intervention group nurses, allegories and metaphors can facilitate transferring psychological concepts.
Some studies have highlighted considerations for incorporating culture in mental health interventions (38, 39). The present study is the first investigation to evaluate the effectiveness of culture-based intervention among nurses. This study showed that using the cultural model to care for nurses in critical situations improves their mental health. Logotherapy Based on Rumi’s Thoughts is based on Iranian culture, emphasizing spirituality, self-regulation, acceptance, assimilation of suffering and making meaning, patience in suffering, mindfulness, and gratitude (36).
Spirituality in LBRT is about finding the individual’s reason for being, why they are in the world, and discovering their mission. It also motivates us to make a valuable impact on the world. This spiritual perspective can be self-reinforcing for nurses under difficult situations. The purpose of spirituality in LBRT was for nurses to gain the awareness and acceptance of their responsibilities to stay in their jobs, not just moral responsibility and professional obligation holding them in this difficult situation. Spirituality negatively correlates with depression, anxiety, and distress (40-42). A study among nurses caring for cancer patients showed that spirituality negatively correlated with death anxiety and burnout (43). Spirituality has long been used to manage critical situations and stress (44). Spiritual interventions have been recommended during COVID-19 (45). A study demonstrated that spiritual growth in social isolation during COVID-19 was associated with lower anxiety, fear, sadness, and a higher level of hope (46).
Holzel et al. have shown that the components through which mindfulness meditation exerts its effects constitute a process of developed self-regulation (47). In particular, reappraisal is how emotions are regulated during mindfulness (47). Mindfulness and self-regulation are highly emphasized in LBRT. Through mindfulness, LBRT invited nurses to meaningfully reappraise surrounding phenomena in a way that has positive consequences. A review has shown that mindfulness meditation is an effective strategy for preventing and managing stress and burnout that often plagues nursing staff and students (48). Mindfulness-based stress reduction (MBSR) effectively reduces depression, anxiety, and stress when used with nursing students (49).
The culture in which the nurses of this study developed is rich in concepts of acceptance, assimilation of suffering, and making meaning. When there are activating events that have no immediate solutions and are beyond the control, accepting those situations can be helpful. A study has revealed that acceptance and commitment therapy reduced anxiety and depression in the staff of Razi Psychiatric Center, Iran (50). Additionally, patience in suffering and extracting meaning from it can help individuals take care of themselves and get through the crisis safely. Finding meaning in patience leads to cognitive reappraisal as an emotion regulation strategy (51). Some studies have shown that searching for meaning contributes to better adjustment in stressful events and reduces depression and distress (52, 53).
One of the intervention sessions was allocated to gratitude. In this study, nurses learned to recognize their abilities and values, make better judgments about themselves, and ultimately appreciate themselves. Studies showed that gratitude improves well-being and supports individuals against depression and stress (54-56). Moreover, it has negatively related to anxiety (57). Gratitude as a positive belief and attitude toward the self, world, and future is incompatible with Beck’s negative triad of depression (55). A study of Vietnam War veterans has demonstrated that individuals with PTSD showed significantly lower gratitude than those without PTSD (58). It suggested that interventions to increase gratitude have benefits for individuals with PTSD.
As shown, this study’s intervention did not have a significant effect on distress. The current study was conducted in the early days of the COVID-19 outbreak when the crisis was more acute due to being unknown. Although nurses in the intervention group were attempting to adjust to the existing conditions, they were constantly faced with a new situation in the COVID-19 pandemic that caused them new psychological distress. They could accept the existing conditions and reduce their depression and anxiety. However, because their information about the disease was limited, the emergence of any new variant of COVID-19 was worrying for them. With each unknown situation in the COVID-19 pandemic, distress reappeared, and nurses required time to adjust.
This study has several limitations. Firstly, the number of participants enrolled in the study was small due to the difficult conditions at the beginning of the COVID-19 period. It is possible that using a larger sample will have stronger effects. Secondly, this study had a higher proportion of women, which might limit the generalizability of the findings. Thirdly, this study included one intervention group. It is better to compare the effectiveness of LBRT to other intervention groups in nurses during the pandemic. Fourthly, the study was just carried out for 4 weeks. Due to the arduous situation, the long-term psychological consequences of this population are worth further investigation.
5.1. Conclusions
Rumi’s metaphors and allegories are very important in Iranian culture. Using Rumi’s metaphors and allegories, LBRT addresses some topics, such as spirituality, self-regulation, acceptance, assimilation of suffering and making meaning, patience in suffering, mindfulness, and gratitude. The Iranian culture is rich in such concepts. The results showed that LBRT was highly effective in improving anxiety and depression in frontline nurses during the COVID-19 pandemic. However, this intervention did not significantly affect the nurses’ distress during the COVID-19 crisis. Further studies should examine the effectiveness of culture-based interventions in critical situations.