1. Background
Access to healthcare pertains to how individuals can readily, conveniently, and affordably obtain essential medical and health services whenever required. This encompasses aspects such as establishing and outfitting medical facilities, medical equipment provision, and the availability of healthcare professionals (1). According to World Bank statistics, an estimated 3.5 billion individuals face inadequate healthcare access. Additionally, a minimum of 400 million people worldwide find themselves unable to avail essential healthcare services (2). In the span of 1990 to 2016, China witnessed a notable rise in its Healthcare Access and Quality (HAQ) index for healthcare accessibility and quality, ascending from 42.6 to 77.9. Despite the notable progress in both expanded care availability and enhanced service excellence, individuals with lower incomes continue to encounter the threat of overwhelming expenses following hospitalization. This phenomenon consequently diminishes the overall accessibility of the healthcare system (3, 4). Despite previous studies on people-oriented health service concepts, there has been a lack of research on developing measurement tools to evaluate the accessibility of health systems from a people-oriented perspective.
The Accessibility and Accommodation of Health Care Questionnaire, which is based on the development of health systems for urban and rural residents, and the Barriers to Care Scale, which is based on the development of health systems for military personnel, are commonly used to evaluate the accessibility of health systems (5, 6). While the scales mentioned earlier may have limitations, such as limited applicability to specific populations or the absence of comprehensive indicators, Penchansky and Thomas argue that access to healthcare can be assessed by examining the alignment between provider and customer characteristics and expectations. These key characteristics encompass availability, affordability, accessibility, accommodation, and acceptability. By considering these factors, researchers and policymakers can better understand healthcare accessibility and make informed decisions to improve it (7). Health service availability refers to the quantity and range of healthcare services provided by healthcare providers to meet the needs of patients. Affordability refers to the ability of patients to pay for healthcare services. Accessibility is defined as an individual's ability to access appropriate medical and healthcare services. Accommodation refers to the convenient distance between healthcare institutions and patients' homes. Acceptability means that healthcare providers will offer tailored medical services based on each patient's unique characteristics, the healthcare system's characteristics, and the level of health literacy awareness.
Hoseini Esfidarjani et al. from Iran designed and developed an application tool for assessing the accessibility of the healthcare system, known as the Perceived Access to Health Care Questionnaire (PAHCQ), in July 2021. The initial questionnaire was constructed based on the five dimensions outlined in Penchansky and Thomas' access model (1981), along with the inclusion of a sixth dimension introduced in Saurman's study. This questionnaire underwent validation for use within the Iranian population (8, 9).
Currently, there are limited research tools available for measuring the accessibility of health systems. Most of these tools focus solely on geographical and organizational dimensions or are limited to specific populations, overlooking important aspects such as adaptation, acceptability, and overall accessibility. For instance, the Barriers to Care Scale, developed by Canadian scholars, is specifically designed to assess the accessibility of healthcare services provided by the military. It is not applicable for evaluating the accessibility of healthcare services for the general population (6). On the other hand, the availability and accommodation of healthcare scale developed by Haggerty and Levesque primarily focuses on geographical convenience and accessibility, overlooking other crucial dimensions of accessibility (5). However, the introduction of the PAHCQ marks a significant milestone in this field. The PAHCQ is the first standardized and validated scale encompassing the five dimensions of access to care. By incorporating these dimensions, the PAHCQ offers substantial value in assessing the accessibility of healthcare services for the population. The instrument has demonstrated reliability and validity, unanimously recognized by experts. In terms of content validity, the instrument has been deemed valid. Additionally, the instrument has a Cronbach α value of 0.86, indicating high reliability. However, participants from different countries and regions may interpret the questionnaire differently due to language, context, and cultural environment differences. This can lead to biased evaluation results. To overcome cultural biases, it is recommended to use questionnaires in different language versions that are more suitable for the characteristics of the local population (10).
The current state of healthcare services in China exhibits regional imbalances, with certain areas falling short in both quantity and quality of medical and health services. These deficiencies fail to adequately address the growing and diverse medical needs of residents, resulting in particular challenges related to allocating healthcare professionals at the grassroots level. Moreover, the lack of effective coordination between supply and demand hampers the adaptability of primary healthcare services. China, as a nation characterized by the coexistence of multiple ethnic groups and a population distribution ranging from large urban centers to smaller settlements, faces additional complexity. Substantial differences in traditional cultures between the western and eastern regions contribute to disparities in the accessibility of primary healthcare services (11).
There is a scarcity of research focusing on healthcare accessibility within the field of healthcare services in China. However, considering factors such as the substantial growth of the urban migrant population, disparities in regional medical resources, and the necessity for tertiary hospitals to expand their capacity to accommodate a wider range of healthcare services, there is an urgent need for standardized assessment tools to gauge the perception of healthcare accessibility among the Chinese population. Such tools would enable the exploration of variations in the perception of healthcare accessibility across different regions in China. Ultimately, this research would aid in enhancing the coverage of medical services and promoting health literacy among residents in these regions.
2. Objectives
Considering the differences in economy, culture, social security, and healthcare system, it is still necessary to explore the applicability of the PAHCQ in the context of Chinese culture and healthcare environment. Therefore, we conducted the present study to translate and evaluate its psychometric properties.
3. Methods
3.1. Study Design
This was a cross-sectional study.
3.2. Population and Sample
The population of this study was residents in Jiangsu Province, China, who participated in physical examinations at tertiary hospitals from March to April 2023. Due to the concentration of comprehensive diagnosis and treatment services in tertiary hospitals in urban areas, there is a notable disparity in healthcare accessibility between rural and urban regions in China. Therefore, this study focused exclusively on urban populations to assess the accessibility of healthcare services through the questionnaire. By limiting the study to urban areas, the research aimed to specifically examine the accessibility of health services for urban populations, acknowledging the distinct characteristics and challenges of the urban health system. Based on the number of items in this research questionnaire and alpha of 0.05, a sample size of over 500 was required to detect at least 95% of the test efficacy (12). Therefore, based on the number of physical examinations conducted by 11 tertiary hospitals in this study and considering the response rate, the sample size to be selected for this study was 600. All participants' data underwent reliability analysis, construct validity, and known-group analysis. The inclusion criteria included: (1) 18 years of age or over; (2) permanent residents of the study sites (residence years greater than or equal to 3 years); and (3) outpatients participating in general physical examination. The exclusion criteria were previous mental health history and cognitive impairment. All participants signed an informed consent form.
A second evaluation was conducted two weeks after the initial assessment for test-retest reliability. Using the Minimize software, 300 subjects were randomly selected, and their scores were recorded during this second evaluation.
The procedure of selecting participants: The researchers organized the participants' information at the study site by arranging it in descending order according to their physical examination number, as well as the inclusion and exclusion criteria. Subsequently, researchers viewed the appointment numbers of the appointment experience personnel and selected the proposed participants through simple random sampling based on the order of the numbers. To select numbers for the sample, we used the random number table method to choose readings within the specified numerical range. We ensured we did not pick numbers outside this range and avoided selecting duplicates until we reached the predetermined sample size. The researcher explained the study's content, procedures, potential risks, and benefits to the participants. Furthermore, the participants were asked to provide informed consent, indicating their voluntary agreement to participate in the study.
3.3. Instruments
The PAHCQ consists of 30 items, each with a score of 5, rated on a Likert scale ranging from 1 to 5. The highest possible score for the PAHCQ is 150, including 20 for the accessibility subscale, 15 for the availability subscale, 45 for the acceptability subscale, 15 for the affordability subscale, 30 for the accommodation subscale, and 25 for the awareness subscale. A higher score indicates greater perceived access to health services. The researcher obtained a consent letter from the original scale developer and the open access license from the publishing institution (Creative Commons Attribution 4.0 International License).
3.4. Translation and Cross-cultural Adaptation
After obtaining permission from the original author and publishing agency, the translation and back-translation process, as well as the cultural adaptation of the PAHCQ, followed Brislin's guidelines (13). Two medical experts who were native Chinese speakers with good English proficiency independently translated the English version of the PAHCQ into simplified Chinese, producing Translations A1 and A2. Then, the translation coordinator, a Chinese individual who has studied in the United States and holds a degree in translation, compared the two translations and conducted a verification process to create Translation B. We invited 2 medical professors and 2 health management professors to read Translation B and asked them to provide their opinions on the items that lacked representativeness in the scale. Cultural adaptation was carried out on the scale, and the revised version of Translation C was formed. In cultural adaptation, translation mainly focused on whether the language expression of relevant items conformed to China's language customs and habits. The adaptation methods are based on five aspects: Content equivalence, technical equivalence, semantic equivalence, standard equivalence, and conceptual equivalence. At the same time, 2 native English-speaking physicians independently reverse-translated Translation C into English. A medical expert with experience studying abroad and proficiency in 2 languages compared the original text with its English translation, identifying any inconsistencies between the two. The researchers corrected the inappropriate aspects in Translation C and formed the final Chinese version of the translation.
The cross-cultural adaptation of the final version of the PAHCQ was conducted using pre-testing. To identify any potential ambiguities in the questionnaire items and wording, we conducted a pilot test as a predictive test involving 10 patients with chronic diseases and 10 healthy individuals. This pilot test aimed to assess the clarity and comprehension of the questionnaire items, ensuring that they were easily understandable and appropriately applicable to both groups. All participants in the prediction completed the questionnaire survey within 5 - 20 minutes. They reported no difficulties in linguistic appropriateness, semantic comprehension, and content acceptability of the PAHCQ. The questionnaire items and content were not changed after the prediction test.
3.5. Validation
3.5.1. Item Analysis
The total score correlation method and internal consistency test were used for item analysis. Pearson test was used to calculate the correlation coefficient (R) between the scores of each item and the total score. The larger the R-value, the more consistent the measurement attributes of the item and the total score table. An R value < 0.40 indicates a low correlation, 0.40 ≤ R ≤ 0.70 indicates a moderate correlation, and R > 0.70 indicates a high correlation. The criteria for deleting entries are R < 0.40 or without statistical significance (14). If there is a significant improvement in Cronbach's α coefficient of the total table after deleting a certain item, it is considered that the measured attributes of that item are different from the other items and should be considered for removal.
3.5.2. Reliability Analysis
We utilized Cronbach's α, Guttman's half coefficient, and the correlation coefficient between each item to assess the scale's internal consistency. If Cronbach's alpha value and Guttman half coefficient exceed 0.70, it indicates a high level of internal consistency reliability for the scale. The test-retest reliability coefficient > 0.75 indicates good tool stability (15).
3.5.3. Validity Analysis
3.5.3.1. Content Validity
The researchers invited 10 experts across the country [region: 4 from Henan Province, 4 from Shandong Province, and 2 from Sichuan Province; Title: 6 professors and 4 associate professors; Professional field (work direction): 4 experts in nursing, 4 experts in clinical medicine, 2 experts in social medicine and public health management]. They evaluated the content validity of the Chinese version of the PAHCQ. Each item is scored on a 4-point Likert scale, with values ranging from 1 to 4 for "irrelevant" to "highly relevant". We calculated the content validity index (I-CVI) at the item level, the content validity index (S-CVI) at the consensus scale level, the average S-CVI, and the probability of random consistency (Pc), and adjusted for Pc using I-CVI to obtain K *. When the number of experts participating in the evaluation is greater than 5, and the I-CVI is ≥ 0.78, it is considered that the content validity is good. The consensus S-CVI should not be less than 0.80, and the average S-CVI should reach 0.90. The evaluation criteria for K * are: 0.40 ~ 0.59 is average, 0.60 ~ 0.74 is good, and > 0.74 is excellent (16, 17).
3.5.3.2. Construct Validity
This study used exploratory factor analysis (EFA) to examine the underlying factor structure. The Kaiser-Meyer-Olkin (KMO) values were calculated to assess the sample adequacy, and the factor loadings of each item were examined to determine the necessity of removing any items deemed irrelevant. Moreover, the researchers conducted confirmatory factor analysis (CFA) and used the maximum likelihood method to fit the sample set data, using a series of model fitting indices to measure the degree of fit of the model. This study selected χ2/df, the goodness of fit index (GFI), adjusted goodness of fit index (AGFI), root mean square of approximation error (RMSEA), normalized fit index (NFI), relative fit index (RFI), value-added fit index (IFI), non-normalized fit index (TLI), comparative fit index (CFI), and other indicators to verify the rationality of the scale structure. If the theoretical model does not fit well with the observed data, it is necessary to make appropriate modifications to the model.
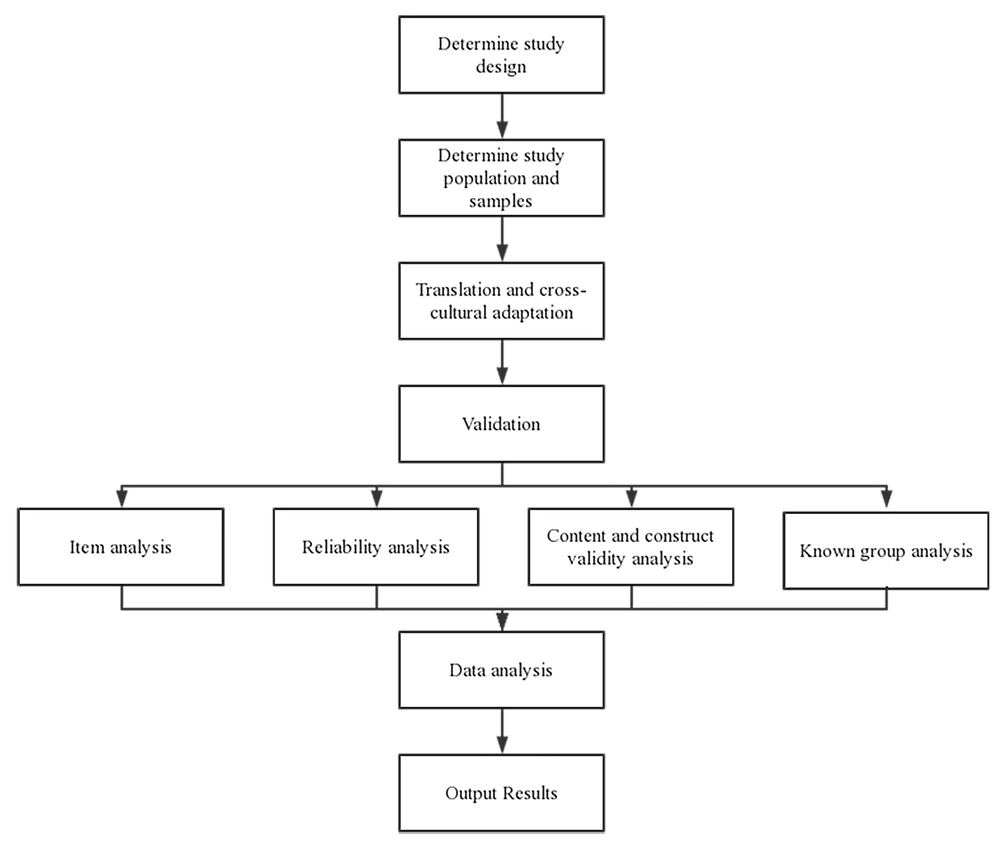
Known-group analysis: Two independent samples t-tests or one-way ANOVA were used to compare different groups of age, gender, marital status, education level, occupation, per capita monthly income, and Charlson comorbidity index (CCI). If the differences are statistically significant, it indicates that the Chinese version of the PAHCQ has the ability to distinguish patients with different characteristics in terms of perceived accessibility to the health system (Figure 1).
3.6. Data Analysis
All participants' data in the questionnaire were collected in Microsoft Office Excel 365. The quality of patient-reported outcome measures was evaluated by Consensus-based Standards for the selection of health measurement instruments (COSMIN) (18). Data of normal distribution are expressed as (
3.7. Ethical Considerations
This study was approved by the Institutional Review Board of the Faculty of Nursing, Mahidol University (IRB-NS2023/756.2202). All participants signed the informed consent form.
4. Results
4.1. Participant Characteristics
The researchers collected 591 valid survey questionnaires. The average age of 591 patients was 49.20 ± 12.17 years, of whom 77.8% were male. Also, 87.3% of the patients were married, and 63.6% were in liberal professions or students. More detailed information on demographic characteristics is provided in Table 1.
| Characteristics | No. (%) | Score | F (t) Value | P-Value |
|---|---|---|---|---|
| Age (y) | 6.22 | 0.002 | ||
| ≤ 44 | 253 (42.8) | 103.24 ± 18.82 | ||
| 45 - 59 | 200 (33.8) | 102.01 ± 21.26 | ||
| ≥ 60 | 138 (23.4) | 93.34 ± 23.29 | ||
| Mean ± SD | 49.20 ± 12.17 | 101.01 ± 20.97 | ||
| Gender | 1.31 | 0.025 | ||
| Male | 460 (77.8) | 101.73 ± 20.35 | ||
| Female | 131 (22.2) | 98.47 ± 22.94 | ||
| Marital status | 0.68 | 0.041 | ||
| Married | 516 (87.3) | 100.78 ± 21.23 | ||
| Unmarried, divorced, or widowed | 75 (12.7) | 102.61 ± 19.18 | ||
| Education level | 1.44 | 0.009 | ||
| High school or below | 458 (77.5) | 95.98 ± 22.17 | ||
| Bachelor's or college education | 123 (20.8) | 100.82 ± 20.63 | ||
| Master or above | 10 (1.7) | 104.19 ± 19.88 | ||
| Occupation | 1.17 | 0.118 | ||
| Government-affiliated institutions staff | 30 (5.1) | 104.19 ± 19.88 | ||
| Government staff | 56 (9.5) | 95.98 ± 22.17 | ||
| Enterprise unit staff | 74 (12.5) | 100.82 ± 20.63 | ||
| Liberal professions or students | 376 (63.6) | 93.10 ± 20.57 | ||
| Individual | 30 (5.1) | 97.50 ± 19.75 | ||
| Retire | 25 (4.2) | 98.84 ± 22.84 | ||
| Income (RMB) | 1.02 | 0.041 | ||
| < 5000 | 404 (68.4) | 100.99 ± 21.35 | ||
| 5000 - 10000 | 151 (25.5) | 102.84 ± 19.49 | ||
| 10001 - 15000 | 6 (1.0) | 74.00 ± 20.53 | ||
| > 15000 | 30 (5.1) | 97.50 ± 19.75 | ||
| CCI level | 3.33 | 0.037 | ||
| Mild (1 - 2) | 406 (68.7) | 103.01 ± 20.20 | ||
| Moderate (3 - 4) | 134 (22.7) | 97.33 ± 22.83 | ||
| Severe (≥ 5) | 51 (8.6) | 94.76 ± 19.70 |
4.2. Item Analysis
The total score of the Chinese version of the PAHCQ for 591 subjects was 101.01 ± 20.97. The highest score was 3.78 ± 1.04 on item 4, while the lowest was 2.75 ± 0.68 on item 10. The participants' scores were normally distributed with a ball shape. The correlation coefficients between each item's scores and the scale's total score were 0.66 ~ 0.84 (P < 0.001). After removing each item one by one, the Cronbach's α coefficient of the scale ranged from 0.95 to 0.96 (whole scale < 0.96), as shown in Table 2. Moreover, the percentage of the lowest or highest scores obtained by respondents from different dimensions was compared in this study. The analysis revealed that the lowest percentage for each dimension ranged from 2% to 9.3%, while the highest percentage ranged from 3.9% to 9.1%. These findings indicate the absence of floor or ceiling effects, suggesting that the questionnaire adequately captured the range of responses and did not excessively skew towards either extreme end of the scale.
| Items | Item Statistics ( | Cronbach's α Coefficient of the Scale After Deleting This Item | Item-Total Correlation (r) a |
|---|---|---|---|
| 1 | 3.72 ± 1.03 | 0.96 | 0.73 |
| 2 | 3.75 ± 1.01 | 0.96 | 0.76 |
| 3 | 3.74 ± 1.00 | 0.96 | 0.73 |
| 4 | 3.78 ± 1.04 | 0.96 | 0.73 |
| 5 | 3.68 ± 1.04 | 0.96 | 0.83 |
| 6 | 3.64 ± 1.00 | 0.96 | 0.83 |
| 7 | 3.57 ± 1.01 | 0.96 | 0.81 |
| 8 | 2.92 ± 0.65 | 0.96 | 0.71 |
| 9 | 2.77 ± 0.70 | 0.96 | 0.78 |
| 10 | 2.75 ± 0.68 | 0.96 | 0.72 |
| 11 | 2.80 ± 0.69 | 0.96 | 0.72 |
| 12 | 2.83 ± 0.67 | 0.96 | 0.68 |
| 13 | 2.79 ± 0.69 | 0.96 | 0.75 |
| 14 | 2.86 ± 0.67 | 0.96 | 0.66 |
| 15 | 2.83 ± 0.69 | 0.96 | 0.79 |
| 16 | 2.83 ± 0.69 | 0.96 | 0.70 |
| 17 | 3.63 ± 1.08 | 0.96 | 0.71 |
| 18 | 3.58 ± 1.07 | 0.96 | 0.75 |
| 19 | 3.55 ± 1.06 | 0.96 | 0.82 |
| 20 | 3.54 ± 1.13 | 0.96 | 0.78 |
| 21 | 3.42 ± 1.31 | 0.96 | 0.79 |
| 22 | 3.41 ± 1.34 | 0.96 | 0.66 |
| 23 | 3.46 ± 1.29 | 0.96 | 0.80 |
| 24 | 3.51 ± 1.30 | 0.96 | 0.81 |
| 25 | 3.52 ± 1.29 | 0.96 | 0.84 |
| 26 | 3.62 ± 1.27 | 0.96 | 0.82 |
| 27 | 3.62 ± 1.28 | 0.96 | 0.80 |
| 28 | 3.62 ± 1.23 | 0.96 | 0.84 |
| 29 | 3.58 ± 1.23 | 0.95 | 0.82 |
| 30 | 3.66 ± 1.20 | 0.96 | 0.82 |
| Total | 0.96 |
4.3. Reliability
The Cronbach's α coefficient of the Chinese version of the PAHCQ was 0.96 (95%CI: 0.953 - 0.963), the Guttman's half coefficient was 0.803, and the correlation coefficients between the items were 0.67 ~ 0.91. After excluding item 20 based on the CFA results, Cronbach's α coefficient of the Chinese version of the PAHCQ was 0.96 (95%CI: 0.951 - 0.961).
4.4. Content Validity
All 10 respondents gave positive feedback on the Chinese version of the PAHCQ, stating that the scale items were concise, the categories of options were clear, the overall scale was easy to understand, and there was no ambiguity. The I-CVI was 0.80 ~ 1.00, with an average S-CVI of 0.98, Pc of 0.01 ~ 0.04, and K* of 0.79 ~ 1.00.
4.5. Construct Validity
The results of the EFA analysis indicated a KMO value of 0.955, along with a statistically significant Bartlett's test of sphericity (P < 0.001). These findings suggest that the translated scale is well-suited for factor analysis, indicating the appropriateness of the data for further exploration of the underlying factor structure. This study extracted a total of 6 factors, with a cumulative variance contribution rate of 70.66%, as shown in Table 3.
| Factor Loading | Factor 1 (Accessibility) | Factor 2 (Availability) | Factor 3 (Acceptability) | Factor 4 (Affordability) | Factor 5 (Accommodation) | Factor 6 (Awareness) |
|---|---|---|---|---|---|---|
| 1 | 0.836 | |||||
| 2 | 0.829 | |||||
| 3 | 0.824 | |||||
| 4 | 0.821 | |||||
| 5 | 0.814 | |||||
| 6 | 0.811 | |||||
| 7 | 0.806 | |||||
| 8 | 0.800 | |||||
| 9 | 0.790 | |||||
| 10 | 0.783 | |||||
| 11 | 0.631 | |||||
| 12 | 0.812 | |||||
| 13 | 0.808 | |||||
| 14 | 0.802 | |||||
| 15 | 0.793 | |||||
| 16 | 0.777 | |||||
| 17 | 0.768 | |||||
| 18 | 0.757 | |||||
| 19 | 0.749 | |||||
| 20 | 0.538 | |||||
| 21 | 0.678 | |||||
| 22 | 0.835 | |||||
| 23 | 0.823 | |||||
| 24 | 0.815 | |||||
| 25 | 0.814 | |||||
| 26 | 0.813 | |||||
| 27 | 0.806 | |||||
| 28 | 0.799 | |||||
| 29 | 0.783 | |||||
| 30 | 0.782 |
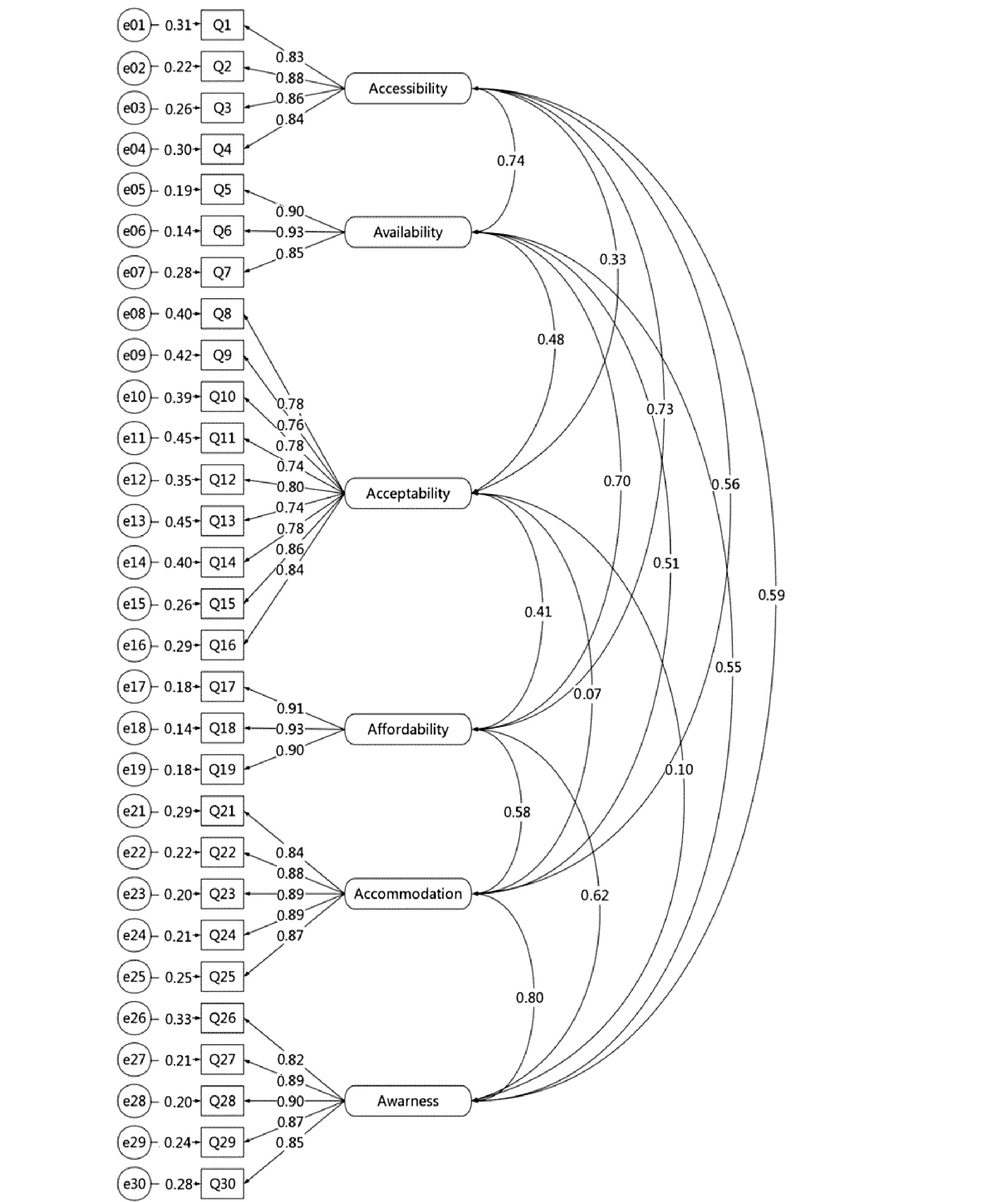
The results showed that the fitting indicators of Model 1 performed poorly with χ2/df = 4.05, GFI = 0.87, AGFI = 0.84, and RFI = 0.89. Due to the measurement variance value of 26.33 for item 20 in Model 1, we modified the model by deleting the item as prompted by the indicator. As a result, we established a standardized single-factor structural equation model (SEM) (Model 2) after making modifications. In Model 2, all fitting indicators were within an acceptable range (Table 4). Figure 2 shows the standardized regression coefficients, which are similar to the original questionnaire.
| Fit Indices | Model 1 Value | Model 2 Value | Reference |
|---|---|---|---|
| χ2/df | 4.05 | 2.39 | ≤ 3.00 |
| GFI | 0.87 | 0.92 | ≥ 0.90 |
| AGFI | 0.84 | 0.91 | ≥ 0.90 |
| RMSEA | 0.07 | 0.05 | ≤ 0.10 |
| NFI | 0.91 | 0.95 | ≥ 0.90 |
| RFI | 0.89 | 0.94 | ≥ 0.90 |
| IFI | 0.93 | 0.97 | ≥ 0.90 |
| TLI | 0.92 | 0.96 | ≥ 0.90 |
| CFI | 0.93 | 0.97 | ≥ 0.90 |
4.6. Known-Group Analysis
Comparison of the total PAHCQ scores among patients in different groups of age, gender, maternal status, education level, per capita monthly income, and CCI levels showed statistically significant differences (P < 0.05), as shown in Table 1.
5. Discussion
The PAHCQ has been proven to comprehensively, quickly, and accurately assess patients' perceptions of the accessibility of the health system. In addition, the PAHCQ can also be used to evaluate the views of populations based on multi-level accessibility, availability, acceptance, affordability, accommodation, and awareness of accessing health services (19). This result indicates that the Chinese version of the PAHCQ is easily accepted by Chinese patients and demonstrates good validation in the construction and identification of the Chinese version of the PAHCQ.
Our translation process followed the guidelines of Brislin's translation model (13), and the validation study was conducted under the guidance of COSMIN (18). Therefore, the research process followed the scientific translation validation and research population screening process. The Brislin classic backtracking model applied in this study continuously compares the source language translation with the original text through backtracking, maximizing the semantic equivalence of the measurement tool. To ensure translation quality, emphasis has been placed on "back translation" and "blind translation" in the translation structure. This measure avoids the impact of memory bias and expected perspectives on translation quality (19, 20). This model is also frequently applied to the design and psychometric properties of other Chinese versions of medical scales (21, 22).
The CFA can assess the ability of models with pre-defined factors to fit actual data, assess whether the data matches the expected theory, and facilitate a clearer analysis of the basic content and structure of the scale (23). Our CFA results indicate that the original structure of the PAHCQ is appropriate. However, the scores are still lower than those of the original questionnaire (χ2/df = 1.15, RMSEA = 0.02) but comparable to the Arabic version of PAHCQ (24). As the scale used in this study is relatively new, there has been limited validation of its various language versions. However, several scales addressing patient satisfaction include dimensions related to the accessibility of the healthcare system. In two separate validations of the Chinese version of patient satisfaction questionnaires, the results of CFA regarding the accessibility of the health system align with the findings of this study (25, 26). This consistency further supports the validity and reliability of the accessibility dimension in the scale used. In the Chinese version of the PAHCQ, item 20, "It is easy to make an appointment at a health center," shows poor fitting performance, so we removed this item. The possible reason is that patients at our study site tend to prefer the queue system over the appointment system, and in fact, the queue system is also more commonly used in medical institutions at the study site. Effectively, due to the huge number of patients and the higher level of service demand in China's large, well-known tertiary hospitals, outpatient services are mostly registered through the appointment system. However, for tertiary and lower-level hospitals in ordinary prefecture-level cities, considering the differences in the number of residents, residents' education levels, and medical costs, hospitals often prefer the queuing system (27).
The results of the known-group analysis indicate that the Chinese version of the PAHCQ can distinguish the ability of patients in different groups of age, gender, material status, education level, per capita monthly income, and CCI levels to perceive the accessibility of the health system, which plays an important role in expanding the application scope of this questionnaire in different population groups. Moreover, the study of the English version of the PAHCQ in the American population also mentioned the scalability of the questionnaire in different populations (28). The perception of healthcare accessibility plays a crucial role as an essential aspect of the social determinants of health. According to the WHO's Social Determinants of Health Model, certain structural determinants such as age, gender, marital status, education level, and income can influence the accessibility of the healthcare system. These structural determinants, in turn, can impact mediating factors such as the Charlson Comorbidity Index (CCI), subsequently affecting overall well-being (29). The accessibility of the healthcare system can also influence environmental, biological, behavioral, and psychological factors among residents. Therefore, conducting group analyses using the PAHCQ can enhance its applicability in studies that explore the relationship between social determinants of health and healthcare accessibility.
Reliability reflects the stability, repeatability, and inherent consistency of the evaluation tool (30). The greater the reliability, the smaller the measurement standard error. It is generally considered that Cronbach's α coefficient > 0.70 and test-retest reliability > 0.80 indicate good scale reliability. In this study, the reliability test showed that the Cronbach alpha value was 0.96, and the test-retest reliability value was 0.83, indicating that the PAHCQ has good internal consistency. Therefore, these entries can consistently and accurately reflect patients' perceptions of the accessibility of the health system.
The scale's length and language are crucial for special groups to complete the questionnaire, especially for the elderly with limited understanding and cognitive ability (31). When applying this questionnaire to the elderly participants, there is a significant difference in the feedback time compared to the young participants, and some of them declared fatigue when answering. Therefore, further studies may consider the communication characteristics, language habits, reading and writing abilities, and cognitive abilities of the elderly population and develop a simpler version of PAHCQ.
Perception of accessibility to health systems is a dynamic process (32). Therefore, further researchers should understand the level of accessibility awareness of people of different ages to the health system, which will help enrich the connotation of accessibility of the health system, strengthen the research on accessibility awareness mechanism of the health system, and provide a corresponding theoretical framework for intervention studies.
Some limitations need to be addressed. This study only used the research population from Jiangsu Province, China, with certain regional limitations. The representativeness of the population needs to be improved, and the universality of the research results needs to be further verified. Considering that China is a large country with multiple ethnic groups in large mixed residences and small settlements, it is recommended to use a random sampling method for multi-level and multicenter research to improve the reliability and applicability of the scale evaluation. Besides, 77.5% of the respondents in this study had a high school education or below, and the age group was relatively older. Further research is needed on a larger sample that includes more young and highly educated individuals. Furthermore, it is important to note that the participants in this study were individuals who underwent physical examinations at urban tertiary hospitals. In future studies, it would be valuable to explore the applicability of the questionnaire to rural populations and examine the effectiveness of the PAHCQ in assessing the accessibility of healthcare services in those areas.
5.1. Conclusions
The Chinese version of the PAHCQ demonstrates good psychometric performance within the Chinese culture and healthcare environment. It also demonstrates equivalence to the original version regarding semantics, concepts, idioms, and content. It is an easy-to-use questionnaire and a reliable, effective, and feasible screening tool for evaluating patients' perceived accessibility to the health system, which may have high utility in the evolving Chinese health system.